No 15 - 2016
Tuberculosis 2014
Hexavalent vaccine for the childhood vaccination programme will be provided with the name of Hexaxim®. The vaccine provided is identical to Hexyon®
Tuberculosis 2014
2014 saw a total of 314 notified cases of tuberculosis (TB), 94 (30%) in persons of Danish origin and 220 (70%) in persons of foreign origin (immigrants or descendants to immigrants). The overall incidence was 5.6 per 100,000.
For persons of Danish origin, the median age was 53 years (range 3-84 years) and the M/F ratio was 1.6:1. Correspondingly, the median age for persons of non-Danish origin was 37 years (range 4-91 years) and the M/F ratio was 1.4:1. The difference in median age reflects that TB is mainly observed in middle aged and elderly Danes, whereas the condition is mainly seen in adolescents and younger adults of non-Danish origin, Figure 1.
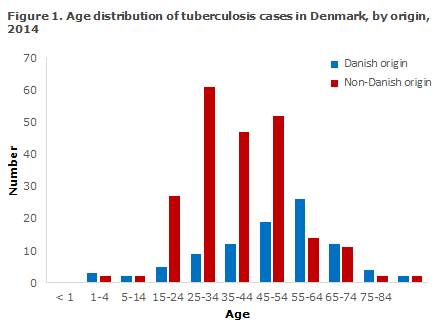
Table 1 shows the distribution by area and origin.
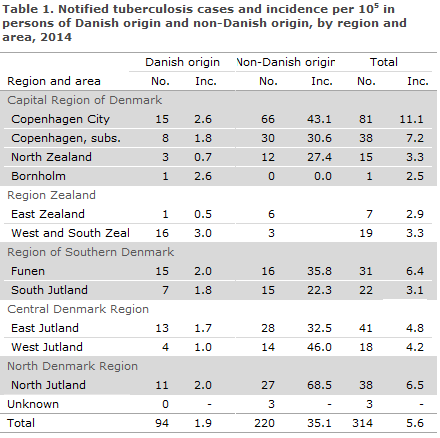
As previously, the highest incidence (11.1 cases per 100,000) was seen in the City of Copenhagen, corresponding to 26% of all detected tuberculosis cases.
The areas Copenhagen Subs., North Jutland and Funen had incidences exceeding the national average (7.2, 6.5 and 6.4 per 100,000), whereas the lowest incidence was recorded on Bornholm (2.5 per 100,000).
The mean number of notified cases and the mean incidences per 100,000 for the 2009-2013 period are presented in Table 2 by area and origin.
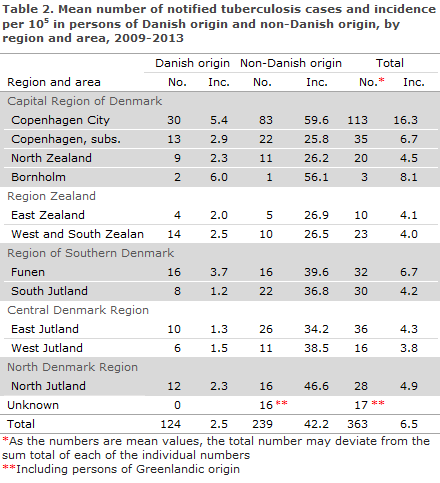
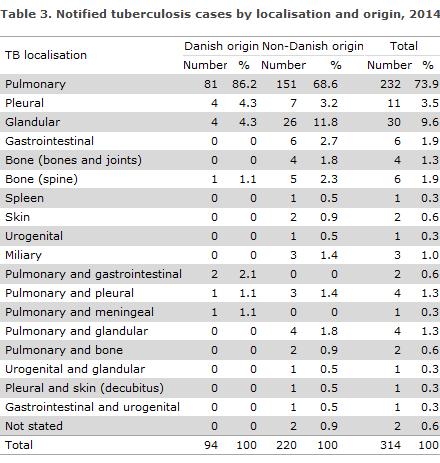
Table 3 shows the distribution by TB localisation and origin.
A total of 26 (8.3%) patients were notified with relapse, including 10 Greenlanders, 6 Danes, 2 Filipinos and Pakistanis, and one from each of the following: Somalia, The Czech Republic, Cameroun, Germany, Bulgaria and Iran. For a total of 14 (54%) of the patients, the previous TB episode had occurred within the previous 4 years. Among these, there was information about treatment failure in connection with the previous TB episode in two cases, in 11 cases the previous TB treatment was recorded as concluded, and for one patient this information was unknown.
Alcohol abuse and/or homelessness were noted for 25 patients (8%) of whom nine were Danes and 16 immigrants. It is estimated that this risk factor is underestimated in notifications.
According to the notifications, information on concurrent HIV infection and therefore AIDS was provided in five (1.0%) cases, one Danish and four immigrant cases.
For nine patients (3%), there was information that the patient was diabetic, was immunosuppressed iatrogenically due to TNF-alpha inhibitor treatment or was immunosuppressed due to other causes.
