No 37 - 2016
Meningococcal disease 2015
Purulent meningitis 2015
Meningococcal disease 2015
In Denmark, invasive meningococcal disease (MD) is monitored via the clinical notification system (Form 1515) and by the Neisseria and Streptococcal Reference Laboratory, which receives meningococcal isolates from the departments of clinical microbiology. MD covers meningitis, sepsis, bacteraemia and culture or DNA detection of meningococci in material from normally sterile locations, e.g. joints.
In 2015, the Department of Infectious Disease Epidemiology received a total of 39 notifications concerning patients with MD. None had more than one case of MD in 2015. In six cases, a reminder had to be sent out for the notification (15%). Reminders were sent to two additional cases, but no response was received: One case with finding of group C in blood and one case diagnosed with MD by PCR in blood and synovial fluid, but without grouping.
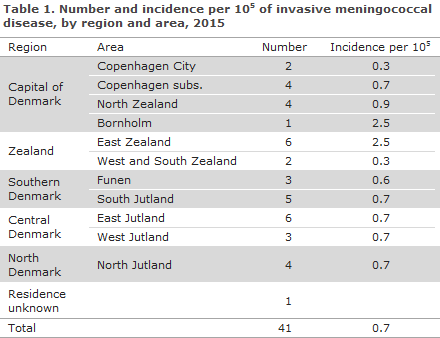
Table 1 shows the distribution by area.
Diagnosis
Of the 41 cases, 23 had meningitis, 10 sepsis, 6 both meningitis and sepsis; and in 2 patients meningococci were found in synovial fluid from the ankle and the knee, respectively.
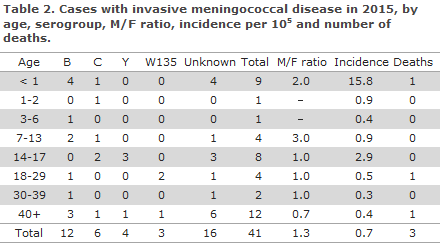
In all, 12 (29%) cases of MD of group B were observed, 6 (15%) group C, 4 (10%) group Y and 3 (7%) group W135. See Table 2, which also presents the age distribution. No cases of serogroups A, X, Z or 29E were notified. In 16 cases (39%), the group was unknown, including seven cases notified based on clinical suspicion alone.
The presumed country of infection was stated in 39 cases: 37 in Denmark, one in Germany (group C) and one in Turkey (group Y).
Diagnostics
In 22 (54%) of the cases, meningococci were detected by culture, including five which were also detected by PCR. An additional nine cases were diagnosed by PCR, three by meningococcal antibody test, whereas seven were notified based on clinical suspicion alone.
Underlying diseases
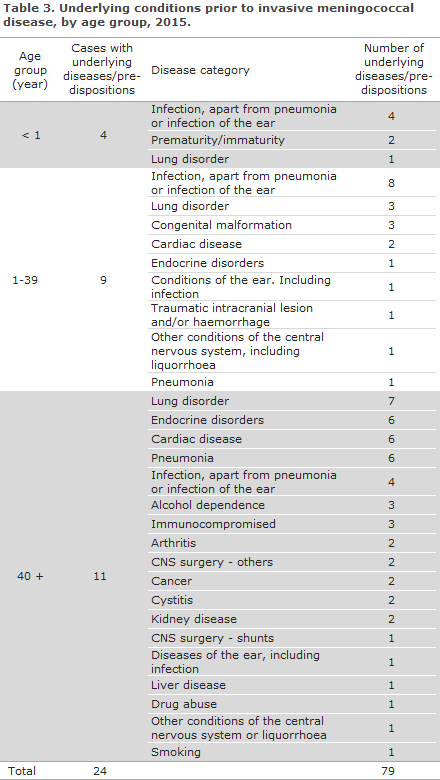
Underlying diseases were determined by linking data from the clinical notification system with the National Patient Register (NPR). From the NPR, underlying diseases and sequelae were categorised into groups based on diagnosis codes. Infections were included up to one month prior to the current MD case, but in general no time restrictions were applied for the remaining underlying diseases/predispositions.
