No 36 - 2015
Syphilis 2014
Outbreak of polio-like disease in the Ukraine
Syphilis 2014
In 2014, Statens Serum Institut (SSI) recorded 530 cases of newly acquired syphilis in 523 persons. In addition to the 530 cases, a total of 285 cases were registered but were assessed as non-current and they are therefore not included in this report.
A total of 476 (90%) were male and 54 (10%) were female cases. The median age was 40 years for men (range 17-79 years) and 30 years for women (range 0-54 years).
A total of 358 (68%) of the cases were notified to the Notification System for Infectious Diseases (NSID), the Department of Infectious Disease Epidemiology. A total of 205 (39%) of the cases were both notified to the NSID and a specimen had been submitted to the Department of Microbiological Diagnostics and Virology, SSI (DMDV), whereas 123 cases (23%) were notified to the DIDE and diagnostically confirmed at another laboratory not forming part of the SSI.
Furthermore, the NSID received 30 notifications (6%) for which there was no information about laboratory diagnostics, but in which it was not possible to dismiss current syphilis. Additionally, 30 cases (6%) had been diagnostically confirmed in the DMDV, but had not been notified to the NSID, and 142 cases (27%) which had been diagnosed in a laboratory not pertaining to the SSI, but had not been notified to the NSID. As in previous years, the majority of the patients resided in the Copenhagen area, Table 1.
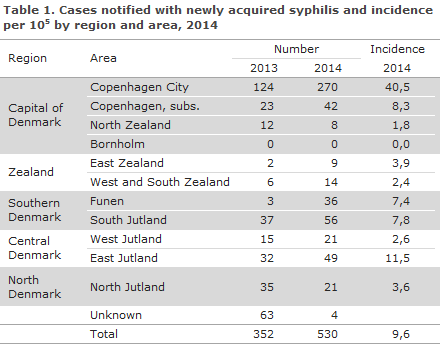
Compared with 2013, an increase of 178 cases was seen, corresponding to 51% more cases in 2014. The increase was seen in nearly all parts of Denmark.
Syphilis Diagnostics
Among the 235 syphilis cases in which samples were submitted to the DMDV, 167 (71%) were detected by serology, 26 (11%) by serology as well as PCR, and 42 (18%) cases were detected by PCR exclusively.
Congenital syphilis
No cases of congenital syphilis were notified in 2014, but syphilis antibodies were detected in 2 neonates whose mothers had tested positive to syphilis in the pregnancy screening. In both cases, the antibodies detected in the newborn were probably only maternal antibodies. Nevertheless, the two children received treatment as their mothers had initiated treatment so late in the course of their pregnancy that a full treatment effect could not be guaranteed.
Transmission
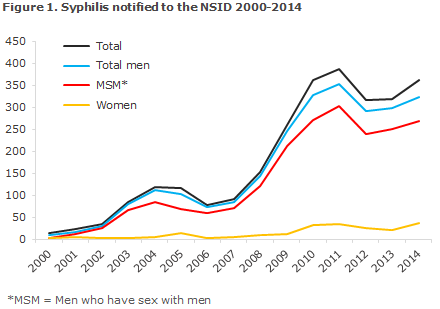
The 358 cases that were notified to the DIDE occurred in a total of 355 persons, as 3 men were notified with two syphilis episodes in the course of the year. Among these 355 persons, 318 were men, including 40 notified as heterosexual transmission (13% of all notified men), 264 notified as men who have sex with men (MSM, 83% of the notified men); and in 14 cases the mode of infection was not stated (4% of the notified men). Finally, a total of 37 heterosexually infected women were notified (10% of all notified cases). Figure 1 presents the number of persons notified with sexually transmitted syphilis since 2000.
A total of 297 (84%) of the notified persons were of Danish origin, whereas 51 (14%) were immigrants, 5 (1%) were second-generation immigrants, and 2 (1%) were tourists. The 58 persons of non-Danish origin were from a total of 30 countries from all parts of the world.
The country of infection was stated for 300 (84%) of those who had been notified, 270 men and 30 women. Among men, a total of 234 (87%) were infected in Denmark, and among women the corresponding number was 20 (67%), including 17 Danes. Among heterosexually infected men, 24 (72%) were infected in Denmark, while this was the case for 203 (89%) of MSM. A total of 28 other countries of infection were stated. The two most frequently stated countries were USA (7 men) and Thailand (5 men and 1 woman).
Syphilis and HIV
Information on HIV status was available for 302 men (97% of MSM, 90% of heterosexually infected men and 79% of men for whom the mode of infection was not stated), and for 30 (81%) women.
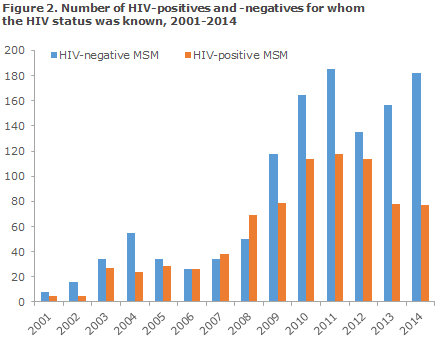
Among HIV-tested men, 77 (25%) were HIV positives. A total of 74 HIV positives were detected among 255 MSM (29%), 2 HIV positives were found among 36 heterosexually infected men (6%), and the mode of infection was unknown for the last HIV-positive man. Among the 77 HIV-positive men, 10 (13%) had been diagnosed with HIV and syphilis simultaneously (all MSM), whereas 56 (73%) were known HIV positives prior to their current syphilis diagnosis (53 MSM, 2 heterosexuals and in 1 case the mode of infection was not stated). For the remaining 11 (all MSM), there was no information on the time of HIV diagnosis. One non-Danish woman was a known HIV positive.
