No 20/21 - 2015
Hiv 2014
Measles outbreak in North Zealand
Hiv 2014
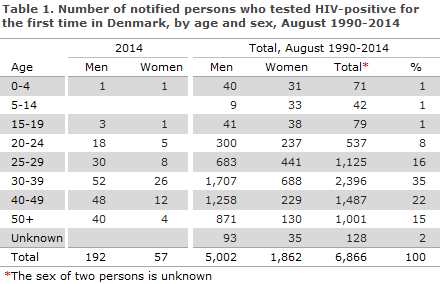
2014 saw a total of 249 notified cases of HIV in 192 men and 57 women, Table 1.
Among the 249 notified cases, 50 had previously been diagnosed with HIV abroad, including 9 Danes. Among the 50 previously diagnosed (34 men and 16 women) persons, 2 were cases of mother to child transmission (MTCT), 18 were homosexually infected (MSM), 23 were heterosexually infected (HTX), 2 were infected via intravenous drug use (people who inject drugs (PWID)) and in 5 cases the mode of infection was unknown or other.
Additionally, 7 tourists were notified, 5 men and 2 women. Two were MSM, 4 HTX and in one case the route of infection was unknown.
Among the 192 non-tourists (153 men and 39 women) who were diagnosed with HIV for the first time, 118 (61%) were Danes (including 5 second-generation immigrants and one adoptee), and 74 (39%) were immigrants, including 3 who had been trafficked and/or were staying illegally in Denmark. Among the 74 immigrants, 32 (43%) were from Sub-Saharan Africa, 12 (16%) from Eastern Europe including Russia, 10 (14%) from Western Europe, 8 (11%) from Southeast Asia, 8 (11%) from the Middle East and Northern Africa, 2 (3%) from South America and 1 (1%) from Greenland and Oceania, respectively.
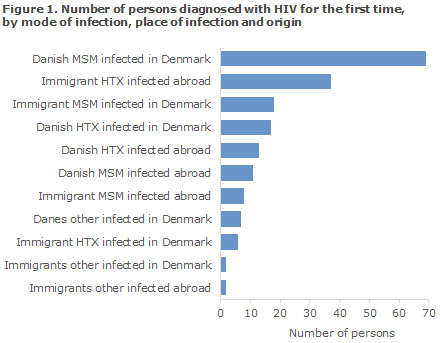
A total of 106 were MSM, 74 HTX and 9 PWID. One case of mother-to-child-transmission was observed. In two cases, the mode of infection was unknown. A total of 119 (62%) were infected in Denmark and 71 (37%) abroad, Figure 1. In 2 cases (1%), the country of infection was not stated. The median age was 38 years for men (range 0-72 years) and 35 years for women (range 20-87 years).
Among 44 heterosexually infected immigrants, 30 (68%) were from Sub-Saharan Africa, 5 (11%) from South-East Asia, 4 (9%) from the Middle East, 4 (9%) from Eastern Europe and 1 (2%) from Western Europe.
Among the 26 homosexually infected immigrants, 9 (35%) were from Western Europe, 6 (23%) from Eastern Europe, 4 (15%) from the Middle East, 3 (11%) from South-East Asia, 2 (8%) from South America, 1 (4%) from Oceania and 1 (4%) from Sub-Saharan Africa.
Figure 2 shows the de development in mode of infection from 2015 to 2014; and the detailed distribution on origin, mode of infection and place of infection are presented in Table 2.
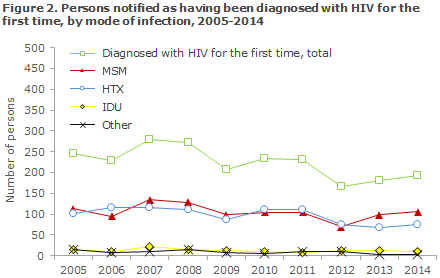
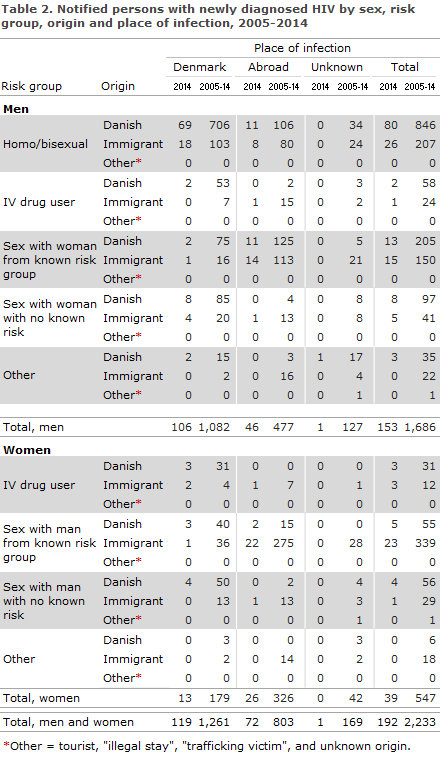
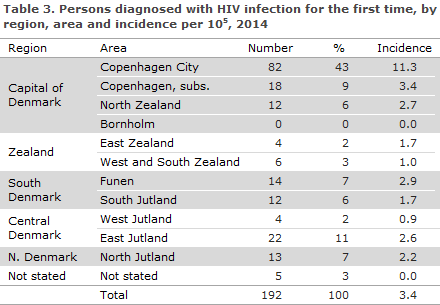
Table 3 shows the distribution by area and region. A total of 112 (58%) resided in the Capital Region of Denmark.
