Mycoplasma genitalium 2024
Mycoplasma genitalium – surveillance of incidence and antibiotic resistance, 2024
Data from the Danish Microbiology Database MiBa
Mycoplasma genitalium (MG) incidence and macrolide-resistance data for this report were, as in previous years, obtained from the Danish Microbiology Database MiBa. This report presents data from 2024 on positive rates, incidence and antibiotic resistance related to macrolides and quinolones.
Data for quinolone resistance mutations are based on randomly selected samples among specimens submitted for MG testing at the SSI. This report covers samples from January to December 2024 and builds on the MG report published in 2024.
A disease episode is defined as the first positive test result within a 42-day period. Negative episodes are defined within the same timeframe, corresponding to the disease definition used for chlamydia (2024). The data analysis is based on disease episodes and is therefore independent of the number of samples per patient, within an episode.
This report includes data on demographic factors such as age, sex and region, as well as positive and negative test results, including detection of genetic markers for macrolide resistance. For patients with a valid personal identification number, information on sex, age and municipality code as well as region is obtained via the CPR register. Incidence or positive rates are indicated here. Not all tested individuals have a valid personal identification number or information on sex, age or region, which may lead to small differences in positive rates in the following tables.
Incidence of MG
In 2024, 37,499 episodes were tested for MG, representing a 10.6% decrease from 2023 (41,956), Table 1. Although there was a reduction in the number of test episodes in 2024, the positive rate remained unchanged. A total of 4,352 positive episodes were found in 2024 (positive rate 11.6%) compared with 4,972 positive episodes in 2023 (positive rate 11.9%). In 2024, positive episodes were distributed across 1,783 men (positive rate 14.7%) and 2,569 women (positive rate 10.1%).
Since 2011, the positive rate of MG has increased from 6.1% to 11.6% (p<0.001). This contrasts with the trend for chlamydia, and since 2020 the MG positive rate has been higher than that of chlamydia in Denmark, Table 1, Chlamydia report 2024.

Age and sex distribution of MG cases
Table 2 shows the number of MG episodes, incidence per 100,000 inhabitants, number of test episodes per 100,000 inhabitants and positive rate, by age groups among men (Table 2a) and women (Table 2b) in 2023 and 2024. The majority of cases continued to be observed among 20–24-year-olds for both sexes, and there was an overrepresentation of women aged 15–24 years compared with men. Among persons over 35 years, a slightly higher number of cases were observed among men than among women, Table 2. A small decline in both the number of episodes and incidence was observed for both sexes across almost all age groups from 2023 to 2024, except for women aged 30–34 and men aged 35–39 and 45–49, where small increases were observed.
As in 2023, the highest positive rate was seen among 20–24-year-olds for both men and women, with a positive rate of 21.9% for men and 14.7% for women in 2024, Table 2a & 2b, whereas the highest positive rate for chlamydia in 2024 continued to be seen in the 15–19-year age group regardless of sex Surveillance report 2024. In 2024, 24-year-old men (25 years in 2023) and 22-year-old women (22 years in 2023) had the highest MG incidence at 366 and 642 per 100,000 inhabitants, respectively. Compared with chlamydia in 2024, the highest incidence among women was seen in 19-year-olds and among men in 20-year-olds, which may indicate that chlamydia affects a younger age group than MG, Chlamydia surveillance report 2024.
In both 2023 and 2024, the majority of MG episodes were registered in the 15-29-year-old age group, comprising 75% of all episodes in 2023 (67.2% and 80.3% among men and women, respectively) and 72.4% in 2024 (65.1% and 77.4% among men and women, respectively). Compared with chlamydia, the proportion of cases in this age group was slightly lower for MG, as the proportion for chlamydia was 80.9% (75% among men and 86.8% among women) in 2024.
Overall, a decrease was observed in both, incidence per 100,000 inhabitants and positive rate from 2023 to 2024 for both, men and women, Table 2a. This may be due to a decline in test activity between the two years, Table 2a & 2b, although the difference is not significant. Overall, a higher incidence per 100,000 inhabitants and a lower positive rate were seen among women in both, 2024 and 2023, with incidences of 86 and 60 per 100,000 among women and men respectively in 2024, Table 2a & 2b, and positive rates of 10.1% and 14.7% among women and men respectively. The lower positive rate and higher incidence among women can be explained by more than double the test activity per 100,000 inhabitants (846 tests per 100,000 inhabitants among women compared with 410 tests per 100,000 among men, Table 2a & 2b).



