No 50 - 2016
Tuberculosis 2015
Tuberculosis 2015
2015 saw a total of 356 notified cases of tuberculosis (TB), 90 (25%) in persons of Danish origin and 266 (75%) in persons of non-Danish origin (immigrants or descendants to immigrants). The overall incidence was 6.3 per 100,000.
For persons of Danish origin, the median age was 51 years (range 16-92 years). A total of 65 men and 25 women were notified, corresponding to an M/F ratio of 2.6/1.
For persons of non-Danish origin, the median age was 33 years (range 0-81 years). A total of 173 men and 93 women were notified, corresponding to an M/F ratio of 1.9/1.
The difference in median age reflects the fact that TB is mainly observed in middle-aged and elderly Danes, whereas the condition is mainly seen in young and younger adults of non-Danish origin, Figure 1.
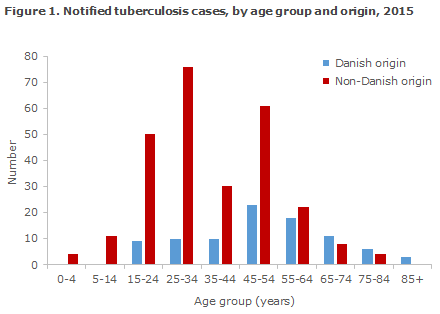
Table 1 shows the distribution by area and origin.
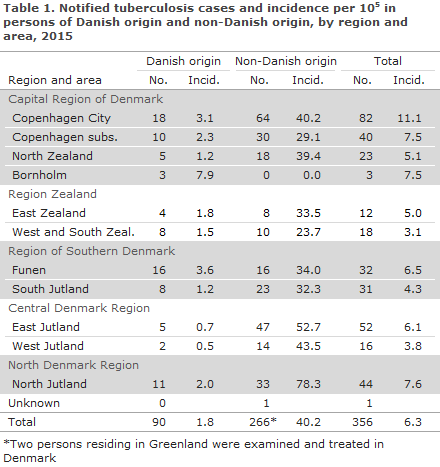
As previously, the highest incidence (11.1 cases per 100,000) was seen in the City of Copenhagen, corresponding to 23% of all detected tuberculosis cases.
The areas of North Jutland, Copenhagen subs. and Funen had incidences exceeding the national average (7.6, 7.5 and 6.5 per 100,000, respectively), whereas the lowest incidence was recorded in West and South Zealand (3.1 per 100,000).
Figure 2 presents the development in the TB incidence in persons of Danish origin, by region in the 2011-2015 period.
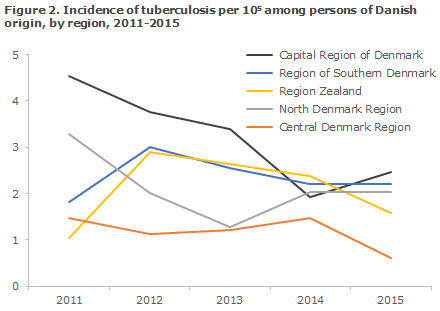
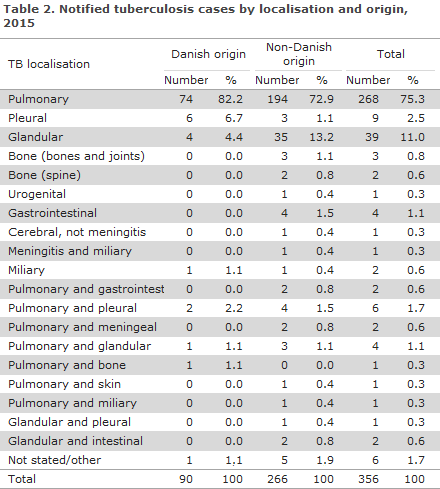
Table 2 shows the distribution by TB localisation and origin.
A total of 39 (11%) patients were notified with relapse, including 17 Greenlanders, five Danes, four Somalis, three Romanians, two Syrians and Afghans, respectively, and one person from each of the following countries: Bosnia and Herzegovina, Burundi, Ethiopia, Pakistan, Russia and Sweden. For a total of 15 (38%) of the patients, the previous TB episode had occurred within the past four years.
For one of these patients, there was information about previous TB treatment failure. In another two cases, TB treatment outcome was recorded as completed and cured , respectively; and for the remaining 12 patients, there was no information about previous TB treatment, either because no treatment form had been received following the previous TB episode, EPI-NEWS 27-33/13, or because the patient had received treatment abroad.
Alcoholism, homelessness and/or drug abuse was noted for 26 persons (7%) of whom nine were Danes and 17 immigrants.
As previously, it is estimated that this risk factor is underreported in the notifications.
Information about concurrent HIV infection and therefore AIDS was provided in nine (2.5%) cases, two Danish and seven immigrant cases.