Perinatally infected persons
One neonate boy was notified as perinatally infected, his mother had tested negative to HIV in the pregnancy screening, but she contracted the infection later in pregnancy. This was only discovered when the woman presented with symptoms consistent with acute HIV shortly after giving birth, and both mother and child then tested positive to HIV, EPI-NEWS 23/14.
Danish men
Of the 106 Danish men, 80 (75%) were MSM, 69 (86%) of whom had been infected in Denmark. A total of 21 (20%) were HTX, including 11 (52%) who were infected abroad (7 in Thailand, 2 in Europe and 1 in Africa and the Philippines, respectively). Two (2%) were infected via PWID in Denmark. In 2 cases, the mode of transmission was not stated. Additionally, the group counts one immigrant child who was described above in the section on perinatally infected persons.
Danish women
Ten of 12 Danish women were infected in Denmark and 2 in Africa. Nine women were heterosexually infected. Three were infected through PWID. Three women were detected in the pregnancy screening, one who had been infected by a bisexual partner, one by an African man, and 1 was a former PWID.
Immigrant men
Of the 47 immigrant men, 26 (55%) were MSM, 18 (69%) of whom had been infected in Denmark. A total of 20 (43%) were HTX, of whom 5 (25%) were infected in Denmark. One (2%) was infected via PWID abroad.
Immigrant women
A total of 27 immigrant women were notified with HIV. Of these, 24 were infected via HTX, including 1 (4%) in Denmark. Additionally, 3 had been infected through PWID; 2 in Denmark and 1 abroad. Nine women (33%) were detected through the pregnancy screening.
CD4 count at diagnosis
Among the 192 notified persons who had an address in Denmark and who were diagnosed with HIV for the first time, information on CD4 count at the time of diagnosis was available for 169 (88%). In the remaining 23 cases, CD4 counts were unavailable.
The CD4 count is a marker that indicates how the HIV virus affects the cellular immune response. A CD4 count below 350 cells per µl blood is currently indication for initiation of highly active antiretroviral therapy (HAART) in Denmark if the patient has not wanted to initiate such treatment earlier.
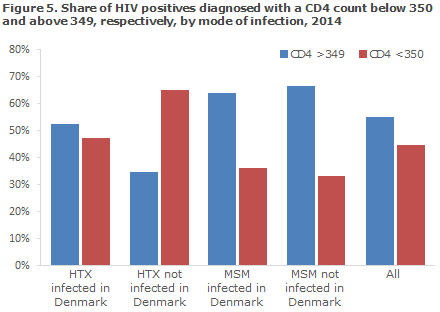
Among the 169 for whom the CD4 count was stated, there were 76 (45%) whose CD4 count was below 350 cells per µl at their diagnosis, including 15 persons assessed as newly-infected based on primary HIV disease and/or a recent negative HIV test, whereas 93 (55%) had CD4 counts of 350 or above.
Among 101 MSM for whom the CD4 counts were stated, the share with a CD4 count > 349 at diagnosis was 65%, whereas it was 40% among 60 HTX. On the basis of the information on CD4 counts at diagnosis, previously negative tests and acute HIV disease, the time from infection to diagnosis was estimated.
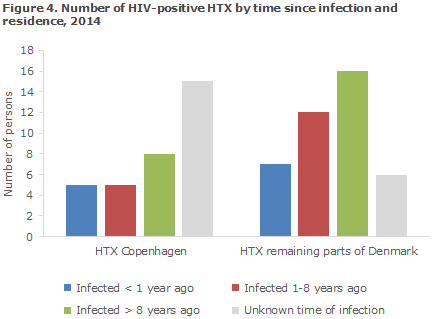
If information was available on acute HIV disease and/or a negative test within a year, the patient was assessed as having been "infected within 1 year"; if there was information on AIDS and/or a CD4 count below 200, the patient was assessed as having been "infected more than 8 years ago".
