No 38 - 2016
Gonorrhoea 2015
Gonorrhoea 2015
National monitoring of gonorrhoea at Statens Serum Institut (SSI) is effected by reporting (submission of isolates) to the Laboratory Notification System (LNS), the Department of Microbiology and Infection Control, and by clinical notification to the Notification System for Infectious Diseases (NSID), the Department of Infectious Disease Epidemiology. Furthermore, as in 2014, EPI-NEWS 40/15, data were extracted from the Danish Microbiology Database (MiBa); a nationwide auto-updated database of all test results from the departments of clinical microbiology (DCMs), EPI-NEWS 45/13.
For gonorrhoea, this includes results from culture and PCR or other nucleic acid amplification technique (NAT), as most DCMs perform combined NAT for gonococci and Chlamydia trachomatis. In case of repeated episodes in a person, a new gonorrhoea case is defined as the passing of more than 21 days since the latest positive finding.
2015 saw the detection of 2,735 cases in the MiBa. To this another 53 cases should be added that were notified to the NSID, but not found in the MiBa. Thus, a total of 2,788 cases were detected. The cases affected a total of 2,682 persons, as 2,580 had a single case detected, 99 persons had two cases detected, two persons had three cases and one person had four cases detected. A total of 1,655 (59%) were men and 1,133 (41%) were women.
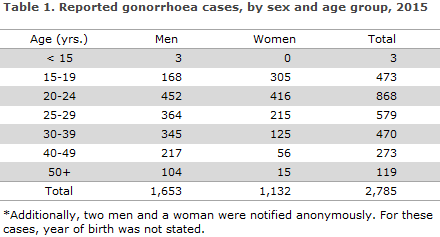
The median age was 27 years for men (range 0-70 years) and 22 years for women (range 6-63 years). The age distribution is shown in Table 1.
A total of 913 (33%) cases were reported to the LNS and also notified with the NSID. A total of 215 cases (8%) were reported only to the LNS and 709 (25%) only to the NSID. A total of 951 cases (34%) were registered only in the MiBa, but had neither been registered in the LNS nor notified with the NSID, including 562 men (59%) and 389 women (41%). The same gender distribution was also found in the other data sources.
Among the 951 cases that were recorded only in the MiBa, 464 (49%) had been tested only using NAT, 452 (47%) had a positive NAT, but a negative culture, and 34 (4%) had both a positive NAT and a positive culture. One case had been tested only by culture.
A total of 53 cases could not be retrieved from the MiBa, either because no civil registration number had been provided on the notification form (39 cases), or because the diagnosis had been made on the basis of clinical tests, epidemiology or microscopy the results of which are not added to the MiBa (14 cases). The distribution was different among the remaining 1,784 cases who were recorded both in the MiBa and had been notified with the NSID and/or reported to the LNS. In this group, a total of 1,025 (57%) had both a positive NAT and a positive culture, 460 (26%) had a positive NAT, but a negative culture, 157 (9%) had been tested only using NAT, and 142 (8%) had been tested only by culture.
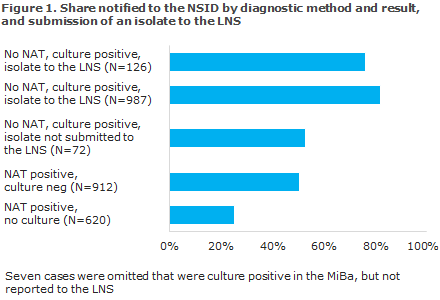
Figure 1 shows that the share of the cases that were notified with the NSID depended on the primary diagnostic method used (culture or NAT), on the result of the test and on whether an isolate had been submitted to the LNS or not. The share of cases notified to the NSID was greater for cases in which an isolate had been submitted to the LNS than for cases in which no isolate had been submitted, Figure 1. The notification share was more or less equally low in the following two situations: when only a positive NAT and a negative culture were available (50%), and when a positive NAT and a positive culture were available, but no isolate had been submitted (52%) The lowest notification share (25%) was seen in cases with a positive NAT, but no culture.