For seven patients (2%), there was information that the patient was immunosuppressed iatrogenically due to TNF-alpha inhibitor treatment or was immunosuppressed due to other causes.
Country of infection and origin
Based on notifications, a total of 123 (35%) cases were presumably infected in Denmark, including 75 of Danish origin. In all, 12 persons were born in Denmark, but were of non-Danish origin. A total of 36 (10%) immigrants were presumably infected in Denmark, including 23 from Greenland, three from Germany and the remaining 10 cases from nine other countries.
Among the 233 (65%) persons who were presumably infected outside of Denmark, 15 were of Danish origin, including one who was presumably infected in Bulgaria, Romania and Turkey, respectively, and a total of three who were presumably infected in Asia. For the remaining eight, the country of infection was unknown or not stated.
A total of 218 (82%) of 266 persons of non-Danish origin were presumably infected abroad; the overwhelming majority of these persons were infected in their countries of origin. For a total of nine persons of non-Danish origin, the country of infection was unknown.
TB among Greenlanders in Denmark
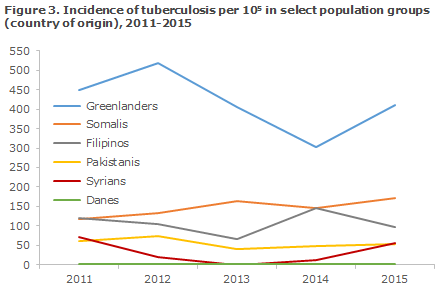
2015 saw a total of 65 notified cases of TB in Greenlanders. This was an increase from 47 cases in 2014, and at an incidence of 410 cases per 100,000, Greenlanders living in Denmark remain the greatest single group among the TB cases of non-Danish origin (24% of the persons of non-Danish origin, 18% of all cases), Figure 3. The majority of cases were notified from the City of Copenhagen (22) South and East Jutland (11 each) or North Jutland (9).
TB in children
A total of 15 cases of TB in children below the age of 15 years were notified (22 in 2013, nine in 2014), including four below the age of five years.
Out of 15 children, eight were born in Denmark by non-Danish parents, and six of the children had probably become infected in Denmark. Seven children were born abroad and all had probably become infected before their arrival to Denmark.
A total of 12 children had pulmonary TB, including one who also had TB meningitis, one child had cerebral TB (an intracerebral tuberculoma) and glandular TB, and for one child the localisation was unknown.
Nine of the children (60%) had probably become infected by a member of their household. A single Danish child was infected through contact to a person who was not part of the household and who had become infected with TB more than three years ago. One child had relapse (TB in 2005), and for four children the source of infection was unknown.
In addition to the 15 notified children, information was provided on positive culture from the lungs of two Danish children (siblings), both below five years of age, who have not yet been notified despite several reminders.
Occupational infection
In three cases, infection had possibly occurred in relation to occupational activity. One person, a construction worker, was believed to have become infected by a work colleague.
The patient and the colleague turned out to belong to the same small chain of infection, which speaks in favour of a connection between the two cases. One had reportedly become infected through work with socially exposed people. On the basis of typing of isolates, occupational infection could neither be confirmed nor dismissed as the patient belonged to the infectious chain “cluster 2” (see below).
Finally, one person had reportedly become infected through a colleague of non-Danish origin who had recently initiated treatment. No personal information was available about the colleague, but the patient and only one more person in Jutland, who was of non-Danish origin and from the same area, belonged to the infection chain in question, which speaks for a connection.
Outbreaks
A total of 30 cases were linked to an epidemiologic outbreak code belonging to a total of 16 outbreaks counting 2-5 persons each. Six persons linked to two different outbreak codes were associated with Sundholm in the Copenhagen area. A total of 24 persons belonged to various different family outbreaks.
Microbiological diagnostics
In 2015, the TB diagnosis was confirmed by culture with subsequent species determination in 277 of the 356 (78%) notified cases, including 78 of the 90 (87%) cases in Danes and 199 of the 266 (75%) cases in immigrants. All cases were caused by classic M. tuberculosis.
Among the 79 notified cases who had not been culture-verified, nine (11%) cases had a positive PCR at the SSI, one of which was performed on paraffin-embedded (dead) tissue and therefore the sample in question had not been cultured. The remaining eight PCR-positive cases were culture-negative, but two were positive upon microscopy. Negative culture despite positive PCR and/or microscopy may be due to patients having been started on anti-tuberculosis treatment before the culture samples were taken. On the basis of the EU disease definition, EPI-NEWS 51/09, a total of 279 (78%) were confirmed cases, eight (2%) probable cases and 69 (19%) were possible cases.