If no information was available concerning a test within 1 year or about AIDS and the patient's CD4 count was above 200, the person was assessed as having been "infected 1-8 years ago". Figure 3 shows the distribution by estimated time until diagnosis for MSM in the Copenhagen area and remaining parts of Denmark, respectively, and Figure 4 presents the distribution among HTX.
The number of HTX for whom the amount of information was insufficient for calculation of the infection period was considerably higher than for MSM. This is due to lacking information on CD4 counts and the fact that only a limited number of HTX had active HIV disease at the time of their diagnosis and/or a recent negative HIV test.
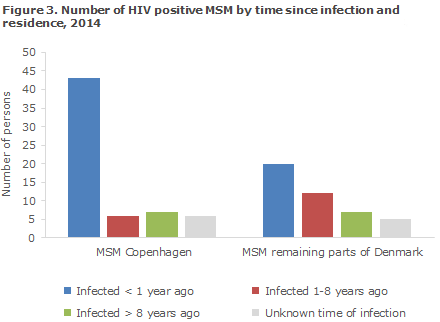
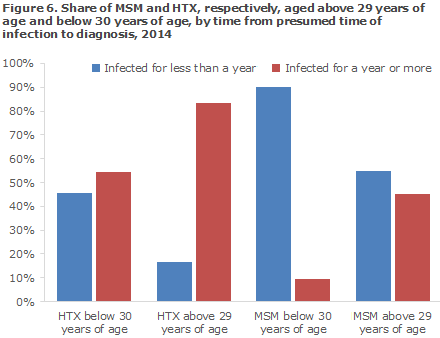
Younger MSM had typically been tested shortly after the presumed time of infection. Thus, 90% of MSM below 30 years of age were estimated to have been infected less than 1 year prior to their diagnosis (based on previous negative tests, symptoms of acute HIV disease and their CD4 counts at diagnosis), compared with MSM above 29 years of age among whom 55% were diagnosed early.
Similarly, among HTX the share of younger (45%) persons who were diagnosed early was higher than the share of elderly (17%) who were diagnosed early.
AIDS
Among 192 newly-diagnosed cases, a total of 24 (13%) were diagnosed with aids simultaneously, including 14 HTX, 9 MSM and 1 PWID.
An additional 9 persons were notified with AIDS; 1 had been diagnosed with HIV within the past year, 4 had been diagnosed with HIV 1-6 years earlier and 4 had been diagnosed with HIV more than 13 years earlier.
Checkpoint
A total of 22 of the 192 notified (11%) cases had been tested at a Checkpoint (the Danish AIDS Foundation's test sites for MSM and immigrants where you can be tested for HIV and syphilis without scheduling an appointment and where you will receive the results immediately), including 19 MSM and 3 immigrant-HTX from Sub-Saharan Africa. An additional 6 MSM tested positive at a Checkpoint, including 5 persons who re-sided in Denmark and who had not been notified to the Department of Infectious Disease Epidemiology even though the Department had sent several enquiries to the 2 departments of infectious disease to which the patients had been referred for confirmatory testing.
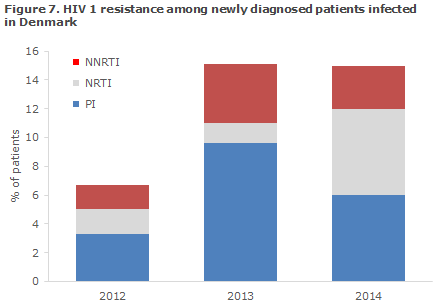
Transmitted resistance in persons with newly diagnosed HIV
In 2014, the Section for Virology Surveillance and Research diagnosed a total of 10 new cases of transmitted, resistant HIV, corresponding to 15% of all the tested newly diagnosed patients infected in Denmark. The prevalence of transmitted resistance has thus increased in the period from 2012 to 2013-2014, Figure 7.
In 2014, the resistance mutations were distributed on all three primary antiretroviral (ARV) treatment groups used for highly active antiretroviral therapy (HAART): 2 patients (3%) were resistant to non-nucleoside inhibitors (NNRTI), 4 patients (6%) were resistant to nucleoside inhibitors (NRTI), and 2 patients (6%) were resistant to protease inhibitors (PI)
No patients were resistant to more than one treatment group, and all were therefore susceptible to a minimum of 2 ARV treatment groups. The 2012-2014 period recorded a total of 25 patients with treatment resistance. A total of 24 of these were of subtype B and 1 was CRF01_ AE; both of these subtypes are endemically transmitted types in Denmark (see the section on HIV subtypes).
