No 3 - 2015
Tuberculosis 2013
European training programme to become a field epidemiologist (EPIET) or a field microbiologist (EUPHEM)
Tuberculosis 2013
2013 saw a total of 355 notified cases of tuberculosis (TB), 116 (33%) in persons of Danish origin and 239 (67%) in persons of non-Danish origin (immigrants or descendants to immigrants). The overall incidence was 6.3 per 100,000.
For persons of Danish origin, the median age was 50 years (range 0-84 years) and the M/F ratio was 2:1. Correspondingly, the median age for persons of non-Danish origin was 35 years (range 0-82 years) and the M/F ratio was 1.7:1. The difference in median age reflects that TB is mainly observed in middle-aged Danes, whereas the condition is mainly seen in adolescents and younger adults of non-Danish origin, Figure 1.
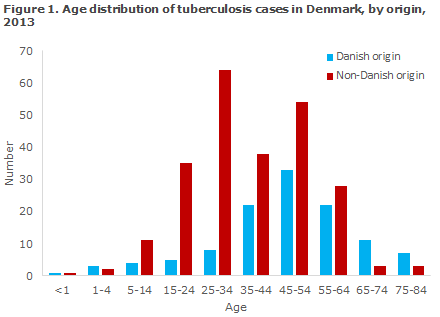
Table 1 shows the distribution by area and origin.
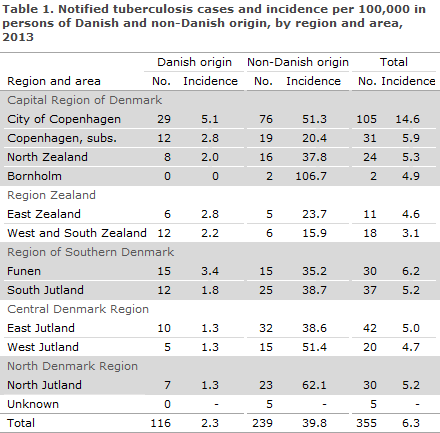
As previously, the highest incidence (14.6 cases per 100,000) was seen in the City of Copenhagen, corresponding to 30% of all detected tuberculosis cases.
The areas of Funen and the suburbs of Copenhagen had the second-highest incidences (6.2 and 5.9 per 100,000, respectively), whereas the lowest incidence was seen in West and South Zealand (3.1 per 100,000).
The mean number of notified cases and the mean incidences per 100,000 for the 2008-2012-period are presented in Table 2, by area and origin.
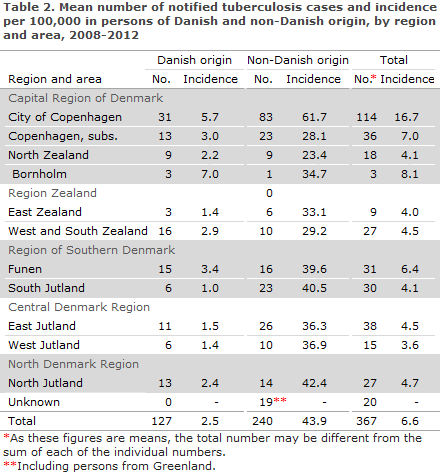
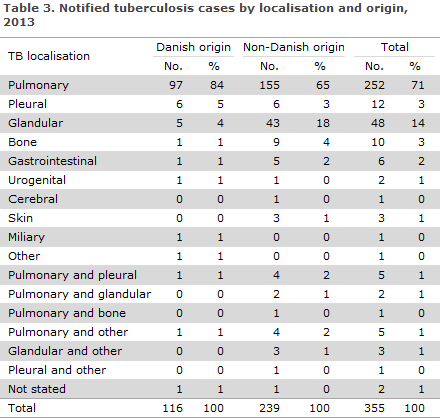
Table 3 shows the distribution by TB localisation and origin.
A total of 24 (7%) patients were notified with relapse, including 14 Greenlanders, three Danes, two Somalis and one from each of the following countries: Vietnam, India, Bosnia-Herzegovina, Tanzania and Afghanistan.
Alcohol abuse and/or homelessness were noted for 40 patients (11%) of whom 15 were Danes and 25 immigrants. It is thought that this risk factor is underestimated in notifications.
According to the notifications, information on concurrent HIV infection and therefore AIDS was provided in 10 (2.8%) cases, five Danish and five immigrant cases.
TB patients' HIV testing rate increased in the 2007-2011 period, from 43% to 72%, EPI-NEWS 50/12. The 2013 share of HIV-tested TB patients remains unknown.
For five patients there was information that the patient was diabetic, was immunosuppressed iatrogenically due to TNF-alpha inhibitor treatment or was immunosuppressed due to other causes.
Country of infection and origin
Based on notifications, a total of 167 (47%) patients were presumably infected in Denmark, including 101 of Danish origin and 13 second-generation immigrants born in Denmark. A total of 53 (15%) immigrants were presumably infected in Denmark, including 36 from Greenland, three from Somalia and the remaining 14 cases from 10 other countries.
Among the 188 (53%) persons who were infected outside of Denmark, 15 were of Danish origin, including one who was presumably infected in Laos and another presumably infected in the US. For the remaining 13, the country of infection was unknown.