Among a total of 286 notified cases of pulmonary TB (± other localisation), 230 (80%) cases were verified by culture, including 69 of the 78 (88%) Danish cases and 161 of the 208 (77%) immigrant cases. By microscopy of expectorates from 69 Danes with culture-confirmed pulmonary TB (+/- other localisation), 46 (67%) tested positive and were thus regarded as infectious.
This proportion was 53% in immigrants (85 of 161). Among all 230 cases of culture-verified pulmonary TB, 138 (60%) were tested by PCR at the SSI, of whom 102 (74%) tested positive.
Typing of bacteria from 275 of 277 (99%) culture-verified TB patients from 2015 showed that a single chain of infection, ”C2/1112-15” (previously named “cluster 2”), EPI-NEWS 04/14 and 03/15, remains dominant. A total of 47 (17%) patients belonged to this chain of infection; 31% (24 of 78) Danes, 30% (16 of 54) Greenlanders and 5% (7 of 143) other immigrants.
Resistance
Drug resistance results were available for all 277 culture-verified cases.
A total of 249 of these cases were notified with TB for the first time, including 74 Danes and 175 immigrants. Among those notified for the first time, isoniazid monoresistance was detected in 13 (5%) patients, including two Danes and 11 immigrants from Somalia (3), Thailand (2), Armenia (1), Congo (1), Mongolia (1), The Philippines (1), Poland (1) and Vietnam (1). Additionally, rifampicin monoresistance was detected in a Somali-born patient. No monoresistance was detected among the 28 previously notified culture-positive TB patients, including four Danes and 24 immigrants.
Additionally, five multiresistant (MDR) and one extremely resistant (XDR) case were detected, corresponding to 2.2% MDR/XDR TB. MDR is resistant to the two primary antibiotics, isoniazid and rifampicin, and possibly to other antibiotics as well. The term XDR resistance designates MDR resistance and additional resistance to a minimum of one of the important second-line drugs belonging to the group of fluoroquinolones and a minimum of one of the three injectable drugs amikacin, capreomycin or kanamycin. If resistance testing shows MDR and only fluoroquinolone resistance or only resistance to one or more of three of the mentioned injectable drugs, the term “pre-XDR” TB is often used. Two of the five detected MDR cases in 2015 were pre-XDR TB.
The XDR TB case was a 47-year-old Russian-born patient who had microscopy-positive (infectious) pulmonary TB. The patient’s isolate was resistant to no less than 13 of 16 tested drugs. One of the two pre-XDR cases was a 20-year-old Somali-born patient who had TB in the spine and in whom the isolate, in addition to MDR, was resistant to all of the tested fluoroquinolones and to ethambutol, pyrazinamide, streptomycin and ethionamide.
The second of the two pre-XDR cases was a 30-year-old Syrian-born patient who had microscopy-positive pulmonary TB and whose isolate, in addition to MDR, was resistant to amikacin, kanamycin, streptomycin, pyrazinamide, cycloserin and ethionamid. One of the three MDR TB cases was a 16-year-old Somali-born patient who had microscopy-positive pulmonary TB and whose isolate, in addition to MDR, was resistant to streptomycin, ethionamid and pyrazinamide. The second of the three MDR TB cases was a 32-year-old Somali-born patient who had microscopy-negative pulmonary TB and whose isolate, in addition to MDR, was resistant to Streptomycin.
The last of the three MDR TB cases was a 40-year-old Danish-born patient who had microscopy-negative pulmonary TB and whose isolate, in addition to MDR, had no additional resistance findings.
Commentary
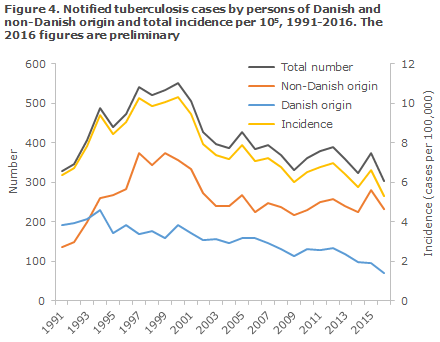
The overall incidence for 2015 (6.3 per 100,000) showed a slight increase relative to 2014 (5.6 per 100,000), EPI-NEWS 15/16. The increase was due to more detected cases among persons of non-Danish origin, Figure 4, and the heightened inflow to Denmark of refugees in 2015 contributed to this.
Nevertheless, it seems that this trend has not continued into 2016, when a total of 302 TB cases have been notified to date, including 232 (77%) cases among persons of non-Danish origin. It should, nevertheless, be stressed that the figures are preliminary and will increase further, in part because more cases may be notified this year; and in part because TB cases notified in 2017, but with symptom onset in 2016, count as 2016 cases.
