No 11 - 2016
Bacterial intestinal infections 2014-15
Bacterial intestinal infections 2014-15
This issue of EPI-NEWS brings reports for a two-year period on three zoonotic bacterial intestinal infections: Campylobacter spp, zoonotic Salmonella enterica and Yersinia enterocolitica. The bacterial intestinal pathogens are surveyed through the laboratory notification system. First-time positive, diagnosed patients (within a 6-month period) are registered in the national surveillance database Register of Enteric infections (Tarmbakteriologisk Register). For Salmonella and Yersinia enterocolitica, the notifications are followed up through concurrent submission of isolates to the SSI reference laboratory. Campylobacter and Yersinia enterocolitica were most recently described in EPI-NEWS 12/14 and Salmonella in EPI-NEWS 11/14.
General development
In 2015, the monitoring of both Campylobacter and Yersinia enterocolitica underwent changes. For the first time ever, data were drawn directly from the Danish Microbiology Database (MiBa) and only supplementary data were entered from submissions from the departments of clinical microbiology. This presumably improved surveillance as data became available more rapidly and more patients were registered. A comparative analysis of the number of patients reported to the Enteropathogenic Register and patients available via MiBa in the 2011-14 period demonstrated that 10-25% (depending on the calendar year) of campylobacter patients were not reported. It was therefore to be expected that the transition to automatic data capture via MiBa would bring an increase in the number of registered patients in 2015. For salmonella, surveillance remained unchanged in 2014-15.
Figure 1 shows the number of notified cases of Campylobacter spp, Yersinia enterocolitica, and zoonotic serotypes of Salmonella enterica in the 1980-2015 period. The age-specific incidence for 2015 is presented in Table 1; the same pattern was observed for 2014 (not shown). For further information, please see the page Overvågning i Tal, Grafer og Kort (Monitoring in numbers, figures and maps, ssi.dk/data) where you will have the opportunity to generate your own reports and export data in Excel format. This webpage allows user to generate reports as from 2001, per year and month, age-group and sex, geography, infection abroad; and for salmonella, the data can be presented by the primary serotypes.
Salmonella
Salmonella infections are primarily characterised by use of serotyping. The majority of the serotypes are zoonotic and transmitted via foodstuffs. A large number of serotypes exist, but two - S. Enteritidis and S. Typhimurium - generally account for about two thirds of all salmonella infections in Denmark. The number of zoonotic salmonella cases registered in 2014 was 1,124 (19.7 per 100,000), which is nearly the same as the previous two years EPI-NEWS 11/14. In 2015, the number decreased to 925 cases, 18% less than in 2014 (16.2 per 100,000). Figure 1 shows the age-specific incidence. As in previous years, patients below 5 years of age accounted for a relatively high number of diagnosed salmonella infections. This also reflects that relatively more in this age group are tested for salmonella.
The ten most frequent serotypes are presented in Table 2. Furthermore, the table presents the number of the corresponding serotypes in 2014. In both years, S. Enteritidis and S. Typhimurium and the monophasic variant hereof accounted for the majority of infections: a total of 62% of all infections in 2014 and 54% in 2015. The second most frequent infections, each representing fewer infections per serotype, however, were serotypes that have also been among the most frequently occurring serotypes in recent years. A total of 94 different serotypes were registered in 2014 and 99 in 2015. In both years, the group Other serotypes seen in Table 3 thus comprises various serotypes each of which occurs very rarely. Many of these serotypes are acquired during foreign travel. Both in 2014 and in 2015, the monophasic variant of S. Typhimurium, including isolates with the antigen formula ”1,4,[5],12:i:-” was more frequently observed than S. Typhimurium.
Salmonella isolates are submitted to the SSI and are typed continuously by use of serotyping, DNA methods and, increasingly, whole-genome sequencing. This is primarily done to facilitate the detection of outbreaks. In 2014, a series of clusters of infections with the same types were detected and tested. Among these clusters, 12 were considered outbreaks. These underwent epidemiological investigation. In 2015, only few clusters of identical types were found: three outbreaks were recorded, one of which turned out to be an international outbreak. In Denmark, it comprised 14 cases and was caused by S. Oranienburg. This outbreak is currently still being investigated in cooperation with the European Centre for Disease Prevention and Control (ECDC).
