No 49/50 - 2021
Extension of the invasive pneumococcal disease vaccination programme
Tuberculosis in 2019-20
Extension of the invasive pneumococcal disease vaccination programme
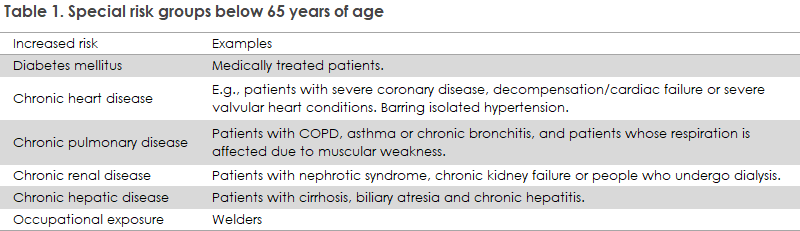
Since 22 April 2020, an offer of free pneumococcal vaccination has been in place for residents of nursing homes and residencies, persons with a particularly high risk of invasive pneumococcal disease (IPD) and, as from June 2020, elderly people who have turned 65 years old. On 15 December 2021, a new executive order came into force, including welders with a continuous occupational risk and persons below 65 years of age with some chronic diseases: diabetes mellitus and renal, hepatic, pulmonary and cardiac conditions, see Table 1. See the full overview of included target group patients in this infographic. Read more about target groups at the SSI website under “people at special risk of invasive pneumococcal disease”. The executive order covers vaccinations given no later than 28 February 2022.
Pneumococcal disease
Pneumococci are a type of bacteria that frequently cause infections in elderly people. They can cause meningitis and blood poisoning if they spread to the blood stream, see the SSI disease encyclopaedia.
Welders’ continuous exposure to certain metal-containing vapours, e.g., iron, chrome and nickel, increase the risk of pneumococcal infection.
The vaccination programme
Cf. the executive order, persons who have not received PPV23 vaccination in the past six years may be offered PPV23 vaccination. Vaccination may be offered earlier to persons who have had their antibody levels measured for medical reasons, indicating that the person is unprotected. For more details, please see EPI-NEWS 14-16/20 and 23/20.
Vaccination against pneumococcal disease, influenza and COVID-19 may be given concurrently (at different injection sites) or with any interval.
Concurrent administration of Pneumovax and Zostavax (against herpes zoster) may reduce the immunogenicity of Zostavax. However, data indicate that this has no clinical importance.
Pneumococcal vaccines are ordered and the cost of vaccination is settled following the provisions in place for seasonal influenza vaccination.
Pneumovax is supplied in Danish packaging with prefilled syringes, including needles: SSI item number 101939 Pneumovax 10x1 dose, at DKK 1,650.00 excluding VAT and are ordered using Form 6.
Vaccination must be performed by a doctor authorised to practice medicine in Denmark or it may be delegated by such doctor. For further information, please see the website of the Danish Medical Association.
Currently, two pneumococcal vaccines have been authorised; a 23-valent polysaccharide vaccine (PPV23, Pneumovax), which is used in special risk groups (as described above) and a 13-valent conjugate vaccine (PCV13, Prevenar13), which forms part of the Danish childhood vaccination programme. For further information about the vaccines, please see SSI’s vaccine encyclopeadia.
Vaccination coverage 2020/2021
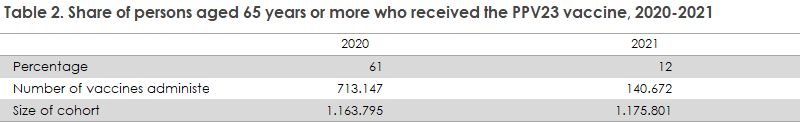
The vaccination coverage of the PPV23 vaccination is presented below. Table 2 presents the coverage in the group of patients aged 65 years or more. The table shows the coverage in 2020 and 2021. The total vaccination coverage recorded for the two-year period is 73%. The lower 12% coverage seen for 2021 should take into account the high 61% coverage recorded in 2020, since vaccination is recommended every sixth year. Persons who received vaccination in 2020 are therefore comprised by the 2021 cohort but will not be offered vaccination.
Enhanced duty of notification
As PPV23 forms part of a national vaccination programme targeting pneumococcal disease risk groups, the Pneumovax vaccine is on the list of medical products with an enhanced duty of notification. Therefore, physicians have an obligation to report all presumed adverse effects to the Danish Medicines Agency. Other healthcare workers as well as vaccinees and their relatives may also report any presumed adverse effects to the Danish Medicines Agency. When notifying, it is important to specify the vaccine’s batch number, if possible. Adverse effects may be notified at www.meldenbivirkning.dk
(S.B. Asmussen, K. Finderup Nielsen, P. Valentiner-Branth, Department of Infectious Disease Epidemiology and Prevention)
Tuberculosis in 2019-20
The 2019 annual report on tuberculosis was delayed one year due to the COVID-19 pandemic. Thus, the present report covers 2019 and 2020.
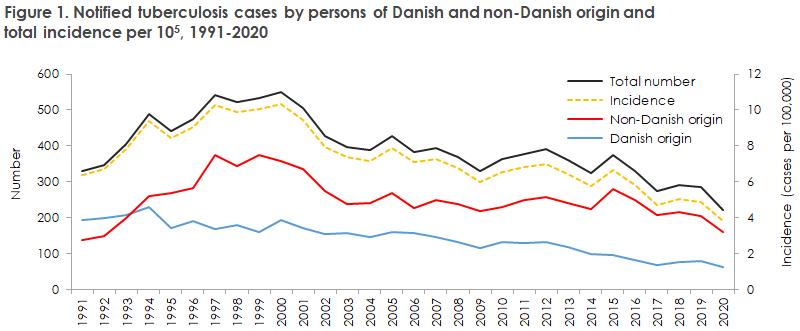
2019 saw a total of 284 notified cases of tuberculosis (TB), and in 2020 a total of 221 TB cases were notified. The occurrence of TB in 2019 was roughly on a par with that of 2018, whereas TB occurrence declined by 22% from 2019 to 2020, see Figure 1.
