No 23 - 2023
Annual report on TBE (Central European encephalitis) in Denmark, 2020-2022
Mumps outbreak in Denmark
Annual report on TBE (Central European encephalitis) in Denmark, 2020-2022
TBE (tick-borne encephalitis, Central European encephalitis) is a virus disease transmitted to humans by ticks. TBE is a very rare disease in Denmark, typically causing 2-4 annual cases. Most of the people infected are symptom free or present with influenza-like disease. Only in a limited number of cases will the condition progress into encephalitis. Until 2019, TBE in Denmark was mainly limited to Bornholm, but an infection area was detected in Tisvilde Hegn and surrounding areas in 2019. The condition occurs far more frequently in limited areas in Sweden, including in Southern Sweden.
Since 2017, an increasing number of TBE cases has been diagnosed in Denmark, Figure 1.
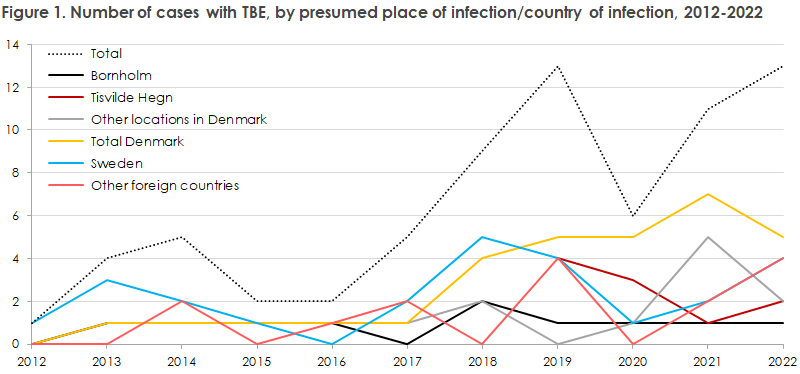
The increase is primarily caused by an increasing number of cases presumably infected in Denmark (the yellow line); partly sporadic cases from areas in Denmark where infection has not previously been acknowledged (the grey line), partly clusters with presumed infection in a new risk area in and around Tisvilde Hegn (the dark red line), EPI-NEWS 1-2/2020. Since 2020, an increase has also been observed in the number of cases with other presumed countries of infection than Denmark and Sweden (the green line).
Sweden has also witnessed a doubling of TBE cases in the past ten years despite intensification of TBEV vaccination; from 209 cases in 2013 to 465 cases in 2022. The cases were spread geographically, among others to the area of Scania (South Sweden).
In 2019, the SSI/DTU detected a new TBEV micro focus in ticks in an area close to a nature playground in Tisvilde Hegn after four persons had become infected with TBE in Tisvilde Hegn and Vinderød Woods, including two at the nature playground. TBEV infection was also detected in Tisvilde Hegn in 2020, 2021 and 2022, even after the nature playground was closed. Thus, other TBEV micro foci presumably exist in Tisvilde Hegn that have yet to be detected. The new TBEV micro focus around the nature playground has survived since 2019. Whole-genome sequencing of the virus shows relation with TBEV from Norway. It is believed that the virus was introduced at Tisvilde Hegn by migratory birds, after which TBEV may have spread further via, e.g., deer.
In 2020, a total of five TBE cases were detected with presumed infection in Denmark: three in Tisvilde Hegn, one on Lolland-Falster and one on the island of Bornholm, see EPI-NEWS no. 34-35/2020, where three of the cases are described in detail.
