Tularaemia 2013-2024
Tularaemia in humans in Denmark, 2013–2024
Tularaemia, also known as rabbit fever, has in the past decade been detected in all regions of Denmark. Although the number of cases remains relatively low, an increasing trend has been observed in recent years.
Key findings
- During the period 2013–2024, 109 people were diagnosed with tularaemia in Denmark. This corresponds to 0.2 cases per 100,000 inhabitants per year.
- In 2024, 28 people were diagnosed with tularaemia; the highest annual number of cases in the period, followed by 2023 with 17 diagnosed cases.
- Tularaemia was detected more frequently in men and among individuals aged 40–49 years.
- Cases were recorded in all regions during 2013–2024, and the disease is considered endemic in Denmark.
- Bornholm had the highest average annual incidence with 1.9 cases per 100,000 inhabitants per year, while North Zealand recorded the highest total number of cases with 28 in total (an incidence of 0.5 cases per 100,000 inhabitants per year).
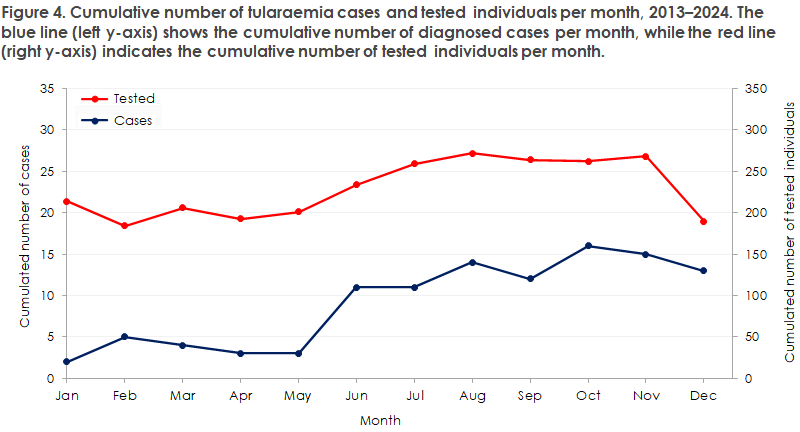
- Tularaemia cases typically occurred between June and December each year.
- Since November 2023, tularaemia has been subject to mandatory laboratory notification, and submission of Francisella tularensis isolates from primary clinical laboratories to Statens Serum Institut has also been mandatory since then.
Introduction
Tularaemia, also known as rabbit fever, is an infectious disease caused by the bacterium Francisella tularensis. The disease typically manifests acutely with high fever and swollen lymph nodes, with or without specific symptoms. These symptoms, which vary depending on the route of infection, define the clinical form of the disease: ulceroglandular, glandular, oculoglandular, oropharyngeal, pulmonary, or typhoidal form. The disease is endemic in the Northern Hemisphere and has in recent years been detected in all regions of Denmark. In Europe, the subspecies F. tularensis subsp. holarctica (Type B) is found, which generally causes a milder disease compared with F. tularensis subsp. tularensis (Type A), the more virulent subspecies occurring in North America.
F. tularensis is found primarily in natural environments with lakes and streams. Humans are infected mainly through bites or stings from vectors (mosquitoes, ticks, flies), through contact with infected animals or their blood (especially during hunting), through ingestion of contaminated drinking water or insufficiently cooked game meat, or through inhalation of dust contaminated with the bacterium.
Surveillance
Since November 2023, tularaemia has been a laboratory-notifiable disease in Denmark. At the same time, it became mandatory for laboratories to submit isolates of F. tularensis, as well as primary samples in which the bacterium has been detected and material considered cultured, to Statens Serum Institut (SSI) according to current guidelines. As a result of mandatory laboratory notification, data on diagnosed tularaemia cases in Denmark are now systematically collected, analysed, and interpreted based on information from the Danish Microbiology Database (MiBa), which is cross-checked with SSI’s laboratory records.
Before the order came into force, laboratories could voluntarily submit isolates to SSI for confirmation of identification and antimicrobial susceptibility testing. Previous estimates of the occurrence of tularaemia were based on review of these clinical samples submitted to SSI. However, specific analyses – i.e. serology, PCR, and culture for F. tularensis – have always been centralised at SSI.
Despite recent improvements in the national surveillance system, tularaemia may still be underdiagnosed.