In 24 of the 41 cases of MD, one or more underlying diseases and/or predispositions were recorded in the patients: In four of nine paediatric cases in children below one year of age, an infection was registered prior to MD. Half of the 18 cases aged from 1 to 39 years of age had underlying diseases. Among these, all had an infection, three pulmonary disease, three congenital malformations, one traumatic intracranial lesion and/or haemorrhage, and one had liquorrhoea. All cases above 40 years of age had underlying conditions of which pulmonary disease was the most frequently occurring. Furthermore, three had alcohol dependence and one had other abuse, three were immunocompromised, two had a previous CNS operation, including one with a shunt, two had cancer and one had liquorrhoea.
Eight of the 11 cases above 40 years of age had an infection, including six with pneumonia, one with previous CNS infection, and one with an infection of the ear.
Mortality and sequelae
Three patients died due to MD: a 72-year-old woman with chronic pulmonary disease and pneumonia who was notified on the basis of her clinical disease picture, an infant aged 2½ months who was notified based on the clinical disease picture, and a woman aged 20 years with group W135 meningococci. No underlying conditions were recorded for the two latter cases.
Only diagnosis codes given more than five days after disease onset and after the patient’s admission for MD were categorised as sequelae. Sequelae were recorded for five patients: Two with epilepsy, and hearing impairment and visual defect, respectively; one with cochlear dysfunction; and two with hearing impairment or hearing loss, one of whom also suffered from headaches.
Notification
Any physician receiving an MD patient for treatment shall immediately notify the case when clinical suspicion arises. Notification is by phone to the Danish Patient Safety Authority, Supervision and Guidance division North, South or East depending on where the patient was admitted, and in writing on Form 1515 to Statens Serum Institut, the Department of Infectious Disease Epidemiology.
Prophylaxis for contacts
Household-like contacts to patients with suspected or verified MD are offered antibiotics prophylactically, EPI-NEWS 17/10.
Vaccination is offered via the Danish Patient Safety Authority, Supervision and Guidance, following verified MD caused by group A, B, C, W135 or Y to the group of persons who have been offered antibiotic prophylaxis EPI-NEWS 33/14. Vaccination must be given no later than 4 weeks after exposure.
Two tetra-valent conjugate vaccines have been registered for protection against meningococcal disease caused by group A, C, Y or W135; Nimenrix® and Menveo®. In case of group C MD, the monovalent vaccine NeisVac-C® is used.
Nimenrix® can be used for children aged ≥ 1 year of age and for adults. The vaccine is administered as a single dose. It is assumed that the protection will last for five years.
Menveo® can be used for children aged ≥ 2 years of age and for adults. The vaccine is administered as a single dose. It is assumed that the protection will last for five years.
If indicated, children aged 2 months to 1 year may receive primary vaccination in the form of two Menveo® doses given at a minimum 1-month interval. The Danish Medicines Agency has previously assessed that the vaccine may be used off-label in this age group, EPI-NEWS 37/10. In case of continued risk of exposure, a booster dose is given 12 months after the primary vaccination programme. Vaccination of children aged from 2 months to 1 year should be limited to cases in which administration of the four-valent vaccine (Menveo®) is indicated, i.e. as prophylaxis against group A, Y or W135.
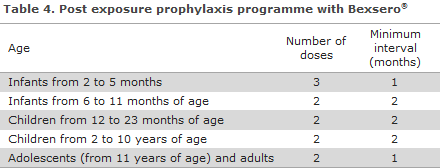
Bexsero® is approved for protection against MD of group B in persons above 2 months of age, Table 3. If children below 2 years of age continues to be at risk, a booster should be given during the child's second year of life at a minimum interval of 2 months after the latest dose, cf. EPI-NEWS 33/14. The need for a booster in children as from the age of 2 years and in adults has not been established. The vaccine requires an issue permit from the Danish Medicines Authority, which you can apply for electronically at The Danish Medicines Agency's website.