Five outbreaks, detected among others by use of MLVA (multi-locus variable number of tandem repeats analysis), comprised more than 15 cases in 2014-15, Table 3. Four of these were caused by the monophasic variant of S. Typhimurium The outbreaks, which are described below, were investigated by the SSI in collaboration with DTU-FOOD and the Danish Veterinary and Food Administration. An S. Agona outbreak stretched across 9 months from August 2013 to April 2014. More than half of the total of 21 infected persons were less than 5 years old; the remaining were young men in their twenties plus some elderly persons. On the basis of the epidemiological investigation, a hypothesis was generated that the source might be whey powder used as an ingredient in e.g. infant formula/baby food, protein powder for muscle training or protein drinks given to elderly persons during their admission to hospital. This, however, could not be verified through trace-back and microbiological analysis. In the spring of 2014, an outbreak counting 22 patients occurred. The majority of patients resided in Jutland, and the outbreak investigation showed that the outbreak was caused by Danish pork sold directly from a local butcher and a supermarket chain. In the summer of 2014, an outbreak counting 25 patients occurred. The outbreak strains shared a specific MLVA and resistance profile. The Danish Food Institute DTU initially found various such strains in samples from an abattoir and a cutting plant, and subsequently patients were registered. The source was Danish pork. An additional two outbreaks occurred in the course of the summer of 2014. Both comprised isolates with a specific MLVA profile and antibiogram. The first of these outbreaks counted 19 cases and was caused by minced beef from a Danish producer. The second outbreak counted 15 laboratory-confirmed cases. This outbreak occurred at a summer camp, and the source of infection was not identified. Finally, the autumn of 2014 saw an outbreak counting 18 registered patients. This outbreak was caused by S. Enteritidis with a specific MLVA profile. In this latter outbreak, investigation was initiated after serious illness was established in a Danish egg-laying farm. Eggs from this farm were immediately recalled from the market and the flock culled. Nevertheless, a total of 13 persons had already fallen ill from eating eggs, while another 5 patients who fell ill had not ingested eggs from the same producer. Three of these had eaten eggs from other farms close by.
Information about travel related infections was collected through telephone interviews with patients, where such information was not part of the notifications. The patients were asked about the date of disease onset and whether they had travelled abroad within a 7-day period prior to disease onset. Information about country of infection was obtained for 71% of the salmonella patients in 2014 and 82% in 2015. Looking exclusively at the patient group for whom the country of infection is known, 46% were infected abroad in 2014 and 57% in 2015. This overall figure covers considerable variation between serogroups. For S. Enteritidis, the share of infections acquired abroad comprised 78%. For S. Typhimurium, the corresponding figure was 32%; for the monophasic S. Typhimurium 20%; and for all other salmonella groups, the share was 55%. Among these, the highest number of infections was seen in Turkey, representing a total of 139 patients. Followed by these other popular tourist destinations: Thailand with 132 patients, Spain with 56 patients, Sri Lanka with 43 patients, Egypt with 42 patients and Indonesia with 33 infected patients.
Campylobacter
In 2014, a total of 3,797 (67 per 100,000) Campylobacter spp infections were reported; nearly the same number as that recorded for the preceding year. In contrast, an increase in the number was seen in 2015, as the total registered was 4,348 (77 per 100,000) cases, corresponding to a 12% increase. The age-specific incidence (Table 1) shows how the disease burden is rather equally distributed across the age groups with a small excess rate among persons in their twenties, which is quite typical for campylobacter.
Campylobacter isolates are not normally submitted to the SSI for subtyping. Among the strains whose species were determined, the overall result was that approx. 93% of the strains belonged to C. jejuni and around 6% to C. coli. Campylobacter outbreaks are relatively rare. In the 2014-15 period, no water-borne outbreaks were described. In 2015, two food-borne campylobacter outbreaks were registered. One occurred in May among the employees of companies in the Copenhagen area who used a specific catering company as lunch provider. A total of 110 persons fell ill and the source of infection was not identified. The second outbreak occurred in connection with a scout camp in Jutland where 25 persons fell ill, and the investigation indicated that the source might be insufficiently roasted chickens, made over camp fires.
In 2014, information about the countries in which the patients had become infected was collected actively through continuous telephone interviews with patients notified by the departments of clinical microbiology in Odense and Aalborg, EPI-NEWS 12/13. For 2014, travel information was available in 73% of the registered cases from these two laboratory catchment areas; a total of 562 campylobacter cases. Hereof, 173 (31%) were acquired abroad. These telephone interviews stopped in 2015 because of the transition to MiBa data capture. For 2015, travel information was available in 43% of the registered cases; a total of 1,858 cases. Hereof, 659 (36%) were registered as having been acquired abroad. When all travel information is summarised for the two years, Turkey with 183 registered infections was the country where most patients had been infected, followed by Spain, Thailand Greece and France with 147, 115, 56 and 51 registered infections, respectively.