Country of infection and origin
Based on notifications, a total of 130 (41%) patients were presumably infected in Denmark, including 82 of Danish origin and six descendants to immigrants born in Denmark. A total of 42 (13%) immigrants were presumably infected in Denmark, including 24 from Greenland, four from Germany and the remaining 14 cases from 11 other countries.
Among the 169 (54%) persons who were infected outside of Denmark, six were of Danish origin, including three who were presumably infected in Thailand, another two in Greenland and one in Russia.
For the remaining 15 (5%), the country of infection was unknown or not stated.
A total of 163 (74%) of 220 persons of non-Danish origin were presumably infected abroad; the overwhelming majority of these persons were infected in their countries of origin. For a total of nine persons of non-Danish origin, the country of infection was unknown.
TB among Greenlanders in Denmark
The TB increase among Greenlanders in Denmark observed since 2009, EPI-NEWS 50/10, 50/11, 50/12 and 4/14, discontinued in 2013 when a total of 62 Greenlanders were notified with TB. In 2014, the number decreased further to 47 cases, including 10 (21%) recurrences. Nevertheless, Greenlanders in Denmark formed the largest group of TB cases among persons of non-Danish origin (21%), and the incidence among Greenlanders in Denmark was approx. 300 cases per 100,000. The majority of cases were notified from the City of Copenhagen (24), East Jutland (8) or North Jutland (5).
TB in children
A total of nine cases of TB in children below the age of 15 years were notified (22 in 2013), including five below the age of 5 years. All nine children had pulmonary TB. Five of the children were Danes; all had been infected in Denmark. Of the four children of non-Danish origin, two were presumably infected in Denmark and two in the country of origin of their parents.
A total of eight (89%) children were probably infected by a member of their household who had had TB within the past 3 years; four Danish children, three descendants born in Denmark and one child of non-Danish origin born abroad. A single Danish child was infected through contact to a person who was not part of the household who had been notified with TB less than 3 years ago.
Microbiological diagnostics
In 2014, the TB diagnosis was confirmed by culture with subsequent species determination in 270 of the 314 (86%) notified cases, including 80 of the 94 (85%) cases in Danes and 190 of the 220 (86%) cases in immigrants. One case of M. africanum case was detected in a 24-year-old woman from Nepal and one M. bovis case was detected in a 39-year-old man from Nigeria with TB meningitis who had ingested unpasteurised dairy products. The remaining cases (268) were caused by classic M. tuberculosis.
Among the 44 notified cases who had not been culture-verified, six (14%) cases had a positive PCR at the SSI, four of which were performed on paraffin-embedded (dead) tissue for which reason the samples in question could not be cultured. The remaining two PCR-positive cases were culture negative. On the basis of the EU disease definition, EPI-NEWS 51/09, a total of 270 (86%) were confirmed cases, six (2%) were probable cases and 37 (12%) were possible cases.
Among a total of 245 notified cases of pulmonary TB (± other localisation), 217 (89%) cases were verified by culture, including 75 of the 85 (88%) Danish cases and 142 of the 160 (89%) immigrant cases. By microscopy of expectorates from 75 Danes with culture-confirmed pulmonary TB (+/- other localisation), 55 (73%) tested positive and were thus regarded as infectious. This proportion was 58% in immigrants (82 of 142).
Among all 217 cases of culture-verified pulmonary TB, 155 (71%) were tested by PCR at the SSI, of whom 112 (72%) tested positive.
Resistance
Drug resistance results were available for all 270 culture-verified cases.
A total of 250 of these cases were notified with TB for the first time, including 74 Danes and 176 immigrants. Among those notified for the first time, isoniazid mono-resistance was detected in 14 (6%) patients, including seven Danes and seven immigrants.
Additionally, two cases of multiresistant TB (MDR-TB) were detected. MDR-TB is resistance to the two primary antibiotics; isoniazid and rifampicin and any other antibiotics. One of the MDR-TB cases was a 27-year-old Indian-born man who had microscopy-positive (infectious) pulmonary TB. The other MDR-TB case was an 18-year-old Somali-born man who had non-infectious pleural TB. Both patients’ isolates were not resistant to other antibiotics.
In 20 patients with positive culture, information on previous TB was provided; this group comprised six Danes and 14 immigrants. All had fully susceptible TB.
Commentary
Following a sustained decrease in the total number of annual cases of tuberculosis in the 2001-2009 period and an increase in the 2010-2012 period, EPI-NEWS 50/12 and 4/14, the incidence once again followed a slightly decreasing trend in 2013, EPI-NEWS 3/15. This decrease continued in 2014, when the number of notified cases was lower than in any other year in the past 15-year period, Figure 2. The decrease was observed among persons of Danish and among persons of non-Danish origin.
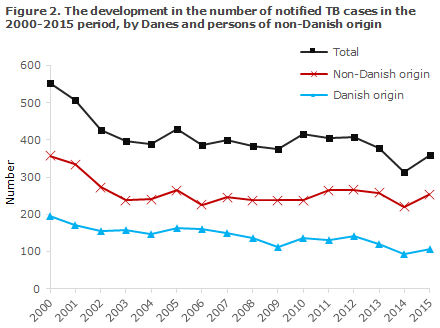
The overall incidence in 2014 (5.6 per 100,000) was 0.9 per 100,000 lower than the mean observed in the previous 5 years (6.5 per 100,000), Table 1 and Table 2.