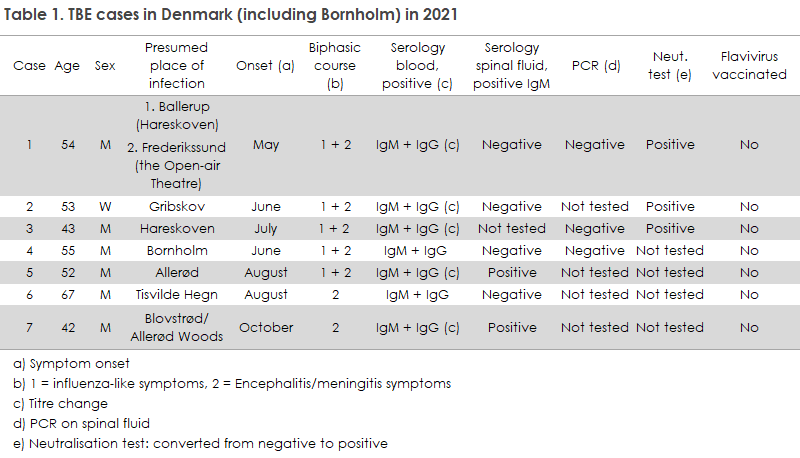
In 2021, all seven detected TBE cases had become infected in Denmark, and all except for one were presumably infected in one of various possible locations in North Zealand, Table 1. A new TBEV micro focus has possibly gained foothold in Hareskoven, where two of the seven patients reported having spent time. However, one of the two patients also pointed to the area in the vicinity of the Open-air Theatre in Frederikssund as a possible place of infection. However, by dragging a 1x1 m white flag across the forest floor (flagging) in the area surrounding the Open-air Theatre, researchers attempted to collect ticks, but none could be collected in the area flagged. So far, an infectious area has not been identified in Hareskoven from where it would be possible to collect ticks for TBEV testing at the SSI. Generally, it is very difficult to identify TBEV micro foci that carry a risk of infection as these foci are typically the size of a handball court or smaller.
Two patients had presumably become infected around Allerød, and the partially connected wooded areas of North Zealand now seem to form a hotspot for TBE cases in the area of Tisvilde Hegn/Vinderød Woods, Gribskov, Hareskoven and Allerød, whereas only sporadic cases were reported from Lolland-Falster, Southern Funen and Jutland, which therefore cannot with any certainty be considered to contain new TBEV micro foci. Even though TBE virus has only been detected in a single micro focus around Tisvilde nature playground, EPI-NEWS 25/2020 and Annual-Report-on-Zoonoses-in-Denmark-2021.pdf, the recently reported TBE cases indicate that the virus may have spread to several different locations in North Zealand in the period from 2020 to 2022. The reason why TBE virus is spreading in Denmark is somewhat elusive, but rising temperatures in May and widespread presence of deer are believed to play a role. An increase was also recorded in nearby Scania with more than 20 cases being recorded in 2021 (which then declined subsequently to 12 cases in 2022). In Sweden, where the condition is more widespread and has been present for a longer period time, some of the causes discussed are climate change and altered social behaviour in humans, including spending more time in woods and shrubbery, and an increase in the number of rodents and deer.
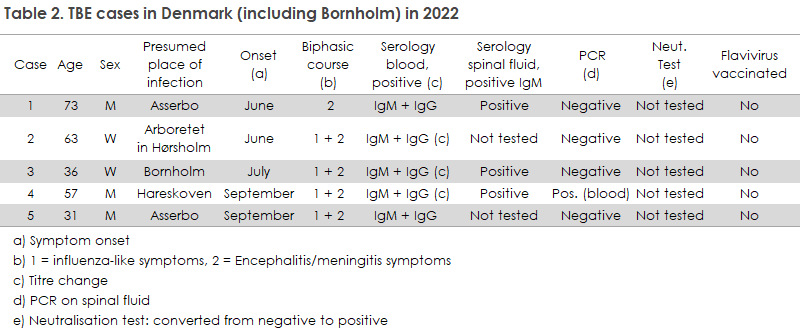
In 2022, a total of 14 TBE cases were diagnosed, among whom five had become infected in Denmark, Table 2. All were tested by serology and/or PCR. In one case, TBE virus was detected using PCR testing of blood. This is a rare finding as virus is present in the blood for only 2-10 days, typically in the phase characterised by fever and influenza-like symptoms, before the affected person develops symptoms from the central nervous system.
Infection abroad mainly occurred in Sweden, but also in Latvia, Germany and Norway. These cases were hospitalised in Denmark but were not included in the present description.
The cases recorded in 2022, which were presumably infected in Denmark, were all likely infected in North Zealand, except for the case recorded on the island of Bornholm: Two cases around Asserbo Plantation, one in Hareskoven and one case who resides in and visits woods in South Jutland but who also spent a day in Arboretet in Hørsholm and presumably became infected there.
The majority report various tick bites, but not all occurred in timely association with the condition. The areas where the infection was transmitted are located close to areas where infection was previously observed (Tisvilde Hegn and Allerød). Hareskoven was stated as the place of infection for one case in 2022, and, in conjunction with the one or two cases recorded in that area last year, it seems that one or more new micro foci may exist. However, it has not yet been possible to identify a specific area from where ticks may be collected.
