No 35 - 2016
Hepatitis B, HIV and syphilis screening of pregnant women, 2015
Hepatitis B, HIV and syphilis screening of pregnant women, 2015
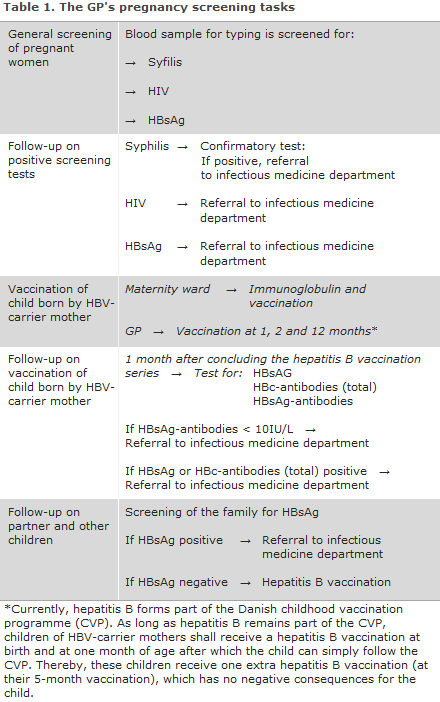
General screening of pregnant women for hepatitis B was introduced on 1 November 2005, EPI-NEWS 41/05, while screening for HIV and syphilis was initiated as from 1 January 2010, EPI-NEWS 27-33/10. The general practitioner's tasks in relation to the screening are presented in Table 1.
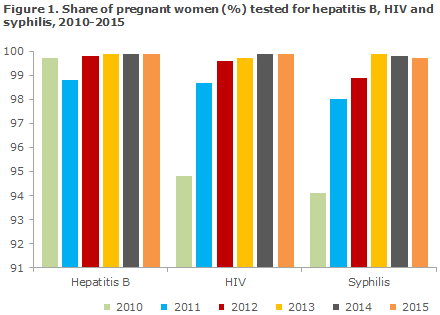
In 2015, a total of 65,942 blood type analyses were performed in pregnant women. Among these women, 65,890 (99.9%) were tested for hepatitis B, 65,850 (99.9%) for HIV and 65,764 (99.8%) for syphilis, Figure 1.
A very limited number of women decline having the tests made, and laboratory error accounts for the majority of missing tests.
Pregnant women with hepatitis B infection
Of the 65,890 tests, a total of 187 were positives (0.28%), which is at par with the level observed in previous years. A positive HBsAg (hepatitis B surface antigen) indicates either current or chronic hepatitis B virus (HBV) infection
Among these, 86 (46%) women tested positive to HBsAg for the first time in 2015. The Department of Infectious Disease Epidemiology sends out reminders for notification of HBV if no current or previous notification has been made. Therefore, all pregnant HBsAg positives were notified with the statutory national notification system in 2015.
The remaining 101 women (54%) had previously tested HBsAg positive.
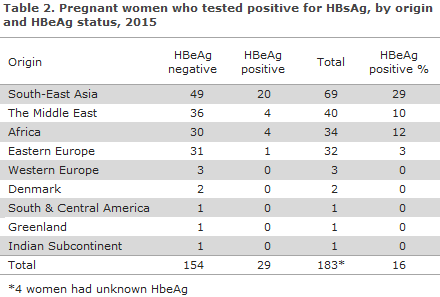
HBeAg, a marker for disease activity associated with an increased risk of intrauterine mother-to-child infection, was detected in 29 (16%) of the women.
As in previous years, the majority of the HBeAg-positive women were from South-East Asia (apart from in 2013, when the majority of HBeAg-positives were from the Middle East), Table 2. Only two women (1%) were of Danish origin; none of them were HBeAg-positive.
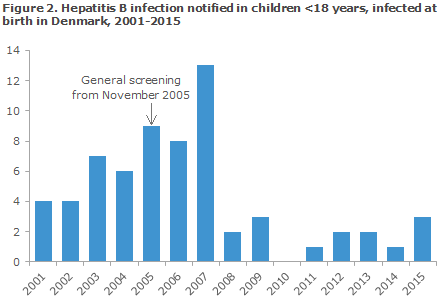
The general screening for hepatitis B has been in place since 2005, and the number of children infected with hepatitis B at birth in Denmark has decreased considerably, Figure 2. In 2015, three children below 18 years of age were notified as having been infected at birth in Denmark; all three were born before the introduction of the pregnancy screening and were of South-East Asian origin. Among the remaining children who were notified with HBV after 2005, three were infected at birth after the introduction of screening.