A total of eight cases of Danish origin, infected abroad, were presumably infected during tourist travels, and one during a stationing. For the remaining six Danes, the mode of infection was unknown.
A total of 173 (72%) persons of non-Danish origin were infected abroad. Among these, 15 were infected in a country other than their country of origin, but the remaining 158 were presumably infected in their countries of origin, including 24 Greenlanders, 22 Somalis, seven Pakistanis, seven Rumanians, seven Myanmarians, six Filipinos, five Indians and five Thais. An additional 73 immigrants were infected in a total of 35 different countries of origin. For a total of nine immigrants, the country of infection was unknown.
TB among Greenlanders in Denmark
The TB increase among Greenlanders in Denmark observed since 2009, EPI-NEWS 50/10, 50/11, 50/12 and 4/14, discontinued in 2013 as a total of 62 Greenlanders were notified with TB, of whom 14 (23%) were recurrences. The now down-sloping trend seems to continue as the preliminary number of Greenlanders notified with TB in 2014 is 40 cases.
Nevertheless, Greenlanders in Denmark remained the largest group of TB cases among persons of non-Danish origin (26%) and nearly a fourth of the notified cases were recurrences. The incidence among Greenlanders in Denmark was approx. 400/100,000. For comparison, the TB incidence in Greenland averaged 200/100,000 in the 2010-2012-period.
Information on homelessness and/or abuse was provided in 18 (29%) cases. A total of 30 were notified from the City of Copenhagen, five from North Jutland, eight from South Jutland, four from Funen, 10 from East Jutland, four from West Jutland and one case from North Zealand.
TB in children
A total of 22 cases of TB in children below the age of 15 years were notified, including seven below the age of 5 years. Eight of the children were Danes; all had been infected in Denmark. Among the 14 non-Danish children, five were presumably infected in Denmark, eight in their parents' respective countries of origin, and for one child the country of origin was not stated.
A total of 14 (64%) children were probably infected by a member of their household who had had TB within the past 3 years; four Danish children and 10 children of non-Danish origin. Two Danish children were infected through contact to a person who was not part of their household who had been infected with TB less than 3 years ago, and in six children the source of infection was unknown.
A total of 19 (86%) children, seven Danish and 12 children of non-Danish origin, had pulmonary TB, including one Danish child with both pulmonary TB and TB of the ear. One Danish child and two children of non-Danish origin had glandular TB, the latter also had TB of the skin.
Microbiological diagnosis
In 2013, the TB diagnosis was confirmed by culture with subsequent species determination in 276 of the 355 (78%) notified cases, including 86 of the 116 (74%) cases in Danes and 190 of the 239 (79%) cases in immigrants. One case of M. africanum was detected in an immigrant from Guinea-Bissau. The remaining cases (275) were caused by classic M. tuberculosis.
Among the 79 notified cases that were not confirmed by culture, 18 (20%) cases had a positive PCR, two of whom also had a positive microscopy. In four of the 18 PCR-positive cases, the diagnosis was made on paraffin-embedded (dead) tissue, and therefore samples were not cultured. The remaining 14 PCR-positive cases were culture negative. On the basis of the EU disease definition, EPI-NEWS 51/09, a total of 278 (78%) were confirmed cases, 16 (5%) probable cases and 61 (17%) were possible cases.
Among a total of 265 notified cases of pulmonary TB (± other localisation), 216 (82%) cases were verified by culture, including 76 of the 99 (77%) Danish cases and 140 of the 166 (84%) immigrant cases. By microscopy of expectorates from 76 Danes with culture-confirmed pulmonary TB (+/- other localisation), 47 (62%) tested positive and were thus regarded as infectious. This proportion was 52% in immigrants (73 of 140).
Among all 216 cases of culture-verified pulmonary TB, 155 (72%) were tested by PCR, of whom 126 (81%) tested positive.
Resistance
Drug resistance results were available for 275 of 276 culture-verified cases.
A total of 255 of these cases were notified with TB for the first time, including 83 Danes and 172 immigrants. Among those notified for the first time, isoniazid mono-resistance was detected in 17 (7%) patients, including three Danes and 14 immigrants.
Additionally, one multiresistant (MDR) and one extremely resistant (XDR) case were detected. MDR is resistance to the two primary antibiotics, isoniazid and rifampicin, and to any other antibiotics. The MDR-TB patient was microscopy-negative and had a strain that was resistant to isoniazid, rifampicin and ethambutol and to amikacin and capreomycin, but sensitive to ofloxacin and moxifloxacin.
The XDR-TB patient had a strain that in addition to being resistant to isoniazid, rifampicin and ethambutol was also resistant to amikacin, capreomycin, ofloxacin and moxifloxacin. This patient was microscopy-positive and therefore infectious. To the best of our knowledge, contact tracing identified no other infected persons. Both cases were detected in Russians with pulmonary tuberculosis.The patients had recently arrived to Denmark as refugees and had therefore presumably been infected in their country of origin.
In 20 patients with positive culture, information on previous TB was provided; this group comprised two Danes and 18 immigrants. In one immigrant, XDR resistance was detected (see above); and in one Dane, isoniazid resistance was detected.