Yersinia enterocolitica
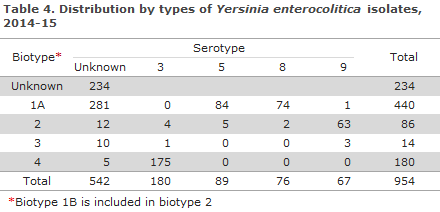
The number of registered Yersinia enterocolitica cases has increased consistently over the past 5 years (Figure 1). In 2014, a total of 415 cases were registered, 20% more than in 2013. A total of 539 cases (9.5 per 100,000) of Yersinia enterocolitica were registered in 2015; a 30% increase compared with 2014. The incidence is highest among children (Table 1), but adult cases also occur. Yersinia enterocolitica isolates are generally submitted to the SSI for bio-typing. The 2014-15 distribution on biotypes and serotypes is presented in Table 4. Among the submitted isolates (isolates were available for typing for approx, 75% of the detected infections), more than half (61%) were of biotype 1A.
In the beginning of 2014, an outbreak occurred with biotype 4 (serotype 3). The outbreak counted 24 disease cases of which 11 were less than 5 years old. Interviews with patients did not identify a common source of infection. In August-September 2015, an increase in the number of cases with the same biotype, mainly from Central Jutland, was once again observed. Three of 14 cases were connected to a handball tournament in the town of Kolding. However, interviews with sporadic cases did not allow identification of a specific food as the source of infection. This bio-serotype is frequently observed, and it was not possible to differentiate further between the strains to determine which cases may have been caused by a common source of infection.
Commentary
The number of salmonella infections decreased further from 2014 to 2015, thus continuing the positive trend seen in past years. For the first time in 30 years, 2015 recorded fewer than 1,000 annual salmonella cases. A considerable part of the explanation is that S. Enteritidis has been successfully eradicated from eggs and chickens produced for human consumption. Thus, since 2013, the Danish Veterinary and Food Administration has not advised against ingestion of raw eggs produced in Denmark. In both 2014 and 2015, less than 50 cases of S. Enteritidis infected in Denmark were registered. A decrease has also been seen in the number of registered infections with S. Typhimurium, which is traditionally associated with pork. Nevertheless, this decrease should be seen in connection with an increased occurrence of the monophasic variant of S. Typhimurium, which has spread rapidly among production animals and also among persons in the Western World in the course of the past decade. It is remarkable that the monophasic variant was more common than S. Typhimurium itself in 2014 as well as in 2015. Additionally, the monophasic variant gave rise to a series of disease outbreaks in 2014, whereas 2015 was characterised by unusually few salmonella disease outbreaks in general, which also contributed to the overall low number of infections.
The number of campylobacter infections remains high. For a number of years, campylobacter has been the most frequent cause of bacterial gastrointestinal infections, and it occurs much more frequently than salmonella. The same is seen in other parts of the Western World, and generally there seems to be a considerable infection pressure in most European countries. The overwhelming majority of infections occur sporadically, and an estimated 30-40% of Danish patients are infected abroad. The epidemiology of campylobacter is presently not fully understood, and we do not have a full understanding of the relative importance of the various routes of transmission. Several research projects and initiatives are under way, also at the SSI, EPI-NEWS 4/16.
Changes are expected to be introduced that will affect the Danish surveillance system for infectious diseases in years to come. The changes reflect both changes in laboratory practice, including the introduction of more sensitive diagnostic methods, and a gradual transition towards more electronic data capture. It is to be expected that the changes will affect disease statistics – although the disease burden may undergo no real change. Campylobacteriosis and yersiniosis are among the first conditions that will be comprised by the changes and they therefore serve as examples of what we may expect for other conditions in the future.
The reorganisation of the monitoring of campylobacter infections so that it is now predominantly based on automatic data capture in MiBa is believed to have improved survaillance. It is not possible to determine if the fact that the number of registered cases has increased in 2015 reflects a real increase, an unchanged number of cases or a decrease with respect to 2014. An additional factor that complicates the interpretation of surveillance data is the concurrent and gradual introduction of diagnostic PCR directly on faeces sample material in the Danish laboratories. Preliminary reports indicate that diagnostic PCR leads to more persons being diagnosed as the method is more sensitive than traditional culture. For this reason, an additional increase in the number of registered cases may be expected in years to come. A mismatch between the trend seen in the number of registered cases and the real trend in the number of disease cases is probably also seen for Yersinia enterocolitica. Automatic data capture based on MiBa has also been introduced there, and is believed to contribute to the observed increase from 2014 to 2015. Furthermore, a relatively large share of the infections is of biotype 1A. The pathogenicity and epidemiology of this biotype has yet to be fully established, but it has traditionally been considered a non-virulent or a moderately virulent type in humans. In the majority of our neighbouring countries, detection of biotype 1A is not notified. It is possible that a part of the increasing number of registered Yersinia enterocolitica infections seen in recent years may be attributable to the fact that the laboratory methods have evolved so that relatively more patients are diagnosed with biotype 1A.
(S. Ethelberg, L. Müller, K. Mølbak, Department of Infectious Disease Epidemiology. E.M. Nielsen, M. Torpdahl, Department for Microbiology and Infection Control)
Link to previous issues of EPI-NEWS
16 March 2016