Commentary
The 41 cases of MD was the lowest number recorded since monitoring of the disease began in 1980. In the 10-year period from 2005 to 2014, the average number of MD cases has been decreasing for all age groups, except among children below 1 year of age and among 30-39-year-old persons. As in previous years, the MD incidence was highest in the younger-than-1-year age group.
Figure 1 presents MD by serogroups. Overall, the number of group B MD has followed a decreasing trend since the 1990s, and in the past 10-year-period it has decreased from approx. 40 annual cases in 2005-2009 to what is currently the lowest number recorded: 12 cases in 2015. Group B has largely been the most frequently occurring group, except in 2011 and 2012 when an increase was observed in group C MD; an increase which was also seen in several other European countries EPI-NEWS 37/11.
Following a considerable decrease since 2011 (46 cases), the number of cases caused by group C now remains at the same low level as was seen in 2014 when 6 cases were also seen.
Group A MD has not been notified since 2005, when two imported cases were observed.
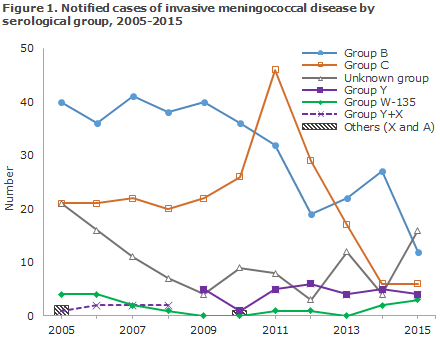
From 1999 to 2008, an average of two annual cases was recorded of group X and group Y in total. Since 2009, only a single case of group X has been recorded, in 2010, whereas the number of group Y cases has ranged from four to six annual cases, except for 2010 when only a single case was recorded.
W135 is a rarely occurring group, as only one or no annual cases have been observed since 2007. In 2014, two cases of W135 were recorded, in 2015 three cases, and in 2016 five (the latest case was recorded in the beginning of August). In other European countries such as the UK and most recently Holland, an increase has been recorded in the number of W135 cases. More group W135 cases have also been seen in Denmark in recent years, EPI-NEWS 38/15, and the development is monitored.
Even though joining of data from the Neisseria and Streptococcus Reference Laboratory and the MiBa has facilitated inclusion of MD cases that were not notified in the annual report for 2015, we take this opportunity to underline the importance of rapid notification in writing following notification by phone to the Danish Patient Safety Authority, Supervision and Guidance, with a view to achieving a complete and current national overview.
(L. Espenhain, C.H. Suppli, P. Valentiner-Branth, Department of Infectious Disease Epidemiology; S. Hoffmann, Department of Microbiology and Infection Control)
Purulent meningitis 2015
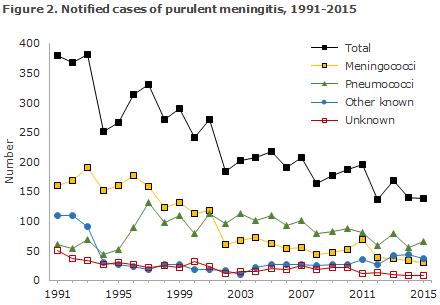
2015 saw a total of 138 notified cases of purulent meningitis. Figure 2 and Table 5 show the distribution by aetiology and age. Meningococcal meningitis (29 cases) in 2015 is described elsewhere in this issue of EPI-NEWS.