Geographical distribution
The highest test activity was observed in Copenhagen City and Greater Copenhagen suburbs for both sexes. The number of test episodes per 100,000 inhabitants was 1,460 and 521 among men, and 2,889 and 1,183 among women in 2024. The same trend was observed in 2023 and previous years, Table 3. Across the regions, a higher MG incidence among women than men was again observed in 2024, with the male/female (M/F) ratio remaining virtually unchanged from 2023 to 2024 for all regions and nationwide. The lowest M/F ratio was observed in East Zealand and the highest on Bornholm, followed by East Jutland, Table 3.
Particularly in Copenhagen City, a decline was seen in both test episodes and diagnosed cases for both sexes, where the incidence rate of test episodes per 100,000 inhabitants decreased from 1,575 to 1,460 and from 3,646 to 2,889 for men and women, respectively, Table 3. Despite the lower test activity, a simultaneous decrease in positive rate was seen for men and women from 15.2% to 13.9% and from 9.7% to 9.6%, respectively. The number of tests per 100,000 inhabitants was largely unchanged in the remaining regions, although an overall decline in both test activity for both sexes and positive rate among men was seen nationwide from 2023 to 2024, particularly from 409 to 402 test episodes per 100,000 (positive rate from 16.5% to 14.8%) among men, and from 1,004 to 839 test episodes per 100,000 (positive rate from 10% to 10.2%) among women, Table 3.
By comparison, the number of test episodes and positive rate of laboratory-verified chlamydia cases decreased for both sexes from 2023 to 2024 nationwide (3,872 test episodes per 100,000 in 2023 and 3,683 per 100,000 in 2024 among men, and 8,798 test episodes per 100,000 in 2023 to 7,979 per 100,000 in 2024 among women) Chlamydia surveillance report 2024.

Treatment and development of antibiotic resistance
The Danish treatment recommendation (MG surveillance report) is based on the European guidelines from IUSTI (International Union against Sexually Transmitted Infections) and supported by WHO and ECDC (European Centre for Disease Prevention and Control). Treatment is complicated by antibiotic resistance to macrolides and quinolones, and the guidelines recommend that macrolide-resistance mutation (MRM) data be available before treatment of MG infections. Testing for quinolone-resistance associated mutations (QRAM) should not be performed unless treatment with moxifloxacin has failed, and quinolone-resistance testing is currently only performed at SSI.
Macrolide resistance
Compared with 2023, no change was observed in macrolide resistance rates by sex or age, Table 4. In 2023 the resistance rate was 63% among women and 65% among men, while in 2024 a resistance rate of 65% was seen among both women and men. The highest resistance rates were seen among 15-24-year-olds for both sexes in both years, Table 4 & Figure 2.
The highest resistance rate was seen in the 15-19-year age group for both sexes in both years. In 2024 the resistance rate was 75% among 15-19-year-old men (72% in 2023) and 72% among 15-19-year-old women (71% in 2023).


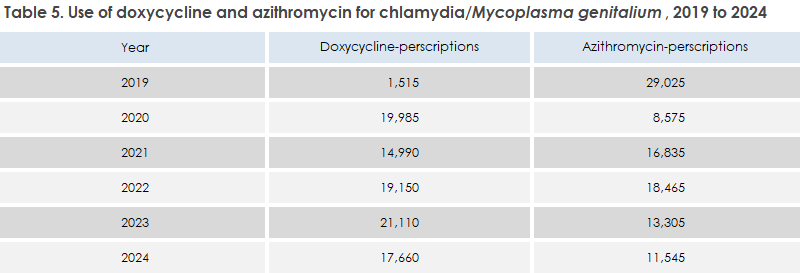
There is a clear association between chlamydia treatment with azithromycin and macrolide resistance in MG, as macrolide resistance is easily selected in cases of concurrent MG infection. In EPI-NEWS 38/2018, the SSI recommended that first-line treatment for uncomplicated chlamydia be changed from single-dose azithromycin to a 7-day doxycycline regimen to improve treatment of rectal chlamydia and reduce resistance development in MG. Since then, a decline has been seen in azithromycin use (from 29,025 prescriptions for chlamydia/MG in 2019 to 11,545 in 2024) and an increase in doxycycline use (from 1,515 prescriptions in 2019 to 17,660 prescriptions for chlamydia/MG in 2024), Table 5. A study published in the annual DANMAP report (2024) showed that MG patients with recent chlamydia infection have significantly higher macrolide resistance rates (76%) than patients with previous or no chlamydia infection (66% and 56% macrolide resistance, respectively). Data from the Prescription Registry show that azithromycin continued to be prescribed for around 60% of chlamydia treatments in 2024. This proportion should be further reduced.
Quinolone resistance-associated mutations
Between 2018 and 2024, sample-based detection of quinolone resistance-associated mutations (QRAM) has been performed for a total of 2,120 MG-positive patients. Overall, a non-significant increase in total quinolone resistance was observed for both sexes from 6.3% in 2023 to 7.2% in 2024 (p=0.7), Figure 3. QRAM are detected more frequently in men, although the difference is not significant. The quinolone resistance rate increased among women from 2023 to 2024 (5.2% to 6.9%, p=0.5), Figure 3. During the same period, a non-significant increase was observed in dual-resistance rates, i.e., samples with both macrolide and quinolone resistance mutations, from 5.8% in 2023 to 6.8% in 2024.
In 2024, the mutation types S83I and D87N continued to be the most frequently observed, consistent with previous findings.

This report is also mentioned in EPI-NEWS 48/2025.