Legionnaires' Disease in Denmark 2024
Legionnaires’ Disease in Denmark 2024
In 2024, a total of 296 cases of Legionnaires’ disease (LD) were reported among residents in Denmark (Table 1). Of these, 180 were men (aged 24–100 years, median age 70) and 116 were women (aged 33–101 years, median age 71.5). Among all LD cases, 29 (9.8%) died—17 men (9.4%) and 12 women (10.3%)—within 30 days after onset of illness or hospitalization. Mortality was thus at the same level as before the COVID-19 pandemic, see the 2023 annual report.

The proportion of elderly ≥70 years with LD remains high (53.4%), though declining since 2022. Mortality in this age group is also falling, reaching 15.6% in 2024.
The proportion of travel-associated cases abroad was unchanged compared to 2023 and the pre-COVID period, with 56 cases (18.9%). These cases had very low mortality (0%) and were relatively young (Table 1). As usual, there were about twice as many men (38) as women (18)—a ratio of 2.1:1—whereas the gender distribution among persons infected in Denmark was more balanced (1.4:1).
Infection in Denmark
In total, 240 of the registered disease cases in 2024 (81.1%) are assumed to have been infected in Denmark (Table 1 and 2), where the unknown category is included. This represents a slight decrease compared with the previous four years (Table 2).
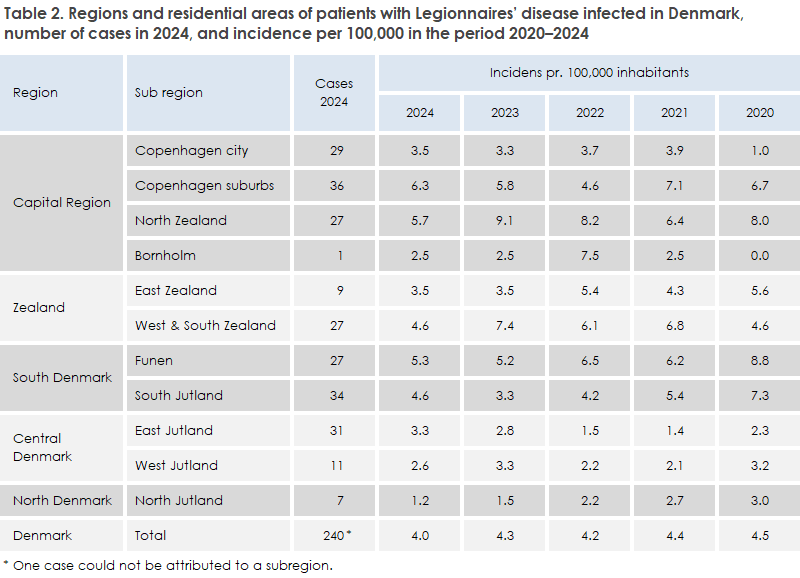
The overall geographical distribution in 2024 (Table 2) was roughly the same as in 2023. However, North Zealand showed a marked decrease—from 43 to 27 cases—and here a relatively high proportion of patients were infected with Legionella non-pneumophila (seven cases; 25.9%), including three with L. longbeachae (see section on laboratory-confirmed cases). North Jutland had the lowest incidence in the country in 2024, at only 1.2 cases per 100,000 inhabitants.
Community-acquired infection in Denmark
Of 184 community-acquired cases (Table 1), 83 were culture-confirmed (45.1%). Among these, 38 (45.8%) were L. pneumophila serogroup 1 (SG1)—23 Pontiac and 15 non-Pontiac. Another 24 patients had SG3 (28.9%). Others included 13 culture-confirmed with different serogroups, six with L. longbeachae, and two with L. bozemanae.
SSI received water samples in 54 cases, of which 50 tested positive for L. pneumophila. For seven patients diagnosed with L. longbeachae, soil and gardening products were examined—five of six tested positive. In 14 of 24 culture-confirmed L. pneumophila cases, a match was found between patient isolates and domestic hot-water systems, though only with less virulent types (SG1 OLDA/Oxford, SG3, SG6). Overall, the source could only be verified in 19 of 61 investigated cases.
Only one small Danish cluster was detected in 2024, consisting of two cases of SG3, ST1005, from the same apartment complex. Four further cases were part of longer-term clusters dating back to 2021.
Travel-related infection in Denmark
Seven persons were probably infected while traveling domestically—five at hotels and two at campsites. Two were linked to a hotel with cases dating back to 2021. Five of the seven were urine-test positive; two were culture-confirmed with L. pneumophila SG1 Pontiac.