This report constitutes the first consolidated epidemiological overview of tularaemia cases in Denmark recorded at SSI. It covers data from 2013 to 2024 and presents information on the number of cases; in total and per 100,000 inhabitants, age and sex distribution, as well as seasonal patterns. For further information on clinical manifestations, genotypic characterisation, diagnostic methods, notification procedures, prevention, and tularaemia in Denmark in 2025, see EPI-NYT 49b/2025.
Methods
This report includes confirmed cases of tularaemia with sample dates between 1 January 2013 and 31 December 2024, diagnosed at a Danish laboratory regardless of country of residence. The presented data are based on MiBa and cross-checked with SSI’s laboratory registers.
A case of tularaemia is considered confirmed if at least one of the following criteria is met:
• Francisella tularensis is isolated from a clinical sample, or
• Francisella tularensis nucleic acid is detected in a clinical sample, or
• a specific antibody response against Francisella tularensis is detected with a titre ≥1:100, or a titre of 1:10, 1:25 or 1:50 followed by a positive test.
A disease episode was defined using a six-month time window such that multiple positive test results from the same person were considered part of one episode if they occurred within six months of each other. Positive samples more than six months after a previous episode are classified as a new episode if confirmed by molecular or culture-based methods, or if serological testing showed a higher antibody titre compared with the previous episode.
It is not possible based on the current surveillance system to determine where the tularaemia infection was acquired. Therefore, in this report, the patient’s place of residence is used as a proxy for the geographical location of infection, but this does not necessarily reflect the actual place of exposure. This limitation should be considered when interpreting the geographical distribution of cases.
Results
Between 2013 and 2024, a total of 109 cases of tularaemia in humans were diagnosed in Denmark. The annual number of cases remained below 10 until 2018. From 2019 onwards, the number generally increased, though with a temporary decline in 2021 and 2022, before reaching a peak in 2024, when 28 cases were recorded, Figure 1. No recurrent infections with tularaemia were detected during the period.
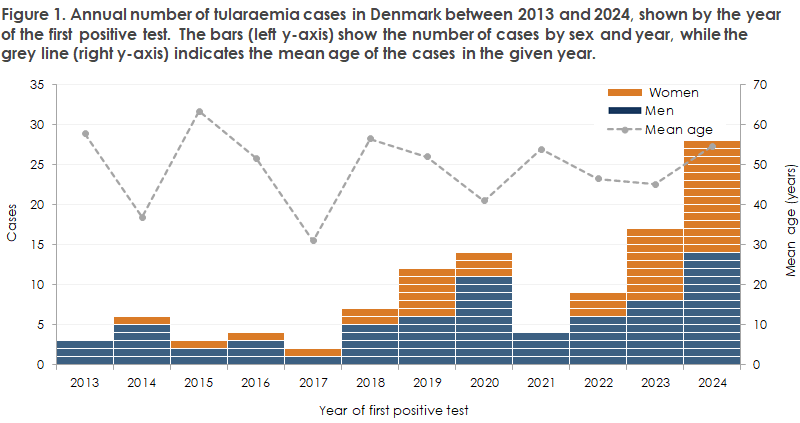
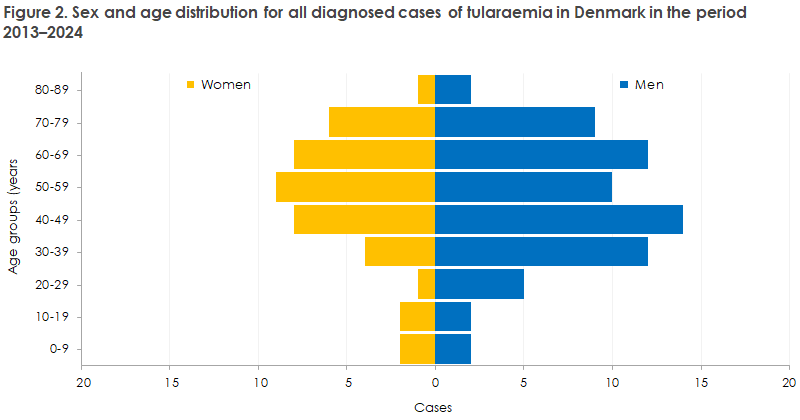
Tularaemia was diagnosed in persons aged 1 to 80 years. The average age was 50 years (median 52 years) for women and 49 years (median 47 years) for men across the entire period. The average age varied between years, as shown in Figure 1, ranging from 31 to 63 years. Approximately 62% (68/109) of cases occurred among men. About one-fifth (22/109) of all cases were in the 40–49-year age group, followed by the 60–69-year group with 20 cases and the 50–59-year group with 19 cases, Figure 2. Among women, the latter age group accounted for the largest share of cases, with nine out of 41 (22%) diagnosed in this group.