The period has not seen any changes in the molecular diagnostics or sequencing analysis that can explain the increase in the prevalence of resistance. The causes explaining the increases may be changes in the prevalence and/or transmission of resistant HIV from patient groups other than the newly diagnosed ones, but other causes cannot be excluded.
The report comprises all newly diagnosed HIV patients who are referred to a department of infectious diseases and have a genotypic resistance test performed within 1 year after diagnosis and prior to treatment initiation. Between 40% and 50% of the newly diagnosed HIV patients are every year enrolled in this study, corresponding to approximately 120 patients annually. The presented data only include persons known to have been infected in Denmark. From this subgroup, sequences were used from 60, 73 and 67 patients infected in 2012, 2013 and 2014, respectively.
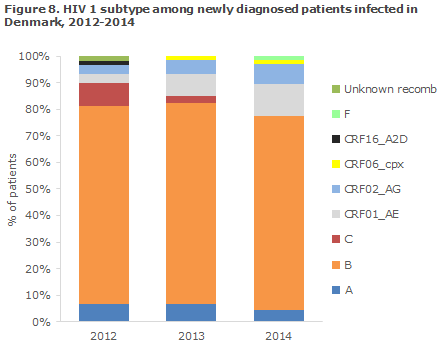
HIV subtypes among newly diagnosed patients infected in Denmark
Among newly diagnosed HIV-1 patients who have been infected in Denmark, HIV 1 of subtype B comprised 73% in 2014, Figure 8. Subtype A and B and the two recombinant forms CRF01_AE and CRF02_AG were seen every year in 2012, 2013 and 2014.
These HIV 1 subtypes/recombinants are therefore endemically transmitted in Denmark with an average prevalence of: 5% for A, 75% for B, 6% for CRF01_AE and 5% for CRF02_AG. These subtypes and recombinants are also among the most frequently observed in the remaining European countries.
Commentary
Like last year, this year's annual HIV report only includes persons who were diagnosed for the first time. That means that the report excludes persons who are known HIV positives because they have been diagnosed abroad. Furthermore, AIDS is not described in a separate report, but treated as part of the HIV disease, EPI-NEWS 37/14.
The number of notified HIV cases in 2014 was in line with those recorded in the previous years, and MSM and immigrants who were HTX infected with HIV before their arrival to Denmark remained the largest infection groups. The third-largest group was homosexual immigrant men, who were infected in Denmark. In contrast to heterosexual immigrants who were primarily from Sub-Saharan Africa and South-East Asia, MSM were mainly from Western and Eastern Europe, and to some extent from the Middle East. This difference in the distribution should inform the preventive efforts among MSM, where homosexual immigrant men seem to comprise an increasing share.
The Checkpoint continues to account for a considerable share of the notified cases, and it causes concern that 5 people who were residing in Denmark had not been notified from the 2 infectious disease departments to which they had been referred for confirmatory testing. It is to be expected that the HIV diagnosis will often be made using a rapid test that is subsequently confirmed through RNA analysis. We emphasise that HIV diagnosed by use of the latest methods is also notifiable, and that the epidemiologic surveillance is based on high notification rates from the clinics.
The large share of MSM who was diagnosed as having been newly infected indicates that the message concerning frequent testing has gained foothold. Additionally, it is a symptom of a considerable and continued spreading of the infection, which it has not been possible to contain through the prophylactic measures presently in use. Rethinking of the prophylactic measures employed among MSM is warranted, not least in view of the increasing HIV infection incidences that are observed in this group in several other European countries.
Both the WHO and UNAIDS recommend medical prevention of HIV, so-called pre-exposure prophylaxis (PrEP), for persons who are at a special risk of becoming infected with HIV. We will likely witness debate to determine how such an - expensive - preventive measure may be implemented in Denmark, provided PrEP is approved as an indication for antiretroviral (ARV) treatment in the EU, and to determine which groups should receive such treatment. One obvious candidate group for PrEP may be MSM who are diagnosed repeatedly with syphilis. Hence, in Denmark it has been shown that having several consecutive syphilis diagnoses increases the risk of being diagnosed with HIV considerably.
That only few cases of HIV are recorded in other groups apart from MSM is a positive sign and an indication that MSM should be the focus for any preventive measures. Particularly, it is encouraging that HIV-positive immigrant HTX only transmit the infection to a limited degree after their arrival to Denmark.