Commentary
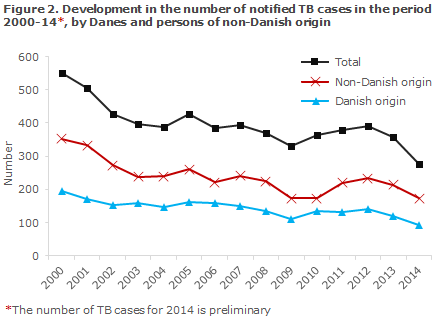
Following a sustained decrease in the total number of annual cases of tuberculosis in the 2001-2009-period and an increase in the 2010-2012-period, EPI-NEWS 50/12 and 4/14, the incidence once again followed a slightly decreasing trend in 2013. Seemingly, the decreasing trend has continued throughout 2014 - with a proviso for lacking notifications - as less than 300 cases have currently been notified, Figure 2.
The overall incidence in 2013 (6.3 per 100,000) was 0.3 per 100,000 lower than the mean observed in the previous 5 years (6.6 per 100,000), Table 1 and Table 2.
The decrease was divided between persons of Danish and non-Danish origin, including Greenlanders notified with TB.
As previously, a large share of all tuberculosis cases were presumably infected in Denmark (47%), whereas the majority of immigrants were presumably infected before arriving to Denmark, alternatively during visits to their countries of origin.
Despite the recorded decrease in incidence, Greenlanders in Denmark are still a population group at special risk of infection or reactivation of TB infection and continues to demand a special focus.
The total decrease in the number of notified tuberculosis cases from 2008 to 2013 was as low as 8%. This corresponds to an annual reduction in TB incidence of just 2 percentage points, which is insufficient in relation to the WHO's strategy on global elimination of TB no later than by 2035.
Additionally, systematic typing of bacteria from TB patients with positive cultures from 1992 onwards demonstrates that a single chain of infection, "C2/1112-15" previously cluster 2), kept growing, EPI-NEWS 4/14. Many of the C2/1112-15 patients are Danish and Greenlandic males with an excess incidence of social problems and abuse issues.
A TB incidence among Greenlanders in Denmark in the order of 400/100,000 and a continued increase in the number of cases in the C2/1112-15 chain of infection demonstrate a continuous need for great awareness of TB control in Denmark. The majority of cases among Danes are detected in middle-aged persons, Figure 1, in contrast to our neighbouring countries where TB in the ethnic population is mainly seen in elderly persons, and where the cause is primarily reactivation rather than first-time infection.
For example, the share of infection chains with a minimum of two identical bacterial strains ("clustering rate") was 60% in Denmark in 2012, whereas the corresponding numbers for the remaining Nordic countries was 18-27%. In 2012, the number of major infection chains exceeded that observed in the remaining Nordic countries. Despite the current decrease in the number of notified cases, all of these conditions bear witness to continued transmission in Denmark.
The Danish Health and Medicines Authority has prepared a new guideline on tuberculosis that describes notification, infection tracing and hygiene issues, and which will expectedly be published shortly. Along with the appointment of regional tuberculosis coordinators and active contact tracing in risk environments, the guideline shall contribute to reducing transmission both in the short and longer run so that Denmark may meet the WHO's long-term objective of eliminating TB no later than in 2035.
(S. Voss, P.H. Andersen, Department of Infectious Disease Epidemiology, E. Svensson, National TB and Mycobacteria Reference Laboratory)
European training programme to become a field epidemiologist (EPIET) or a field microbiologist (EUPHEM)
Once again it is possible to apply for the 2-year European training programme to become a field epidemiologist, EPIET (European Programme for Intervention Epidemiology Training). Participants will achieve skills comprising, among others, monitoring and control of infectious diseases, outbreak tracing and handling, applied research, communication etc.
The programme consists of 2 years of stationing in another European country. It is “on-the-job training” and participation in the study programme is remunerated. Participants are expected to have undergone relevant training, possess experience in the field of public health and to have an interestin field epidemiology.
It is also possible to apply for a similar 2-year European training programme for microbiologists, EUPHEM (European Public Health Microbiology Training).
This training programme is also completed as 2 years' of stationing in another European country. Programme participants will achieve proficiency in performing independent laboratory tasks in connection with the surveillance and control of infectious diseases, tracing and management of outbreaks, applied research and communication, etc. Participants are expected to have some work experience in the field of microbiology, to have a PhD degree and an interest in field epidemiology.
Both programmes are offered by the European Centre for Disease Prevention and Control (ECDC), and starts as a joint 3-week introductory course held mid-September 2015.
Applicants to EPIET and EUPHEM shall be citizens of the EU, Iceland, Liechtenstein or Norway with proficiency in English. The deadline for application is 2 February 2015.
For further information, please see www.ecdc.europa.eu or contact Consultant Kåre Mølbak, Department of Infectious Disease Epidemiology (EPIET) or Consultant Robert Skov, Microbiology and Infection Control (EUPHEM).
(Statens Serum Institut).
Link to previous issues of EPI-NEWS
14 January 2015