No 36 - 2016
Syphilis 2015
Measles cases in the Copenhagen area
Syphilis 2015
In 2015, Statens Serum Institut (SSI) recorded 777 cases of newly acquired syphilis in 742 persons. In addition to the 777 cases, a total of 234 cases were assessed as not newly acquired and they are therefore not included in this report.
A total of 705 (91%) were men and 72 (9%) were women. The median age was 41 years for men (range 17-80 years) and 32 years for women (range 17-62 years).
A total of 391 (50%) of the cases, 350 men and 41 women, were reported to the Notification System for Infectious Diseases (NSID), the Department of Infectious Disease Epidemiology (DIDE).
A total of 172 (22%) of the cases were both notified to the NSID and a specimen was submitted to the Department of Microbiological Diagnostics and Virology, SSI (DMDV), whereas 207 cases (27%) were notified to the DIDE and serologically confirmed at another laboratory not forming part of the SSI.
Furthermore, the NSID received 12 notifications (2%) for which there was no information about laboratory diagnostics, but in which it was not possible to dismiss current syphilis. A total of 386 (50%) were not notified to the NSID, 14 hereof were confirmed through full serological testing in the DMDV; and the remaining 372 cases were diagnosed at laboratories not forming part of the SSI. As in previous years, the majority of the patients resided in the Copenhagen area, Table 1.
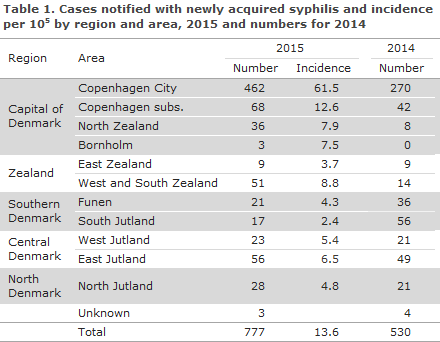
Compared with 2014, an increase of 247 cases was seen (47%), Table 1. The corresponding increase from 2013 to 2014 was 51%. The increase was seen in all areas, apart from Funen and South Jutland, where a disproportionately large number of cases was observed in 2014, EPI-NEWS 36/15.
Congenital syphilis and syphilis in pregnant women
No cases of congenital syphilis were notified in 2015, but syphilis antibodies were detected in two neonates whose mothers had tested positive to syphilis in the pregnancy screening. In both cases, it is probable that only maternal antibodies were found. Nevertheless, it was decided to treat the two children as their mothers had initiated treatment so late in the course of their pregnancy that a full treatment effect could not be guaranteed.
Among the 72 syphilis cases that were detected in women, 12 were found owing to the pregnancy screening, EPI-NEWS 35/16. In two of these cases, no notification had been made to the NSID. Seven of the pregnant women were of Danish origin, the remaining were from countries in Eastern Europe, Asia and Africa.
Transmission
The 391 cases that were notified to the DIDE occurred in a total of 383 persons, as eight men were notified with two syphilis episodes in the course of 2015.
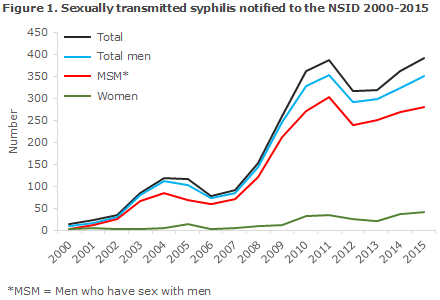
Among these 383 persons, 342 were men, including 54 who were notified as heterosexual transmission (16% of all notified men), 273 were notified as men who have sex with men (MSM, 80% of the notified men); and in 15 cases the mode of infection was not stated (4% of the notified men). Finally, a total of 41 heterosexually infected women were notified (11% of all notified cases). Figure 1 presents the number of persons notified with sexually transmitted syphilis since 2000.