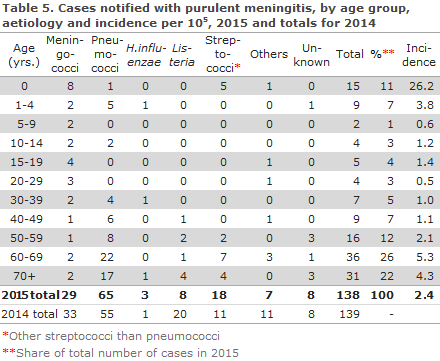
Pneumococci
2015 saw a total of 65 notified cases of meningitis with Streptococcus pneumoniae. A total of 45 cases were detected by culture of cerebrospinal fluid (CSF), six hereof were also verified by PCR on CSF. An additional 12 cases were detected only by PCR in CSF, eight cases were notified with a combination of clinical meningitis and finding of pneumococci by blood culture (4) and/or finding of pneumococcal antigens in the urine (3) or microscopy of the CSF (1).
Generally, across age-groups, infection prior to disease was the most frequently recorded predisposition. A total of 35 of the 65 notified cases (54%) had an infection prior to presenting with the condition. Ear infection (22) was the most frequently observed, whereas pneumonia was recorded in eight cases prior to presenting.
A total of 24 (37%) had endocrine conditions. Pulmonary conditions were recorded in a total of 16 (25%) cases. For six (9%) of the patients, diagnoses consistent with diseases of the central nervous system were stated, including hydrocephalus, liquorrhoea and traumatic intracranial lesion and/or haemorrhage. In twelve cases (19%), it was stated that the patient had undergone shunt surgery (9) and other CNS surgery (3). For 54 patients, information was available on underlying conditions and/or pre-dispositions: Typically, more than one diagnosis code was given for each patient and therefore the total number of diagnoses exceeds the total number of patients.
Eight patients died due to their condition, one woman aged 32 years and seven men aged 45-84 years. Four of these had alcohol dependence or other types of abuse and other underlying conditions. Additionally, one had lung cancer, one lung disease and one had both a cardiac condition and intracranial lesions. One had infection prior to disease and sepsis. For one patient, there was no record of underlying diseases.
Eighteen patients suffered sequelae: Seven suffered hearing impairment or hearing loss, six needed rehabilitation, two suffered visual defects, one acquired learning disabilities, one hydrocephalus and one epilepsy.
Other streptococci
Meningitis due to other streptococci than pneumococci was detected in 18 cases. Fifteen cases were caused by b-haemolytic streptococci: three with group A streptococci, nine with group B streptococci (GBS), one with group C and two with group G. In three cases, non-haemolytic streptococci were detected: S. mitis, S. salivarius and S. anginosus.
The three patients with group A streptococci were all 65 years old or more and all had an aural infection focus and underlying conditions. One died and one suffered hearing impairment or hearing loss.
The patient who had group C streptococci was a man aged 60 years who had a defect in the frontal sinus following a trauma suffered 40 years earlier; he had meningitis in 1991 and also had endocrine conditions, pulmonary disease, pneumonia, a shunt and intracranial lesions. He subsequently needed rehabilitation.
The two patients with group G streptococci were both more than 60 years old and one of them had a heart disease. None of these patients had sequelae.
Five of the nine cases with GBS occurred in infants. Among these, three were probably infected at birth. Three of the four persons above 50 years with GBS were immunocompromised, two had cancer and one had chronic diseases in nearly all organ systems. Two had late sequelae, including one who suffered hearing impairment.
The patient with S. mitis was a woman aged 76 years who had various underlying diseases and pneumonia. She suffered no sequelae.
A 68-year-old woman with various underlying conditions had S. salivarius meningitis. She recovered without sequelae.
The patient with S. anginosus was a 59-year-old man who had a periventricular abscess that drained to the ventricular system. He suffered no sequelae.
Haemophilus influenza
A total of three cases of H. influenzae were notified, one of serotype F in a 1-year-old child with congenital malformations, splenectomy, malformations and kidney disease and two non-capsular strains, biotype II and III, respectively, which could therefore not be grouped. In the two latter cases, one of whom also had endocrine diseases, a cardiac condition and cancer, pneumonia and pulmonary disease were recorded as the underlying predisposing conditions. No late sequelae were recorded for any of these patients.