In 2022, four of the five Danish cases experienced a typical two-phased disease course, starting with fever and an influenza-like feeling. Subsequently, all cases have been hospitalised for shorter or longer periods of time with symptoms of encephalitis, including, among others, headache, altered state of consciousness and confusion.
TBE virus infection and symptoms
TBE virus is mainly transmitted to humans via tick bites. In contrast to ticks carrying the very common Borrelia bacterium, ticks with TBE virus are recorded in multi-year micro foci (small areas the size of a bush or a handball court). The cause of the very varying and unequally distributed occurrence limited to micro foci remains unknown. Therefore, the risk associated with different areas within a single country may vary considerably. In Denmark, the tick season usually starts in April-May, when humans start to spend time in woods, and extends until October-November. Ticks may also be active in winter months, but the risk of infection in these months is limited.
TBE virus transmission by tick bites is initiated from the saliva glands of the tick within few minutes and continues for some hours. Therefore, the tick should be removed as soon as possible after being detected.
The infection is asymptomatic for approx. 75% of those affected. In the remaining 25% who develop symptoms, the condition is usually two-phased. Following a 7-14-day incubation period after the tick bite, phase one starts with 2-7 days of fever and uncharacteristic influenza-like symptoms, including fever, myalgia, fatigue and headache. After a symptom-free period lasting from few days to three weeks, between one and two thirds of the patients with symptoms will develop an infection in the central nervous system (encephalitis) with symptoms like fever, headache, unilateral paralysis, affection of consciousness and personality changes.
No treatment is available for TBE virus infection. Around one third of the patients with CNS symptoms may develop year-long or persisting neurological sequelae in the form of paralyses, tremor and/or cognitive dysfunction like learning disabilities and paranoid delusions.
Prevention and vaccination
Given the signs of increased spreading of TBE virus in Denmark, particularly in some areas of North Zealand, it is important to inform of preventive measures and, where relevant, to vaccinate risk groups.
You can protect yourself against tick bites either by attempting to avoid tick bites, by quickly removing ticks and/or by being vaccinated if you frequently spend time in woods and shrubbery beyond established paths in areas where TBE occurs. However, it is important to remain aware that vaccination will not provide 100% protection against infection.
The risk of becoming infected with TBE virus may be reduced by avoiding contact to vegetation and by wearing smooth-surface rubber boots and long-sleeved clothes, which may be impregnated with permethrin. Trouser sleeves should be tucked into your socks. Dogs may also be given permethrin preventively to keep them from bringing ticks indoors. Dogs can also develop TBE themselves.
Some mosquito balms (with DEET) also repel ticks. If you use mosquito balm to prevent tick bites, be sure to apply the balm every few hours.
Also be sure to check for tick bites, including in children. If you shower after staying outdoors, be sure to rinse off any ticks that have not yet bitten. Otherwise ticks may be removed using tick pliers/forceps, which may be acquired at pharmacies, or simply using your nails or by rubbing them until they fall off. Whether the head of the tick remains lodged in the skin will not affect the infection, but you should remain aware of any secondary infection that may occur in the wound.
The risk of developing a symptomatic CNS infection increases with age. This applies, in particular, to men aged more than 50 years. You may consider being vaccinated if you regularly spend time in a known risk area beyond established paths in the vegetation where deer pass and the concentration of ticks potentially carrying TBE infection is therefore high. Risk groups may, e.g., include hunters, campers, mushroom pickers, orienteers, wood workers and cottage owners. The SSI still assesses that the primary risk areas in Denmark are located on the island of Bornholm and in Tisvilde Hegn and surroundings. The SSI monitors the development of any new micro foci in other parts of North Zealand closely, and will regularly report any extended vaccination recommendations in collaboration with the Danish Health Authority. Beyond Denmark, the typical TBE risk areas are Scandinavia, the Baltics and, in particular, parts of Central Europe, including Poland, Germany and Austria.
Two inactivated TBE vaccines are currently registered in Denmark (Ticovac and Encepur), both are available in both paediatric and adult formulations. The SSI currently stocks the following inactivated TBE vaccines: TicoVac® 0.5 ml for persons above 16 years of age and TicoVac® Junior 0.25 ml for children from 1 to 16 years of age. If adults need vaccination, it may also - following individual assessment - be considered to vaccinate the family’s children. TBE protection is achieved after receiving two initial doses given at a 1-3-month interval. However, the interval separating the first and second dose may be reduced to 14 days. A third dose is given 5-12 months after the second vaccination, preferably shortly before the tick season starts in May. The vaccination course provides protection for three years. Thus, in case of continued exposure, a booster vaccine is warranted every 3-5 years:
- In persons who are less than 60 years of age at the time of vaccination, the second booster vaccination is given after three years and then every fifth year.