Three children were notified with gonorrhoea in 2015. One of these was a neonate who had been reported either to the LNS or the NSID, but for whom the MiBa made it clear that it was a case of gonococcal conjunctivitis transmitted at birth. The two other children had been notified to the NSID as sexually transmitted cases, and it was clear from the notifications that the cases would undergo further follow-up at a clinic of infectious disease medicine and at the Centre for Sexual Assaults (Center for Seksuelle Overgreb).
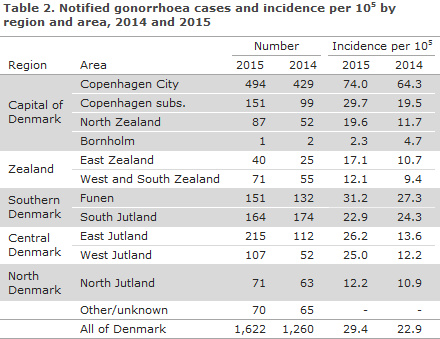
Geographical distribution
A considerable increase was seen in all areas except for South Jutland, Table 2. In 2014, South Jutland recorded the country’s highest increase in incidence (149%), EPI-NEWS 40/15, but the incidence decreased slightly in 2015.
Transmission
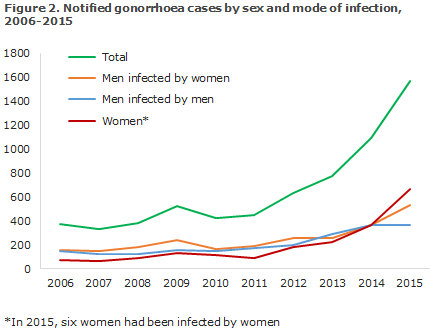
Among the 1,622 cases notified to the NSID, 957 were in men and 665 in women, Figure 2. Among 957 cases reported in men, 533 (56%) were acquired by heterosexual transmission, 368 (38%) by homosexual transmission, and in 56 (6%) cases the mode of transmission remained unknown.
Among the 665 cases in women, six had become infected by women.
Furthermore, eight of the female cases were notified as having been established owing to examinations made in connection with pregnancies.
Information on origin was available for 1,486 of the notified cases, of which 1,361 (91%) occurred in Danes, 83 (6%) in immigrants, 31 (2%) in second-generation immigrants and 10 (1%) in tourists.
Among a total of 344 cases in men who have sex with men (MSM) and for which the country of infection was stated, 318 (92%) were infected in Denmark, whereas the corresponding share was 469 (91%) among the 513 cases observed in heterosexually infected men (HIM). Among the 639 female cases for which the country of infection was known, 615 (96%) were infected in Denmark.
Of the 82 cases (62 in men and 20 in women) which were notified as having been acquired abroad, 14 were acquired in Thailand: 12 in HIM and two in men for whom the mode of infection was not stated.
Gonorrhoea and HIV
Information about HIV status was available for 346 (95%) of the 364 men who were notified as MSM. Among these, 77 (22%) were HIV positives; 67 of whom were already known to have HIV. Among the 533 men who stated that they had been infected through heterosexual contact, 367 (69%) had been tested for HIV. Including two known HIV positives. Among 665 women, a total of 446 (67%) had been tested for HIV. Including one woman who had emigrated from Sub-Saharan Africa and who had previously been registered as a HIV positive.
Specific anatomical localisations
In five cases, gonococci were established in culture from the eye: a 20-year-old and a 28-year-old woman, a 7-year-old boy and a 23- and a 54-year-old man. Additionally, a neonate was registered in the MiBa with a NAT-positive eye test.
Antimicrobial resistance
In 2014, the Reference Laboratory received gonococcus isolates relating to a total of 1,127 cases of gonorrhoea from the Danish departments of clinical microbiology (DCMs). The isolates were tested for ciprofloxacine, azithromycin and ceftriaxone sensitivity by determination of MIC (minimum inhibitory concentration, mg/l) and for formation of penicillinase, which indicates high resistance to penicillin.