A total of 319 (82%) of the notified persons were of Danish origin, whereas 66 (17%) were immigrants, 4 were second-generation immigrants and 2 were tourists. The 72 persons of non-Danish origin were from a total of 42 countries from all parts of the globe.
The country of infection was stated for 327 (84%) of those who had been notified, 288 men and 39 women. A total of 267 (93%) men and 33 women (85%) had become infected in Denmark. In all, 31 (94%) of the women who had become infected in Denmark were of Danish origin. Among heterosexually infected men, 44 (90%) were infected in Denmark, while this was the case for 215 (93%) MSM. A total of 18 other countries of infection were stated. The two most frequent countries were Germany (five men) and Spain (three men).
Syphilis and HIV
Information about HIV status was available for 325 (93%) men and 37 women (90%).
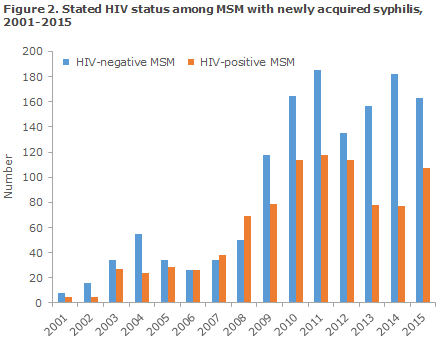
Among HIV-tested men, 112 (34 %) were HIV positives. In all, 107 HIV-positive men were found among 270 MSM (40%) and 2 among 46 heterosexually infected men (4%), and in 3 cases in which sexual orientation was not stated.
Among the 112 HIV-positive men, 9 (8%) had been diagnosed with HIV and syphilis simultaneously (8 MSM and 1 heterosexual), whereas 103 (92%) were known HIV positives prior to their current syphilis diagnosis (99 MSM, 1 heterosexual and 3 cases for whom sexual orientation was not stated). One non-Danish woman was a known HIV positive.
Among the eight MSM with newly diagnosed HIV, one had previously been notified with syphilis.
The share of HIV positives among MSM with syphilis has varied over time, Figure 2. The largest share was recorded in 2008 (58%), whereas the share has subsequently followed a decreasing trend, reaching 40% in 2015.
Frequency of notification
Among the recorded cases that were assessed as newly acquired syphilis, only 50% were notified to the NSID. In 2013, 91% were notified, EPI-NEWS 34/13; and in 2014, 68% were notified, EPI-NEWS 36/15. Thus, a considerable decrease in the share of notified cases has been observed in a short three-year time span. In 2013, virtually all confirmatory syphilis tests were performed at the SSI; in 2014, a total of 50% of the recorded cases were confirmed in a laboratory not forming part of the SSI; and in 2015 this share was 74%. The increase in the share of cases that are confirmed in laboratories not forming part of the SSI coincides with the decrease in the share of registered cases that are also notified to the NSID. Several circumstances may explain this.
The most obvious explanation is that the DMDV sends a notification form to the person ordering the test whenever the laboratory findings are consistent with current syphilis. This alone brings a high notification frequency. Thus, in 2015 a total of 172 of 186 cases (92%) who were diagnosed in the DMDV were also notified to the NSID. Even though the two Copenhagen-based laboratories that do not form part of the SSI expressly encourage the persons ordering tests with them to notify any confirmed cases, it is possible that enclosing a notification form constitutes an extra incentive for notification.
The Department of Infectious Disease Epidemiology cannot send out reminders concerning patients whose positive test results were established by laboratories not forming part of the SSI.
Commentary
Following a reduction in the number of syphilis cases in 2012, the condition is once again on the rise. The increase has been observed for both sexes and applies to both homosexually and heterosexually infected persons, but the occurrence of syphilis remains higher among MSM.