The decrease was divided between persons of Danish and non-Danish origin, including Greenlanders notified with TB.
An analysis based on the Danish microbiology database (the MiBa) about locally performed PCR in 2014 demonstrated that up to 40% of the samples were not forwarded for culture at the National TB and Mycobacteria Reference Laboratory at the SSI, as recommended nationally and by the ECDC.
This may potentially cause under-diagnosing and under-reporting of TB; under-diagnosing because culture is a more sensitive method than PCR, why more patients are identified at an earlier stage of their disease. It is not possible to establish how many TB patients may have been overlooked due to lacking culture. In 2014, a total of six cases were detected in which a local, positive PCR existed which had, nevertheless, not been notified. Henceforth, the MiBa will be used to underpin the current monitoring through identification of persons who test positive to TB and who have not been notified.
In 2014, a growing share of TB cases was verified by culture (86% compared with 82% in 2013 and 77% in 2012). The increase was primarily observed in cases among ethnic Danes and may reflect some under-reporting of purely clinical TB cases. This will be investigated further through validation of the notified cases against the cases registered in the National Patient Registry.
The recorded decrease in 2014 has not continued in 2015. At present, a total of 360 cases have been notified for 2015. This number is not final and may increase if cases with disease onset in 2015 are reported late, and may decrease if cases are removed from the statistics because the diagnosis later turned out to be incorrect. This occurs every year among the approx. 20% of the cases who do not have tuberculosis bacteria detected by culture. The increase seen in 2015 was primarily observed in the immigrant group and particularly among refugees from areas with a high incidence of tuberculosis, primarily Somalia, Eritrea and Ethiopia, whereas only a limited number of TB cases were detected among asylum seekers from Syria.
As previously, a large share of all tuberculosis cases were presumably infected in Denmark (42%), whereas the majority (74%) of immigrants were presumably infected before arriving to Denmark, alternatively during visits to their countries of origin.
Despite the recorded decrease in incidence, Greenlanders in Denmark remain a population group at special risk of infection or reactivation of TB infection and continues to demand a special focus. The same applies to the socially exposed persons in the Copenhagen area where screening in risk environments from September 2012 and until now have persistently shown that approx. 2-3% of the persons screened have TB, including many with infectious pulmonary TB. At present, no firm decrease in TB incidence has been seen in this population group.
In the autumn of 2015, the National Health Authority has published a new guideline on tuberculosis (in Danish) which describes issues relating to notification, infection tracing and hygiene. Along with the appointment of regional tuberculosis coordinators and active infection tracing in risk environments, the guideline shall contribute to reducing the spreading of infection both in the short and longer run, so that Denmark may meet the WHO's long-term objective on elimination of TB no later than in 2035.
In January 2016, the Danish Society for Infectious Disease published a new guideline on tuberculosis diagnosis and treatment (in Danish). This guideline was prepared to provide practical assistance for physicians who are involved with the treatment of tuberculosis patients.
(P.H. Andersen, S.S. Voss, Department of Infectious Disease Epidemiology, T. Lillebæk, National TB and Mycobacteria Reference Laboratory)
Hexavalent vaccine for the childhood vaccination programme will be provided with the name of Hexaxim®. The vaccine provided is identical to Hexyon®.
Since the end of February and as part of a temporary vaccination programme, Statens Serum Institut (SSI) has provided a hexavalent vaccine for primary vaccination of children who initiate vaccination under the childhood vaccination programme, EPI-NEWS 5/16.
This hexavalent vaccine from Sanofi Pasteur MSD is produced in the EU/EEA. The vaccine is marketed as Hexyon® in Western Europe, as Hexaxim® in markets beyond the EU and as Hexacima® in Eastern Europe.
In pursuance of Section 30 of the Danish Act on Medicinal Products, the SSI may provide medicinal products (in this case vaccines) that are not marketed in Denmark, provided this is done in limited quantities and for a limited period of time in cases when a medicinal product that is marketed in Denmark cannot be procured.
To ensure stable provision, the SSI will - for a period of time - provide Hexaxim® rather than Hexyon®.
Hexaxim® is provided in English/French/Spanish packaging with a corresponding package leaflet in packs of one. With each pack, the SSI will provide an information letter and a Danish package leaflet for Hexyon®.
The vaccine is ordered using Form 6 or item number 97935 or by contacting the SSI Order Office.
As Hexaxim® and Hexyon® (and Hexacima®) are different names for exactly the same product, they may be combined freely in the vaccination programme, in line with the guidelines described in EPI-NEWS 5/16.
As from May 2016, the vaccine is expected once again to be provided in Danish packaging under the name of Hexyon®. As from this time, the vaccine will be provided with a syringe.
(P. Valentiner-Branth, Department of Infectious Disease Epidemiology, G. Germod, Planning Division)
Link to previous issues of EPI-NEWS
13 April 2016