In this group, the efforts should focus on early diagnosis and treatment, not least because, logistically, it is much simpler to offer test and treatment immediately after the immigrant's arrival to Denmark than trying to identify new citizens with a view to testing them at a later date. The pregnancy screening, among others, shows that HIV-positive women have stayed in Denmark for several years before being diagnosed thanks to the offer of testing for all pregnant women, EPI-NEWS 23/14.
Among the newly diagnosed HIV-positives who had been infected in Denmark, 15% of the tested persons had transmitted resistance (TR) to 1 of the 3 primary ARV treatment groups that are used for highly active antiretroviral therapy (HAART). Even though no-one was resistant to several groups and therefore constituted no problem in relation to effective treatment, it is thought-provoking that TR follows an increasing trend in Denmark where we have hitherto recorded a lower TR than countries with which we are usually compared, EPI-NEWS 48/12.
A CD4 count below 350 at diagnosis is an established target for the identification of so-called late testers, i.e. persons who have been infected for a considerable period of time without being tested. In 2014, data indicating that the person was newly infected were available for 15 of the 76 persons notified with CD4 counts below 350.
This discrepancy is of no relevance in the clinical work as the physicians can easily distinguish newly infected persons from late testers, but it may potentially skew the surveillance, particularly when a large share of the persons are diagnosed while they are newly infected during which period the CD4 count often shows a non-permanent drop. It is encouraging that the physicians generally state the relevant information on the HIV notifications.
(A.H. Christiansen, S. Cowan, Department of Infectious Disease Epidemiology, J. Fonager, Virology Surveillance and Research)
Measles outbreak in North Zealand
In the course of the past 2 weeks, a total of 6 cases of measles have been diagnosed in North Zealand. Figure 9 shows the epi curve for the 9 cases which were detected in 2015 until now.
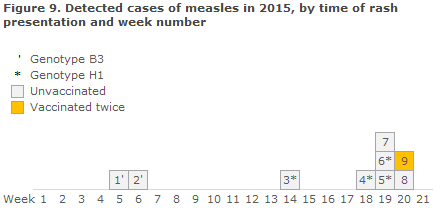
In the beginning of May, the condition was detected in a 3-year-old unvaccinated child, and subsequently another 4 cases have been diagnosed in the same family, including 3 cases in children aged 0-10 years, all unvaccinated. Genotyping of virus isolated from the first case is of the H1 type, which is identical to a measles virus that has caused a major measles outbreak in China.
The genotype is nearly 100% identical to the genotype H1 that was isolated from an adult Dane who was infected with measles during a stay in China in late March 2015, and who fell ill in the beginning of April, EPI-NEWS 16/15.
It has not been possible to establish any contact between these 2 cases, and an intermediary, undiagnosed patient may exist because the distance in time between these 2 cases is equivalent to slightly more than 2 average-length incubation periods (10 days, range 7-18 days). Typing of virus isolated from 2 of the 4 family members is also of the H1 genotype. Typing of measles from the two final cases is in course.
This week saw the diagnosis of yet another measles case in a young adult registered as having received 2 doses of MMR vaccine. The case can be linked epidemiologically to the 3-year-old child during the child's admission to hospital in the beginning of May. Typing of measles virus from this patient is pending.
Infection tracing is currently being undertaken by the Medical Officer of Health with a view to determining the vaccination status among contacts and possibly offering post-exposure prophylaxis. Vaccination is recommended as prophylaxis for unvaccinated persons who have been exposed to known infection within 72 hours.
According to the summary of product characteristics, the MMR vaccine may be used as from 9 months of age, but several international studies have documented that the majority of children of vaccinated mothers do not have measurable levels of measles antibodies as from 6 months of age, and therefore the vaccine may be used off-label already from this age.
If the MMR vaccination is given before 12 months of age, the vaccination shall be repeated when the child reaches the age at which the first dose of MMR vaccine is normally given (15 months).
Injection with human normal immunoglobulin (e.g. Beriglobin) may be given as prophylaxis or to weaken the disease for up to 6 days from the exposure to measles infection. Immunoglobulin may be used as from birth if it is to be expected that the child has not received antibodies from the mother.
Protection against measles following exposure to infection is no longer a registered indication for the available immunoglobulin drugs, and the content of measles antibodies is probably lower now than previously as the drugs are now mainly based on plasma from vaccinated donors.
Therefore, the dosage is currently being debated; but until further notice, the recommended dosage of Beriglobin is 0.25 ml/kg, max 15 ml as in practice this dose has proven capable of preventing measles in most cases.
(P.H. Andersen, L.K. Knudsen, Department of Infectious Disease Epidemiology, L.D. Rasmussen, C.S. Jensen, T.K. Fischer, Virology Surveillance and Research).
Link to previous issues of EPI-NEWS
20 May 2015