No cases of congenital syphilis were notified in 2015, but the general screening of pregnant women identified 12 women with newly acquired syphilis, including 7 women of Danish origin. It is therefore still important that the screening of pregnant women continues and that the pregnant women who screen positive to syphilis undergo full serological testing to ensure that the diagnosis may be confirmed or dismissed within the time period in which treatment may prevent infection of the foetus, EPI-NEWS 35/15, i.e. so early that sufficient treatment may be concluded no later than four weeks before the pregnant woman gives birth. An increase in the number of pregnant women with current syphilis is, of course, worrying and warrants close follow-up in the future.
Among MSM who were diagnosed with syphilis in 2015, 40% were HIV positives. The majority of these cases were known HIV positives and had been diagnosed with syphilis in connection with the regular HIV tests at an infectious medicine clinic. Eight percent of the MSM with syphilis who had been notified as HIV positives had been diagnosed with HIV and syphilis simultaneously. As sex without a condom may not only cause infection with syphilis, but also with HIV – and other sexually transmitted conditions – syphilis among HIV-negative MSM is a marker for behaviour that entails a risk of HIV infection. Due to their risk behaviour, HIV-negative MSM who contract syphilis repeatedly are at increased risk of contracting HIV compared with those who are only diagnosed with syphilis once.
This group is therefore an obvious candidate group for enhanced measures against HIV infection, EPI-NEWS 20-21/2015. It is important to establish that the use of condoms remains an important measure of prevention against syphilis and other sexually transmitted infections. Nevertheless, the use of condoms is not an expedient measure of prevention for everyone. In this context, it will probably soon be possible to give so-called pre-exposure prophylaxis (PrEP) against HIV. This is recommended by the WHO as well as the UNAIDS for persons at special risk of HIV as a supplement to the use of condoms.
In July 2016, the European Medicines Agency approved the medicinal product Truvada (which was previously only approved for treatment of HIV) for PrEP in the EU. As the patents of the two ingredients used in Truvada will not expire until 2018 and 2020, respectively, there is a need for funding of this expensive medicinal product, alternatively for approval of a similar, but more inexpensive pharmaceutical.
The share of the notified syphilis patients (particularly MSM) who has been tested for HIV is very high. This is encouraging, and it remains important that MSM who are tested for syphilis also be tested for HIV, EPI-NEWS 46/09, chlamydia, lymphogranuloma venereum (LGV), hepatitis B & C, and gonorrhoea.
PCR testing is expedient for detection of Treponema pallidum in chancre material and is often positive before any antibodies can be detected.
Less than half of the cases that were diagnosed at laboratories not forming part of the SSI were notified to the NSID. This seems to be due to the fact that the SSI can only contact the ordering doctors directly by sending them forms and reminders if the doctors have ordered their tests with the SSI.
Newly acquired syphilis, i.e. primary and secondary syphilis, is notified to the Department of Infectious Disease Epidemiology, Statens Serum Institut (SSI) on Form 1510.
As from July 2015, the full civil registration number (CPR of the patient needs to be stated on the form, whereby monitoring is improved. The new form also includes the questions that were previously stated on a separate white form from the SSI's syphilis laboratory and which, among others, facilitate staging. The latter form is therefore no longer used, which facilitates the work of the notifying physicians.
(S. Cowan, Department of Infectious Disease Epidemiology, S. Hoffmann, Microbiology and Infection Control)
Measles cases in the Copenhagen area
During admission to a regional hospital in the Copenhagen area, morbillivirus (measles) was detected in a urine sample drawn from a school-aged girl who had been on a tourist journey to Thailand. The patient who had received the first, but not the second MMR vaccine presented with symptoms of a bad cold the day after she returned to Denmark, but did not run a fever or experience photophobia until 8 days later.
The patient was admitted to the paediatric department twice, first on 27 August 2016 and then again on 29 August 2016. During the first admission she was admitted to a single-bed room and during the second admission she was isolated. Subsequently, the girl was discharged with clinical signs of improvement.
Contacts have been exposed at several occasions; at school, at a recreational club, at the hospital and in her GP's waiting room. Contact tracing was initiated at the time of the diagnosis as a collaborative effort counting the Danish Patient Safety Authority, Supervision and Guidance East (formerly The Medical Officers of Health East), the hospital and general practice.