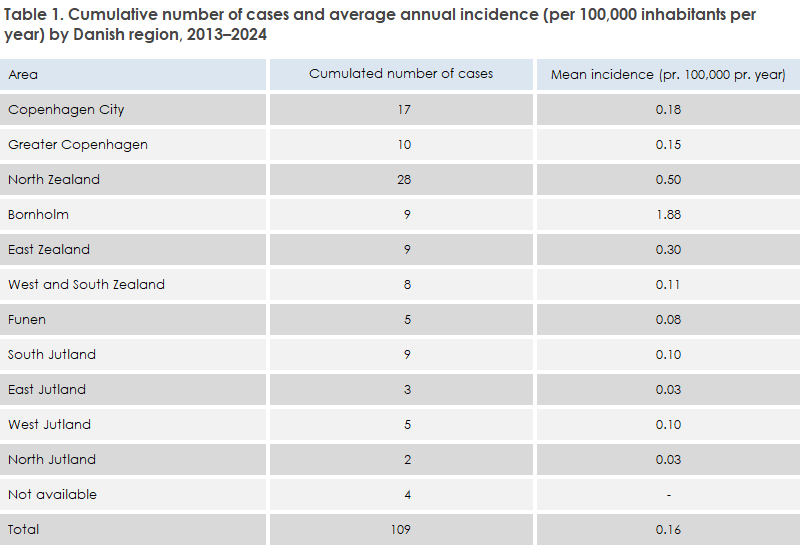
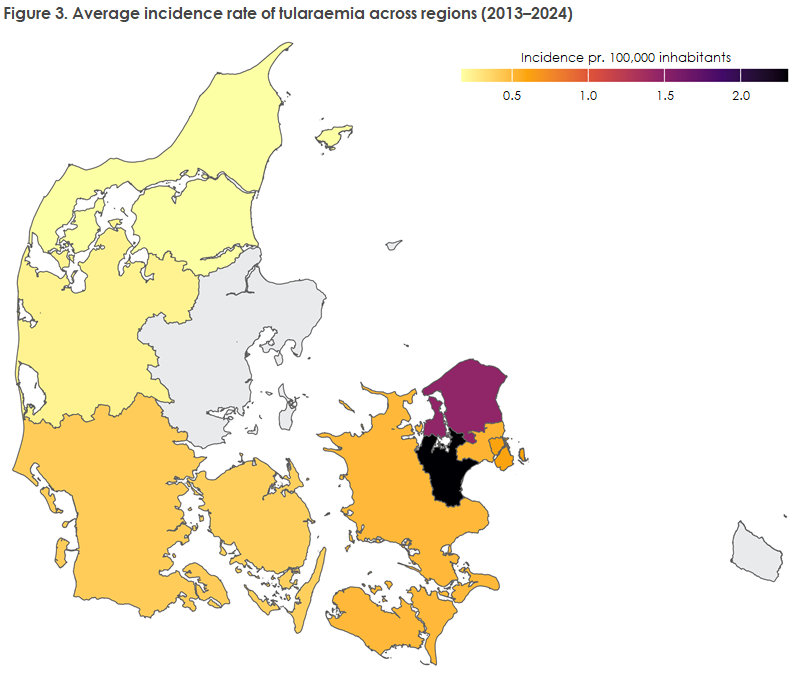
In addition to demographic differences, the geographical distribution of tularaemia cases also varied across regions and over time. Incidence was generally low in most regions, mostly below 1.0 per 100,000 inhabitants. On Bornholm, the average incidence was 1.9 per 100,000 inhabitants per year, Figure 3, corresponding to nine cases in total during the period. North Zealand accounted for the largest proportion of episodes with 28 cases in total (26% of the national total for the period), corresponding to 0.5 cases of tularaemia per 100,000 inhabitants per year, Table 1.
However, as mentioned above, it should be noted that the geographical indicators in this report refer to the patients’ place of residence, which does not necessarily correspond to the actual region of exposure.
A clear seasonal pattern was observed in the number of cases and in the number of tested individuals. The number of cases was low in winter and spring months, but increased markedly between June and October, indicating that the tularaemia season begins in summer and continues towards the end of the year, Figure 4. The number of tested individuals follows a similar pattern and increases in the same period. The person-based positivity rate ranged from 0.9% to 2.7% in January to May, after which it increased from June to December to values between 4.3% and 6.8%.
This annual report is also mentioned in EPI-NYT 49b/2025.