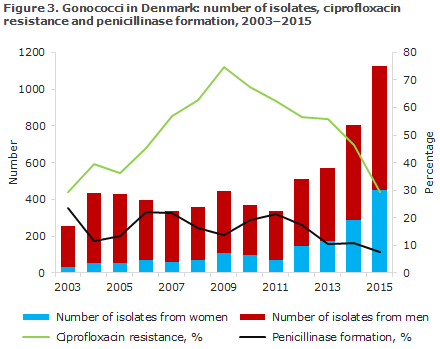
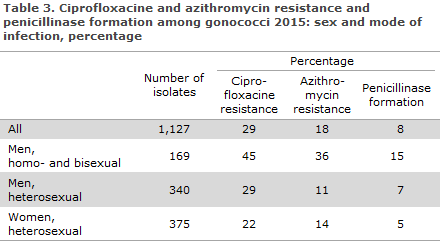
Ciprofloxacin resistance (including reduced susceptibility) was detected in 29% (46% in 2014) of the isolates, Figure 3. Azithromycin resistance was found in 1% of the isolates, and reduced susceptibility was found in 16% (5% and 19%, in 2014). Penicillinase formation was detected in 8% (11% in 2014).
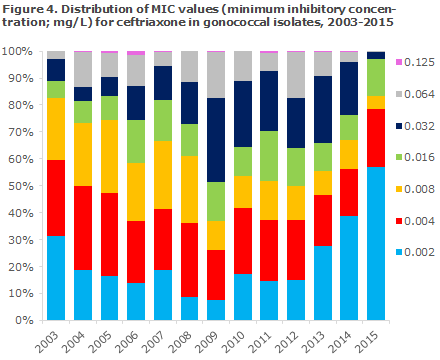
An isolate is considered susceptible to ceftriaxone at a MIC ≤ 0.125 mg/l, and resistant at a MIC > 0.125 mg/l. In 2015, one isolate was detected with a MIC = 0.125 mg/l, Figure 4 (four in 2014 and two in 2013). In 2004, 73% of the isolates had a MIC not exceeding 0.008 mg/l. In 2009 this share was only half as large (37%), but the worrying trend towards gradually increasing MIC values then reversed, and in 2015 the share had increased to 83% (67% in 2014).
As part of a joint EU effort, the Reference Laboratory annually tests approx. 100 isolates against an expanded panel of antibiotics. In 2015 it was determined that among 110 isolates, 0% (6% in 2014) were resistant to cefixim (an oral cephalosporine) and 0% to spectinomycin (0% in 2014). None of the two latter drugs are marketed in Denmark.
Transmission and resistance
Ciprofloxacine resistance occurred more frequently among MSM than among men notified as HIM, Table 3. Among HIM, transmission abroad was associated with a higher occurrence of resistance than transmission in Denmark, Table 3.
Treatment
Several locations abroad, but not in Denmark, have reported ceftriaxone treatment failure and detection of ceftriaxone-resistant strains.
In late 2015, the Danish Health Authority published amended Danish guidelines on the diagnosis and treatment of sexually transmissible infections (in Danish). The standard treatment is 500 mg ceftriaxone intramuscularly and 2 g azithromycin orally, both as a single dose. The exception to this rule is uncomplicated urogenital gonorrhoea detected by culture. Here, the first-line treatment is ceftriaxone 500 mg intramuscularly alone, and - in case of documented susceptibility - ceftriaxone 500 mg orally as a single dose.
Gonorrhoea should not be treated with azithromycin alone. Doses of 1g carry a considerable risk of treatment failure and resistance development. It is important that all treated patients attend check-ups. Asymptomatic patients should have a NAT performed 2 weeks after treatment has been concluded, and any positives should be supplemented by culture and sensitivity testing - as is the case during primary diagnostics.
If gonococci were initially detected by culture or NAT, a control test should be performed 1-2 weeks after the treatment with swabs from relevant anatomical locations (culture and resistance testing). If the initial test results were a positive NAT, but negative culture for gonococci, a control test should be performed with NAT 2 weeks after the treatment with swabs from relevant anatomical locations.