Two unvaccinated exposed adults were identified and measles post-exposure prophylaxis was initiated on 31 August in the form of vaccination (< 3 days after exposure) and human immunoglobulin (>3 and <6 days after the exposure).
Genotyping has presently been performed on a urine sample from 29 August and the type is D8 and a 100% match to a type currently circulating in Asia, including Thailand.
Physicians in the Copenhagen area are now encouraged to pay extra attention to the diagnosis in children and younger adults with symptoms that are consistent with measles. It is important that any person who is suspected of having measles avoids being in waiting rooms with other patients as measles is extremely infectious.
For a detailed description of measles, please see the SSI's measles theme page.
Sampling
On suspicion of measles, the following samples should be taken:
- A blood sample for IgM/IgG antibody determination. IgM antibodies may be confirmed by rash.
- Pharyngeal swab and urine for virus detection (PCR). The greatest possibility for detecting measles virus is in the early phases of the disease course, but the virus is frequently detectable for several weeks after the acute disease occurs. A negative finding does not exclude measles.
We request that all measles-positive samples be sent to the National WHO Reference Laboratory for Morbilli and Rubella, Section for Virology Surveillance and Research, Statens Serum Institut for characterisation which is free of charge.
For further details, please see the SSI's measles theme page.
Vaccination and prophylaxis following exposure
The primary form of prevention is MMR vaccination. MMR vaccination is normally offered to all children at 15 months and four years of age (previously 12 years of age). As post-exposure prophylaxis (PEP), MMR vaccination may be given to non-immune contacts within three days and normal human immunoglobulin within six days after certain exposure to infection.
Certain exposure is defined as contact with a laboratory-confirmed or epidemiologically linked MMR case. Delimitation of contacts who need PEP is done by the on-duty physician at the Danish Patient Safety Authority, Division for Supervision and Guidance (formerly The Medical Officers of Health). Expenses are covered by the regional authorities.
For more details on prophylaxis, please see here.
Commentary
The current case underlines that physicians should be particularly attentive to the diagnosis in children and younger adults who present with symptoms that are consistent with measles, i.e. fever and a rash, in travellers who are returning from areas where measles still occur frequently.
The case also underlines the importance that persons who are under suspicion of having measles avoid staying in waiting rooms with other patients, whenever possible. Instead, these patients should be seen late in the day. If possible, house calls should be made. Furthermore, it is important that the doctors referring suspected measles cases to hospital inform the hospital of the suspicion so that the patient may be isolated immediately upon arrival.
Please note that the best possible protection is achieved after two MMR vaccinations. Most of the people who do not achieve immunisation after their first vaccination will be immunised after their second vaccination. If a person has not been vaccinated in accordance with the age-criteria of the childhood vaccination programme, the person should be offered immunisation. The MMR vaccine is free of charge for all persons below 18 years of age.
Measles cases complying with the disease definition, i.e. cases that are laboratory-confirmed or epidemiologically linked to such a case, are notifiable to the Department of Infectious Disease Epidemiology at SSI and to the Danish Patient Safety Authority, Division for Supervision and Guidance (formerly The Medical Officers of Health).
To underpin the preventive efforts, notification shall be done as soon as possible and preferably at the time of diagnosis as described in the above case. In the amended executive order on notification of infectious diseases, measles will become notifiable by phone. Until the executive order comes into force, you may e.g. notify by sending a fax (using Form 1515) to the Danish Patient Safety Authority, Division for Supervision and Guidance while also sending the notification by surface mail.
(R.M. Pedersen, L.D. Rasmussen, Virology Surveillance and Research, P.H. Andersen, Department of Infectious Disease Epidemiology, N.H. Nielsen, the Danish Patient Safety Authority, Supervision and Guidance East)
Link to previous issues of EPI-NEWS
7 September 2016