Institution- and Hospital-Acquired Infections in Denmark
A total of 37 cases were reported with suspected or confirmed infection acquired from healthcare institutions: nine from hospitals and 28 from other institutions such as nursing homes. One hospital and two nursing homes were each associated with two cases. In total, eight of these cases were confirmed by culture: two with L. pneumophila SG1 (non-Pontiac) and six with other serogroups (3, 5, and 10). The remaining cases were diagnosed exclusively by other methods. SSI is aware that water samples were examined from 20 of the institutions/hospitals. A match between patient and institution was demonstrated for two hospitals and two nursing homes – but water samples from all institutions and hospitals were positive for L. pneumophila.
Travel-Associated Infections
Travel-related cases (abroad) occurred in all months except February. Most travel cases were recorded from July to October – a total of 34 cases (67.9 %), with an average of 8.5 cases per month.
In total, 56 people (18.9 %) were likely infected during travel abroad (Table 1), which is at the same level as in 2023. Italy was the most frequent travel destination among those infected with Legionnaires’ disease outside Denmark (17 cases). Next were Greece and Turkey with nine cases each, and the United Arab Emirates (Dubai) with five cases. Thus, the same countries dominate the list each year, but as a new trend, many cases have been linked to Greece in both 2023 and 2024.
Fifty of the 56 cases were reported to the European Centre for Disease Prevention and Control (ECDC) for preventive follow-up in the respective countries. The few unreported cases were due either to stays in private settings (e.g. own house) or missing information about accommodation during the incubation period.
Twelve cases were part of eight clusters with two or more Danish or international cases – including two clusters in Greece, one of which involved three Danish citizens, and two clusters in Italy, one of which involved two Danish citizens.
In total, 21 of the travel cases were culture-verified, 17 with SG1 (81 %), of which 16 belonged to SG1 Pontiac subgroups. One case associated with travel to Turkey was identified as L. bozemanae by culture, which – as far as is known – is the first travel-associated case of culture-confirmed Legionnaires’ disease caused by a species other than L. pneumophila.
A total of 15 cases of travel-associated Legionnaires’ disease were LUT-positive (39 % of all LUT-positive), of which nine were diagnosed exclusively with LUT. Among these, five were PCR-negative, two of them only having samples from the upper respiratory tract.
Travel-related infections typically occur in connection with water installations where Legionella has had favorable growth conditions. Examples of potential sources in travel settings include:
- Hotels and holiday homes where water installations can serve as reservoirs if not properly maintained and operated.
- Spas and jacuzzies that generate aerosols and, if not sufficiently disinfected, can be potent sources of infection.
- Ships and cruises with water tanks and recirculation systems, including showers in cabins.
- Public fountains, misters, and cooling towers, which may occasionally spread infection to the environment.
Preventive measures in travel-related contexts include letting all bathroom taps run for a few minutes before showering, checking whether the hot water is sufficiently hot (so hot that you cannot hold your hand under it), and avoiding inhalation of sprayed warm water, especially from older or poorly maintained installations. It is also advisable to avoid spas if hygiene appears uncertain.
Risk groups, such as people with COPD, smokers, and the elderly, may benefit from exercising particular caution.
In addition to travel-associated infections, infections can also occur in nursing homes, hospitals, other institutions, and in the patient’s own home, including gardens and greenhouses. It is also advisable to flush all taps in one’s home thoroughly with both cold and hot water after periods of reduced or interrupted use, e.g., due to travel or absence.
Laboratory-Confirmed Cases in 2024
L. pneumophila was detected in 110 patients by culture. L. longbeachae was detected in six patients, and L. bozemanae in three patients. In 2024, a total of 119 out of 296 cases (40 %) were confirmed by culture, which is at the same level as in the past three years. The distribution by serogroup and subgroup for L. pneumophila is shown in Table 3.