Commentary
The number of gonorrhoea cases kept climbing in 2015. The increase was seen across Denmark, apart from in South Jutland, and among women and men alike. Nevertheless, among men the increase was seen only in HIM, whereas the number of cases among MSM is in line with the 2014 level, EPI-NEWS 40/15. The relative increase was greater among women (66%) than among men (34%).
As in 2014, inclusion of data from the MiBa yielded a total number of cases that was 51% higher than the sum total reported to the LNS and the NSID. We consider that MiBa is accurate as it is complete and covers all parts of Denmark, and because the methods used for detection of gonococci are considered to have a high sensitivity and specificity.
According to the notifications, the majority of the cases had become infected in Denmark, and the second most frequent country of infection was Thailand.
As opposed to syphilis, which is mainly seen in MSM, gonorrhoea is now increasingly reported among heterosexuals. It causes concern that more cases of gonorrhoea are also seen in pregnant women, and health workers are encouraged to be attentive to gonococci as the cause of conjunctivitis in neonates, particularly in the initial 14 days of life. Gonorrhoeal conjunctivitis, which is increasingly being diagnosed in non-neonates, is a potentially very serious condition that shall be referred acutely to a specialist department and treated rapidly to maintain vision in the eye/eyes.
As other sexually transmissible diseases, gonorrhoea is a so-called indicator condition for HIV, which means that more than 0.1% of patients with a sexually transmissible condition are co-infected with HIV. Physicians are therefore encouraged to test for HIV when diagnosing gonorrhoea, regardless of the mode of transmission. Furthermore, testing for other relevant sexually transmissible diseases, like syphilis, chlamydia and possibly LGV is recommended.
Thorough diagnostics remains an important measure to counter further spreading of gonorrhoea. Diagnostics should include sampling from all relevant anatomical locations (urethra, rectum, throat and in women also the cervix) along with barrier protection with by use of condom and partner tracking. Gonorrhoea can show few symptoms and be asymptomatic, and this is practically always the case for gonorrhoea of the throat and rectum. If the infection is located to these anatomical sites exclusively, and if it is not diagnosed, the patient constitutes an infection reservoir.
As for syphilis, EPI-NEWS 36/16, the notification frequency was affected if a notification form had been sent out in connection with the submission of an isolate to the LNS. It seems safe to assume that the notification form that the LNS sends to the person ordering the test after receiving the isolate from the diagnosing DCM constitutes an extra incentive for case notification.
Nearly half of the NAT positives who had a culture performed tested negative. This may be due to the fact that gonococci are very fragile and will not tolerate prolonged transport in the mail system. In other cases, the infection may be in the early stages, which are, indeed, detectable with the more sensitive NAT, but not yet by culture. Finally, it is possible that a limited number of the positive NAT results are false positives.
This latter possibility is probably rare and as NAT is considered to have a good specificity, a positive NAT test shall always trigger immediate treatment. In the Danish Health Authority’s recommendations on the prophylaxis, diagnosis and treatment of STI (in Danish) immediate initiation of treatment is recommended following a positive NAT test, but after taking specimens from all relevant localisations for culture and susceptibility testing.
The Department of Infectious Disease Epidemiology has contacted a number of those who had ordered a test, which according to the MiBa later came back positive, but for which a notification was missing. It turned out that several of those who ordered the tests had misunderstood the text sent out with the positive NAT test result.
These texts may vary from one DCM to the next. In some cases the text has a wording similar to: “The result needs confirmation by culture” or “should be followed-up by a culture”, and several physicians had interpreted this to mean that the NAT result alone was not indication for treatment, but that they should await the result of the culture. A subsequent negative culture result was interpreted as if the patient did not suffer from gonorrhoea, and therefore no treatment of the patient was initiated and no notification submitted. The SSI is currently scrutinising more closely the cause and effects related hereto.
(S. Cowan, L. Espenhain, Department of Infectious Disease Epidemiology, S. Hoffmann, Microbiology and Infection Control)
Link to previous issues of EPI-NEWS
21 September 2015