HIV-positive pregnant women
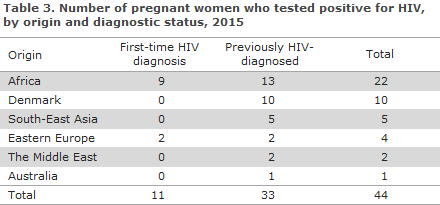
Among 65,850 HIV tests, 44 (0.07%) were positives.
A total of 11 women had newly detected HIV and 33 were known HIV positives.
All were from other countries than Denmark, including nine from Africa and two from Eastern Europe, Table 3. Four had arrived in Denmark in 2015 (including two with no CPR number), four had arrived in 2014, one in 2012 and, finally, two had been residing in Denmark since 2001 and 2003, respectively.
All newly detected HIV positive women were notified via the statutory national HIV notification system.
No children were notified as infected at birth in Denmark in 2015.
Pregnant women with syphilis
Among the 65,764 syphilis screening tests, a total of 128 were positives. The majority of these were false positives or had antibodies from previous syphilis. The confirmatory test makes it possible to identify both the false positives/previously infected cases and the pregnant women who currently have syphilis. Confirmatory serological tests were performed in 125 of the women (98%). Current syphilis was established in 12 of these cases, corresponding to 0.02% of all screened pregnant women. Additionally, in one woman, latent infection could not be excluded. Her child was not infected at birth.
The 12 positives included seven Danes, two East Europeans, one woman from Thailand, another from Indonesia and, finally, the origin of one woman was not stated. Ten of the 12 women were notified via the statutory national syphilis notification system. Three women did not have the confirmatory test performed despite several requests from the SSI to do so.
No cases of congenital syphilis were notified in 2015, but syphilis antibodies were detected in 2 neonates whose mothers had tested positive to syphilis in the pregnancy screening. In both cases, it is probable that only maternal antibodies were found. Nevertheless, the two children received treatment as their mothers had initiated treatment so late in the course of their pregnancy that a full treatment effect could not be guaranteed.
Commentary
The general screening of pregnant women may still be considered a success. Not only are nearly all cases of mother-to-child infection with the three conditions prevented in Denmark; pregnant women who were unaware that they had become infected can be tested and treated. It is, however, only those pregnant women who are examined by a physician during their pregnancy who can make use of this offer.
Those pregnant women who stay in the country illegally may be examined by a physician at a Red Cross health clinic in Copenhagen or Aarhus. Here, pregnancy screening is also offered, but this service does not form part of the public offer of care for childbearing women. If a woman in labour of unknown status arrives at a maternity ward, the ward shall perform tests for syphilis, hepatitis B and a rapid HIV test.
Two of 12 women who gave birth without having been screened had hepatitis B. This finding underlines the importance of the test. Tests made in connection with parturition disclosed no HIV or syphilis positives who had not already been detected by screening.
In 2015, a considerable share (7 out of 12) of the pregnant women with syphilis was of Danish origin. This shows that syphilis is not exclusively a condition that occurs among homosexual men; it has been re-introduced among heterosexuals.
As the syphilis screening tests made among pregnant women produce many false positive test results, a full serological testing is required of anyone who tests positive in the screening.
It is important that the treating physicians refer any pregnant women who have been diagnosed with one of the three infections in the screening to the relevant specialist departments, even if the woman in question has no symptoms of infection, Table 1. In pursuance of the Danish Health Authority's guideline on general screening of pregnant women for infection with hepatitis B, HIV and syphilis, the pregnant woman's partner and remaining children should have blood tests performed.
In the most recent guideline on HIV, hepatitis B and C virus published in 2013, the Danish Health Authority recommends that all children born by carrier mothers who receive hepatitis B vaccination at birth and subsequently at the GP should be tested to confirm that the vaccination has taken and to test for current infection one month after the vaccination series has been concluded, i.e. when the child is 13-15 months old.
This recommendation is based on studies demonstrating that inter-uterine infection does occur in some children, in which case the vaccine is ineffective. It is the responsibility of the GP to perform this test. If the child has become infected or is insufficiently protected despite the vaccinations, the child is referred to a specialist department.
(N. Mellerup, A.H. Christiansen, S. Cowan, the Department of Infectious Disease Epidemiology, S. Hoffmann, Microbiology and Infection Control)
Link to previous issues of EPI-NEWS
31 August 2016