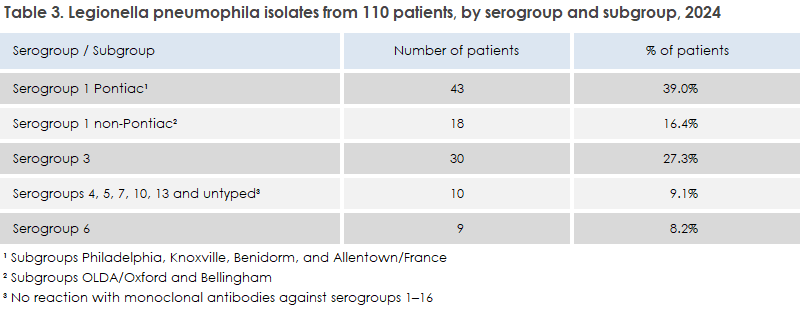
In addition to serogroup determination, the clinical L. pneumophila isolates were also assigned a sequence type (ST) using whole genome sequencing. A total of 51 different sequence types were identified. The most common ST, as in previous years, was ST1 (belonging to SG1, both Pontiac (Philadelphia) and non-Pontiac (OLDA/Oxford)) with 16 isolates (14.5%). This is somewhat lower than the usual 20–25%, which is related to the unusually low number of OLDA/Oxford cases (n = 14), of which 13 were ST1. This subgroup is normally the most common cause of Legionnaires’ disease among Danes, but in 2024 the Benidorm subgroup (a much more virulent type), with 16 cases, was the most common culture-confirmed cause. It should be noted, however, that six of the Benidorm cases were imported, while none of the OLDA/Oxford cases were imported. The second most frequent ST was, as usual, ST87 with nine isolates (8%), belonging to SG3 (all infected in Denmark). For 34 STs, there was only a single case each.
Serogroup 3 accounted for a somewhat higher proportion (27.3%) than in 2022 and 2023 (19.8% and 17.1%, respectively); all are presumed to have been infected in Denmark.
In total, 281 patients tested positive for Legionella PCR (94.9%). The L. pneumophila urinary antigen test (LUT), which almost exclusively detects SG1, was positive in only 38 cases (12.8%), the lowest level ever recorded. Respiratory samples from eight LUT-positive patients were negative by PCR, although four of these were upper respiratory tract samples.
Altogether, 39 of the 281 PCR-positive patients (13.9%) tested positive for Legionella species non-pneumophila (n = 36) or Legionella species (n = 3) without further examination for L. pneumophila.
Of the 36 non-pneumophila cases, the species could be identified in 19 cases by sequencing the region between the 23S and 5S genes. The most common were L. longbeachae with six cases, L. anisa with four cases, and L. bozemanae and L. rubrilucens with two cases each. L. feeleii, L. cincinnatiensis, L. lytica, L. micdadei, and L. sherrii were each detected in one case (a total of nine different species).
Of these 36 cases, 27 were from the Capital Region, where non-pneumophila testing is performed. In addition to these 27, there were seven culture-confirmed non-pneumophila cases from the region. Thus, the 34 Legionella non-pneumophila cases accounted for 31.8% of the total 107 cases from this region, which is at the same level as in 2023.
In addition to the Capital Region, Legionella species are also detected at some clinical microbiology departments in Southern Jutland. Of a total of 44 cases from Southern Jutland, at least seven were caused by non-pneumophila (16%), but testing for non-pneumophila is not performed throughout the entire region.
Legionella longbeachae and Other Legionella Species
In 2024, Legionella longbeachae was detected in a total of 12 patients. However, the actual number of cases is assumed to be at least twice as high. All cases were diagnosed either in the Capital Region (nine cases) or in Southern Jutland, and species identification was carried out at SSI. In 2023, ten cases were identified, three by culture and seven via 23S–5S sequencing.
L. longbeachae is not believed to spread via water systems, which distinguishes it from e.g. L. pneumophila. It is a natural soil bacterium and can multiply to high concentrations in compost, potting soil, plant soil, and soil improvement products. In 2024, the bacterium was detected in five of six commercial soil products examined, which had been handled by patients with infection.
Concentrations were up to 200,000 cfu/gram product. Most cases occur in the summer and early autumn months. Transmission is assumed to occur, among other ways, through inhalation of aerosols. However, studies have shown that good hand hygiene – such as handwashing and glove changes – is the most effective preventive measure. It is also recommended to moisten the soil carefully to reduce dust and to handle soil products outdoors in fresh air, rather than indoors, e.g., in greenhouses.
It is not only L. longbeachae that occurs in these soil products. L. bozemanae is often found alongside L. longbeachae. In addition, L. pneumophila (and other species) can also be cultured from potting soil and similar products, though usually in lower concentrations. In 2024, five cases of L. bozemanae infection were identified. In none of these cases were potting soil/soil improvement products examined.
L. anisa was identified in four patients by sequencing. It is generally considered apathogenic or of low pathogenicity, but it is the second most common species that can be cultured from water samples. The four patients were of advanced age, over 85 years (average 92.5 years), which likely contributed to the severity of the illness. The fatality rate for these four cases was 50 %. On average, they were significantly older than patients with L. longbeachae, who had an average age of 70.4 years, with no deaths recorded.
This annual report is also discussed in EPI-NEWS 27/2025.