In 2021, the decline is expected to continue. At present, a total of 173 cases have been notified.
For a detailed epidemiological description of the 2019 and 2020 incidence, please see the joint 2019-20 annual TB report.
The total TB incidence in Denmark was 4.9 cases per 100,000 in 2019 and 3.8 cases per 100,000 in 2020.
As in previous years, the highest incidence in 2019 was recorded in the Capital Region of Denmark (6.4 per 100,000), where the incidence was higher for persons residing in Copenhagen than in the remaining parts of the region. In 2020, the highest incidence was recorded in the North Denmark Region (4.6 cases per 100,000), followed by the Capital Region of Denmark (4.1 cases per 100,000).
The region recording the lowest incidence in 2019 was the Central Denmark Region (4.1 cases per 100,000), and in 2020 the lowest incidence was seen in Region Zeeland (1.3 cases per 100,000).
Based on the total number of notifications for 2019 and 2020, 42% of the patients had become infected in Denmark, and 55% hereof were of Danish origin and 45% were of non-Danish origin.
Among children aged 0-14 years, a total of 65% had presumably become infected in Denmark. Among nine notified children aged < 5 years, eight had presumably become infected in Denmark. TB was therefore not only due to reactivation of latent TB the patients had acquired before their arrival to Denmark, but was to a considerable extent due to continued infection in Denmark, which is also documented by the large infection chain (”Cluster 2/1112-15”) that accounted for 24% of all typed cases in 2020 (corresponding to an increase from 2017 and 2018, respectively, when the infection chain comprised 18% of all typed cases). This chain of infection therefore still demands considerable attention as it is the largest recorded in Scandinavia to date. The observed increase underlines the importance of screening of exposed groups, not only in the Copenhagen area.
Greenlanders living in Denmark still have a high TB incidence, whereas the incidence among immigrants from Eritrea has been decreasing.
Impact of the COVID-19 pandemic on the number of notified TB cases in 2020
Globally, a considerable decline has been observed in the number of persons diagnosed with TB and notified in 2020 compared with 2019. Following considerable increases in the 2017-2019 period, an 18% decline was observed between 2019 and 2020, from 7.1 mio. to 5.8 mio. In contrast, the global number of deaths caused by TB increased from 1.2 mio. in 2019 to 1.3 mio. in 2020 due to reduced access to diagnostics and treatment. The global effects of the COVID-19 pandemic on the TB situation are described in the WHO’s annual tuberculosis report, Global Tuberculosis Report 2021.
The marked decline in TB cases globally was reflected in Denmark from 2019 to 2020. In the past ten years, the number of notified TB cases has followed a declining trend, even though minor fluctuations between years have been observed. Whereas the incidence remained at roughly the same level from 2017 to 2019, a more pronounced and marked decline was recorded from 2019 to 2020. The total reduction in the number of cases was 22% (284 in 2019 and 221 in 2020), with no difference between persons of Danish and non-Danish origin. The reduction covered most age groups but was greater for persons of Danish origin aged 35-44 years (54%) and among men. For persons of non-Danish origin, the largest reduction was observed in the age group 45-54 years (38%).
As was the case globally, it is assessed that the decline in the number of TB cases from 2019 to 2020 was likely due to COVID-19 lock-downs and/or poorer access to healthcare. A need exists to resume tuberculosis screening among socially exposed individuals across Denmark to avoid a subsequent increase in tuberculosis incidence in coming years in a group of patients that is already heavily affected by this condition.
Continued need to remain attentive to TB in Denmark
In Denmark, TB occurrence has followed a declining trend since 2000 when the incidence was 10.3 cases per 100,000. Internationally, the 2035 objective is to reduce TB incidence by 90% compared with 2015, when the incidence was 6.6 cases per 100,000. Even though the incidence has declined since 2000 to 3.8 cases per 100,000 in 2020, the decline is not sufficiently large to meet the objective of a 90% reduction in 2035 relative to 2015. Therefore, a need exists to further intensify the fight against TB in Denmark.
Microbiological trends
Compared with 2018, 2019 saw a decline in the number of microscopy-positive pulmonary TB among Danes, from 48% in 2018 to 42% in 2019. In contrast, the share of microscopy-positive pulmonary TB cases increased among immigrants, from 48 (in line with the previous year) to 53%. For 2020, a total of 62% of Danish pulmonary TB cases were positive by microscopy, whereas 54% of immigrants with pulmonary TB were positive by microscopy. The 2020 increase in the share of microscopy-positive Danish pulmonary TB cases likely reflects poorer control with the TB epidemic in 2020 as a higher share of microscopy-positive cases suggests a later diagnosis of TB cases.
In contrast, no more cases of multiple resistance (MDR) were recorded in 2019 (four cases, 2% of the culture-verified cases) or 2020 (two cases, 1% of the culture-verified cases) than in previous years. No cases of extreme drug resistance (XDR) were observed in either 2019 or 2020.
(L.H. Holm, A. Koch, L.K. Knudsen, P. H. Andersen, S. Cowan, Department of Infectious Disease Epidemiology and Prevention, D. B. Folkvardsen, T. Lillebæk, Department of Tuberculosis and Mycobacteria)
15 December 2021