- In persons aged 60 years or above at the time of vaccination, the second booster vaccination is also given after three years, but then every third year.
Patients who are immunocompromised due to treatment or disease may need an extra vaccine dose. In these cases, antibody levels should be tested four weeks after the second dose was given to determine if an additional dose is needed.
In relation to minimising the risk of vaccine failure, Swedish data, as mentioned above, support giving an extra vaccine dose to persons aged 50 years or more in the basic vaccination programme (at 0, 1 and 6-12 months). This is not described in the approved TicoVac® summary of product characteristics and will therefore constitute off-label use of the vaccine, which must rely on a shared decision made together by the doctor and the patient.
(H. Aftab, R. Dessau, A.B. Hesselvig, DCM Slagelse, Region Zealand, A. Fomsgaard, Virology Surveillance and Research, T. Dalby, P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention)
Mumps outbreak in Denmark
The mumps is caused by parotitis virus infection. The disease causes swelling of the salivary glands and a slight fever. Not rarely, in 1-10% of cases, the condition causes a mild inflammation of the tissue that lines the brain and spinal cord (meningitis). Before the introduction of the MMR vaccine (measles, mumps and rubella) in 1987, parotitis virus was the most frequently observed cause of viral meningitis. Lasting sequelae following mumps are rare, but unilateral deafness may occur. Orchitis is observed in approx. a third of larger boys or men with mumps. This complication is more frequent in the 15-29-year age group. However, male sterility due to mumps is rare. Since the introduction of the MMR vaccine in 1987, the number of cases with mumps (parotitis) in Denmark has declined drastically, also see Mumps, Individually notifiable diseases - Monitoring in numbers, figures and maps (in Danish).
The age of those who fall ill with mumps has generally increased since the introduction of the MMR vaccine, and the mumps can no longer exclusively be considered a "childhood disease". This also applies to the current cases as the condition was detected in children and adults, alike. The risk of complications increases with increasing age.
To date, Statens Serum Institut (SSI) has recorded four laboratory-confirmed mumps cases in Denmark in 2023. All four cases had received at least one vaccination, most had received two vaccinations. The first three cases were diagnosed in mid-May, and the fourth in late May. All four cases occurred among persons from North Zealand. How the first three persons became infected has not been established as none of the cases had any travel activity or known contact to infectious persons. We do, however, see disease cases in Denmark every year in persons with no travel activity and no known contact with other disease cases. It therefore seems likely that mumps is lowly endemic in Denmark and that some cases go undetected.
The Danish Patient Safety Authority, Supervision and Guidance East, has been notified and has initiated information activities in the local area of this outbreak and established contact with other relevant healthcare stakeholders. Children with mumps may not return to their day-care service, school or kindergarten, etc. until a minimum of six days after symptom onset. No preventive treatment exists for persons who have been exposed to infection, and no specific treatment exists for the disease either.
Mumps can be prevented through vaccination with the MMR vaccine which forms part of the Childhood Vaccination Programme. The mumps component of the vaccine is not quite as effective as the measles and the rubella component, but a high vaccination coverage will yield a good general population immunity. Internationally, outbreaks have been described even among well-vaccinated population groups, and it should be expected that the share of vaccinated people may be relatively high during an outbreak in an area in which the majority of the population have been vaccinated. A good description of this paradox, taking measles vaccination as an example, is available at the ECDC’s website (page 7-8).
Physicians are currently encouraged to pay particular attention to the diagnosis in children and younger adults who present with symptoms compatible with mumps. Suspicion may be confirmed by blood sample testing for IgG and IgM antibodies, but the diagnosis is firmly established though PCR detection of parotitis virus in a throat swab, nasopharyngeal secretion and/or urine (or blood). Virology Surveillance and Research at the SSI performs typing and sequencing of parotitis virus.
The mumps is individually notifiable. The condition is notifiable in cases with clinical diagnosis and concurrent detection of virus and/or specific antibodies or contact to a known, laboratory-confirmed case in the community. With the new executive order on notification, with comes into force as per 1 July 2023, mumps will no longer be individually notifiable, but will instead be monitored through laboratory surveillance.
(L.K. Knudsen, P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention, K.T. Franck, Virology surveillance and Research, DPSA, East)