Listeria monocytogenes
A total of eight cases caused by L. monocytogenes were notified. All cases had become infected in Denmark. Three cases occurred in patients aged 41, 57 and 58 years, respectively - the remaining five cases occurred in patients ≥ 65 years of age. Underlying disease and/or pre-dispositions were recorded for all patients. Five had cancer disease, and one also had lung disease, one arthritis and another had endocrine disease and a liver disorder. Three patients died due to the disease, all of whom had cancer disease. One patient developed encephalitis during the disease course and suffered from sequelae in the form of impaired eye-sight and hearing and cochlear dysfunction.
Other aetiology
Three patients had meningitis caused by Escherichia coli, including one neonate (premature). It is presumed that this patient had become infected through the birth canal. In one 69-year-old man, neuro-infection was probably due to a course of urosepsis. A 60-year-old man died in whom various underlying conditions were recorded. No late sequelae were recorded for the two survivors.
A 46-year-old man had meningitis, which secondarily developed into endocarditis, for which Staphylococcus aureus was detected. No sequelae were recorded.
Two patients aged 17 and 62 years, respectively, had meningitis with enterococci, one with Enterococcus faecalis and one with Enterococcus faecium; both had underlying conditions and/or risk factors. One had undergone scoliosis surgery 12 days previously and one was admitted with a subarachnoid haemorrhage with subsequent insertion of a drain and had a liver disorder, heart disease and alcohol dependence. None of these patients died. Rehabilitation was recorded for one of the patients.
One immunocompromised 27-year-old patient had meningitis with Pasteurella multocida. He had probably become infected in Denmark, but had entered Denmark from Romania 11 days prior to disease onset. No sequelae were recorded.
Unknown aetiology
In a total of 8 cases, patients were notified on the basis of clinical tests and/or cell counts and microscopy of cerebrospinal fluid consistent with purulent meningitis, but without detection of bacteria by culture or PCR.
Underlying disease and/or risk factors were recorded for six of these patients; four had infection prior to their disease episode, three of whom had a lung condition. One had a traumatic subdural haematoma evacuated prior to the disease episode and one had a heart disease. One patient with no underlying conditions died due to the disease. Sequelae were recorded in the form of visual defects or loss of vision in one already chronically ill person.
Commentary
The number of cases of purulent meningitis in 2015 was in line with that recorded in the three preceding years.
The 65 notified cases of pneumococcal meningitis remains lower than the approx. 100 annual cases observed in the 2000-2007 period before the introduction of the conjugate pneumococcal vaccine into the childhood vaccination programme, EPI-NEWS 37a+b/07. Nevertheless, it constitutes a small increase compared with the levels observed in 2012 and 2014.
All five cases of pneumococcal meningitis in children aged 0-4 years of age who were serotyped were caused by serotypes that do not form part of the 13-valent conjugate pneumococcal vaccine, which has been included in the childhood vaccination programme since 2010. In one case the serotype could not be determined.
Meningitis caused by other streptococci than pneumococci increased from 11 cases in 2014 to 18 in 2015, which is the highest number recorded since registration was initiated in 1991.
The number of cases of purulent meningitis of unknown aetiology was in line with 2014 when 8 cases were also recorded, but has followed a slightly decreasing trend since 2007 when 24 cases of unknown aetiology were recorded.
The number of meningitis cases caused by the listeria bacterium in 2015 (8) was once again in line with the number observed in 2011 and 2012, when six and nine cases, respectively, were recorded. 2014 saw a total of 18 cases of listeria meningitis due to a major listeria outbreak EPI-NEWS 1-2/15.
(L. Espenhain, C.H. Suppli, P. Valentiner-Branth, Department of Infectious Disease Epidemiology; K. Fuursted, S. Hoffmann, Department of Microbiology and Infection Control)
Link to previous issues of EPI-NEWS
14 September 2016