The share of HIV positives among MSM with syphilis has varied over time, Figure 2. It peaked in 2008, when the share of HIV positives among MSM was 58%. Since then it has maintained a decreasing trend, and in 2014 the share was 30%.
Commentary
Following a decrease in the number of syphilis cases in 2012, the number of syphilis cases is once again increasing, even though the number of cases is not quite as high as in 2011. The increase has been observed for both sexes and applies to both homosexually and heterosexually infected persons, but the occurrence of syphilis remains far higher among MSM.
No cases of congenital syphilis were notified in 2014; but in the general pregnancy screening, a total of 18 syphilis positives were detected, EPI-NEWS 35/15, which is the highest number since the syphilis test was introduced into the general screening of pregnant women in 2010. The increasing number of pregnant women testing positive to syphilis in the pregnancy screening and the fact that 20 women (including 17 Danes) were registered as infected with syphilis in Denmark in 2014 indicates that syphilis has now been introduced into heterosexual circles in Denmark.
In 2014, 30% of the MSM with syphilis were also HIV positives. The majority of these were known with HIV and were diagnosed with syphilis in connection with the regular HIV check-ups at infection medicine clinics, but 13% of the MSM with syphilis who were notified as HIV positives had been diagnosed with HIV and syphilis simultaneously. Syphilis among HIV-negative MSM is a marker for risk behaviour, because condom-free sex cannot only transmit syphilis, but also HIV (and the remaining sexually transmitted diseases).
HIV-negative MSM who contract syphilis repeatedly are at an increased risk of contracting HIV compared with those who are only diagnosed with syphilis once. This group is therefore an obvious candidate group for enhanced measures against HIV infection, EPI-NEWS 20-21/2015. In this context, it will probably soon be possible to give so-called pre-exposure prophylaxis (PrEP) against HIV. This is recommended by the WHO as well as the UNAIDS for persons at special risk of contracting HIV as a supplement to condoms, which for some people is not anexpedient prophylactic measure.
The share (particularly among MSM) who has been tested for HIV is very high. This is encouraging, and it is still important that MSM who are tested for syphilis also be tested for HIV, EPI-NEWS 46/09, lymphogranuloma venereum (LGV), hepatitis B & C, and gonorrhoea.
PCR testing is expedient for detection of Treponema pallidum in chancre material and is often positive before any antibodies can be detected.
Correct diagnosis and staging are important for the treatment of the individual syphilis patient as well as for monitoring efforts. Tentative diagnoses based on positive serological screening results should therefore be verified through extended serological tests. It is particularly important that pregnant women who are screened for syphilis receive full serological testing so that their diagnosis may be confirmed or dismissed within the relative short time period within which treatment may prevent transmission to the foetus, EPI-NEWS 35/15.
A fourth of the cases diagnosed in other places than the SSI were not notified to the NSID. The greater the share of diagnosed cases is notified, the better the epidemiological monitoring will be.
Newly acquired syphilis, i.e. primary and secondary syphilis, is notified to the Department of Infectious Disease Epidemiology, Statens Serum Institut (SSI) on Form 1510, which is available for download at www.ssi.dk.
As from July 2015, the full civil registration number (CPR) of the patient needs to be stated on the form, whereby monitoring is improved. The new form also includes the questions which previously were stated on a separate white form from the SSI's syphilis laboratory and which, among others, facilitate staging. The latter form is therefore no longer used, which eases the work of the notifying physicians.
(S. Cowan, A. H. Christiansen, Department of Infectious Disease Epidemiology, S. Hoffmann, Microbiology and Infection Control)
Outbreak of polio-like disease in the Ukraine
Two children from South-West Ukraine have presented with symptoms of infant paralysis (poliomyelitis) caused by a special polio virus.
The two children aged 4 years and 10 months, respectively, were affected by a polio-like disease already on 30 June and 7 July 2015. It has now been determined that their condition was caused by a vaccine strain of type 1 poliovirus, which has reacquired its disease-causing properties.
The WHO is in dialogue with the national Ukrainian health authorities to implement several national vaccination campaigns as soon as possible covering all children below 5 years of age with a view to curbing the outbreak.
The cases occurred in Zakarpatskaya Oblast in South-Western Ukraine, which borders on Romania, Hungary, Slovakia and Poland. The WHO assesses that the risk of spreading within Ukraine is high, but that the risk of spreading beyond the borders of Ukraine is currently low.
So-called circulating vaccine-derived polio viruses (cVDPV) are well-known and originate from populations with an insufficient vaccination coverage. The vaccine strain - which is taken orally and then excreted in faeces - can therefore circulate in the population and slowly reacquire the ability to cause polio. In 2015, this was also seen in Madagascar, where a total of 9 cases of cVDPV had been detected by 7 July.
Ukraine has been at increased risk of outbreaks of infectious diseases due to low vaccination coverage for a considerable period of time. Thus, in 2014 only half of all children received full polio vaccination and other vaccine-preventable conditions.
All travellers to areas where polio occurs should be fully vaccinated against polio in a manner equivalent to the vaccinations provided in the Danish childhood vaccination programme. It has yet to be established whether the WHO will introduce recommendations on polio vaccination for travellers from Ukraine like those currently in place for travellers from a series of countries where polio occurs, primarily Pakistan and Afghanistan, EPI-NEWS 26a+b/15.
(P.H. Andersen, Department of Infectious Disease Epidemiology)
Link to previous issues of EPI-NEWS
2 September 2015