Even though the number of cases among ethnic Danes is decreasing in the Copenhagen area - possibly owing to intensified active infection tracing since 2012, EPI-NEWS 15/16 - the region has a total incidence of more than 10 per 100,000, which is the threshold value for low incidence. One of the main reasons for this is the still high and increasing occurrence among Greenlanders as most of the increase in cases in Greenlanders were observed in the City of Copenhagen.
It is encouraging that relatively few children were notified with TB (15 cases, 4%), but it is also cause for concern that about half of the children presumably became infected in Denmark. We have specific knowledge about lacking notification of culture-verified TB in two Danish children, which may raise suspicion that some under-reporting occurs of TB among children. This may occur because healthcare workers insist less on taking diagnostic samples from children and instead base the diagnosis on recent contact to a TB patient, the patient’s symptoms and maybe on a positive Mantoux/IGRA test.
Further reasons may be that children have a lower bacterial load than adults and therefore less frequently test positive by microscopy, PCR and/or culture when samples are submitted for testing, and that it may be easier to forget to notify the clinically detected cases.
Globally, the TB incidence is decreasing, but the total global number of TB cases (the prevalence) increases due to population growth. Furthermore, some parts of the world are facing considerable challenges due to resistant strains, including MDR and XDR TB. The resistant strains are primarily seen in Eastern Europe, South-East Asia and in Southern Africa. For instance, 18% of all tested new pulmonary TB cases in 2014 had MDR TB in the WHO’s European Region, which includes parts of Eastern Europe.
In contrast, Denmark has so far been spared serious problems relating to MDR and XDR TB. On average, as little as two MDR TB cases have been detected annually in the past many years, corresponding to approx. 0.5% of all TB cases.
2015 saw the highest ever number of MDR/XDR TB cases ever recorded in Denmark, and the second ever case of XDR TB. The first ever case of XDR TB in Denmark, also from Russia, was recorded in 2013, EPI-NEWS 03/15. To date, the number of cases recorded in 2016 also exceeds the average as four MDR TB cases have presently been diagnosed.
The increase in MDR, pre-XDR and XDR TB cases is worrying. These are very serious forms of resistance that require considerably prolonged (1 to 2 years) and complicated treatment with many different antibiotics and entail a considerable risk of complications and adverse effects. Furthermore, the treatment of XDR TB, in particular, is very costly and requires prolonged - often many months of - hospital admission.
It is important that the resistant cases are diagnosed as early as possible in the course of the disease to avoid incorrect treatment and unnecessary complications for the affected people, and unnecessary spreading of resistant strains in the community. The many isoniazid monoresistant patients in 2015 (5%) stress the importance of culturing the diagnostic samples to ensure that isoniazid resistance (or other forms of resistance) is not missed and thereby in practice to give these patients monotherapy in the continuation phase of their treatment, i.e. the final four months of treatment when the standard treatment regime is based on isoniazid and rifampicin.
Otherwise, the result may be additional development of MDR TB. The importance of reminding of this is stressed by the report in EPI-NEWS 15/16. The report, which were based on the Danish microbiology database (the MiBa), demonstrated that not all of the samples tested locally by PCR were also cultured as recommended nationally and by the ECDC.
In addition to missing resistance, this may potentially cause under-diagnosing and under-reporting of TB as culture remains a more sensitive method than PCR, why more patients are identified at an earlier stage of their disease when their samples are cultured.
Currently, as part of an ongoing research and development project at the SSI, a more expedient diagnostic flow has been introduced, which means that genotypic determination of resistance is done as early as possible by use of various PCR/DNA-based methods, which are subsequently validated and supplemented by culture-based methods. This ensures that resistant TB strains are detected earlier in the disease course. It is our ambition to continue this project into 2017.
As previously, in 2015 the systematic typing of bacteria from culture-positive TB patients from 1992 onwards demonstrated that a single chain of infection, "C2/1112-15" (previously cluster 2), continues to comprise a considerable problem in Denmark, EPI-NEWS 04/14 and 03/15. Among the culture-positive patients in 2015, 31% of the Danes, 30% of the Greenlanders and 5% of immigrants from other countries belonged to this chain of infection which is by far the largest infectious chain in Scandinavia.
So far, a total of more than 1,000 cases have been recorded as from 1992. During the initial approx. 10 years, the patients in the infectious chain were predominantly of Danish origin, but 2015 once again brought an increasing share of cases relating to Greenlanders residing in Denmark and immigrants.
As mentioned, thanks to active screening, some patients belonging to the C2/1112-15 chain (and other chains of infection) are detected every year, but systematic screening is still not in place beyond Copenhagen, where approx. 60% of all patients reside.
(P.H. Andersen, A.H. Christiansen, Department of Infectious Disease Epidemiology,T. Lillebæk, National TB and Mycobacteria Reference Laboratory)
Link to previous issues of EPI-NEWS
14 December 2016