No 34 - 2014
Syphilis 2013
Hospital departments and rehabilitation centres can now order hepatitis B vaccines
Syphilis 2013
2013 saw 352 notifications of newly acquired syphilis in 350 persons. A total of 327 (93%) were male and 25 (7%) were female cases. The median age was 38 years for males (range 16-77 years) and 30 years for females (range 0-57 years).
A total of 319 (91%) of the cases were notified to the Notification System for Infectious Diseases (NSID), the Department of Infectious Disease Epidemiology (DIDE). A total of 191 (54%) of the cases were both notified to the NSID and a specimen had been submitted to the Department of Microbiological Diagnostics and Virology, the SSI (DMDV), whereas 128 cases (36%) were notified to the DIDE and diagnostically confirmed at another laboratory. Additionally, 33 cases (10%) were diagnostically confirmed at the DMDV, but not notified with the NSID. Finally, the NSID received 32 notifications which the DMDV established were not current syphilis.
As in previous years, the majority of the cases resided in the Copenhagen area, Table 1. In 2013, a total of 30 cases were notified for which no data were entered into the field of residence. Furthermore, in 33 cases that were confirmed at the SSI's laboratory, the patient's residence was not stated. The majority of these cases were diagnosed in the Copenhagen area.
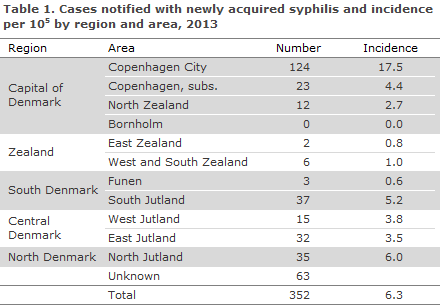
Consequently, the total number of cases recorded in the Copenhagen area was 147. However, as the majority of the cases with unknown residence were diagnosed in Copenhagen, the number may reach 210. This is lower than in 2012 when 236 cases were recorded. In contrast, the total number of cases recorded for Jutland in 2013 was 119 compared with 64 in 2012.
The majority, 263 (83%) of the notified cases, were Danish-born persons, whereas 39 (12%) were immigrants, 4 (1%) were second-generation immigrants and 4 (1%) were tourists. For 9 of the notified cases (3%), the country of origin was not stated.
Syphilis diagnostics
Among the 224 syphilis cases for which samples were submitted to the DMDV, 183 (82%) were detected by serology, 19 (8%) by serology as well as PCR, and 22 (10%) cases were exclusively detected by PCR.
Congenital syphilis
A single case of congenital syphilis was notified in 2013. The child was born in Denmark by a woman who screened negative to syphilis at the beginning of her pregnancy, but who became infected after her screening.
Syphilis antibodies were detected in 4 neonates whose mothers had been diagnosed as syphilis positives in the pregnancy screening. In all 4 cases, only maternal antibodies were detected. Nevertheless, treatment was administered in 2 of the children as their mothers had received treatment so late in the course of the pregnancy that full treatment effect could not be guaranteed.
Transmission
The 319 cases that were notified to the DIDE occurred in a total of 318 persons as 1 male was notified with two syphilis episodes in the course of the year. Among these 318 persons, 20 were heterosexually infected females (6% of all notified persons), 36 were heterosexually infected males (12% of the notified males), 250 were men who have sex with men (MSM, 84% of the notified males) and 11 were males whose route of infection was unknown (4% of the notified males). Furthermore, 1 neonate was notified.
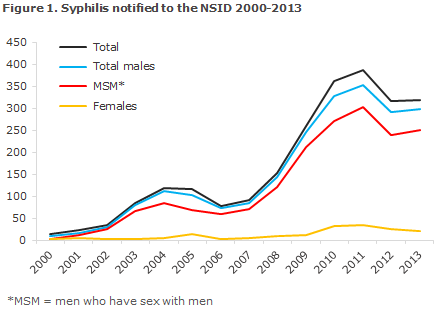
Figure 1 presents the number of persons notified with sexually transmitted syphilis since 2000. The country of infection was stated for 270 (85%) of those notified, 16 females and 254 males. Among males, a total of 222 (87%) were infected in Denmark, and among girls/females the corresponding number was 11 (69%).
Among heterosexually infected males, 23 (72%) were infected in Denmark, while this was the case for 196 (90%) of MSM.
Syphilis and HIV
Information on HIV status was available for 269 males (96% of MSM, 77% of heterosexually infected males and 73% of males for whom the mode of infection was not stated), and for 17 (81%) females.
Among HIV-tested males, 79 (29%) were HIV positives. A total of 74 HIV positives were detected among 234 MSM (32%), 4 HIV positives were found among 27 heterosexually infected males (15%), and the mode of infection was unknown for the last HIV positive male.
Among the 79 HIV positive males, 12 had been diagnosed with HIV and syphilis simultaneously (11 MSM and 1 male for whom the mode of infection was not stated), whereas 49 were known HIV positives prior to their current syphilis diagnosis. One non-Danish female was known to be HIV positive. For the remaining 18 cases, there was no information on the time of their HIV diagnosis.
Commentary
The nationwide decrease in the number of cases observed in 2012 compared with 2011 has not continued. The number of notifications is now in line with that observed last year,EPI-NEWS 34/13.
The majority of the 63 cases for whom no residence was stated were diagnosed in Copenhagen, but even if all of these are counted as part of the Copenhagen area, the total number was lower than that observed in 2012. Conversely, in 2013 nearly twice as many cases of syphilis were recorded in Jutland as in 2012. In the Capital Region of Denmark, the confirmatory tests were not only performed at the DMDV.
The decrease in the Greater Copenhagen area may therefore be due to some cases not being notified if they are not confirmed by the DMDV which routinely submits a NSID notification form to anyone ordering a test. Nevertheless, the increase observed in Jutland is probably real.
In Denmark, syphilis continues to occur primarily among MSM, and - in contrast to gonorrhoea - no substantial increase has been seen in the number of cases among heterosexually infected persons.
A single case of congenital syphilis was notified in 2013. The pregnant woman tested negative at her pregnancy screening, but subsequently became infected with syphilis. Generally, the pregnancy screening is well-functioning, and a single case such as this one does not mean that all pregnant women should be screened several times during their pregnancy, EPI-NEWS 22-23/14.
Syphilis is a marker of unprotected sex, and therefore also a marker of the risk of HIV infection and of infection with other sexually transmitted diseases. It is therefore still important that MSM who are tested for syphilis also be tested for HIV,EPI-NEWS 46/09, lymphogranuloma venereum (LGV), hepatitis B & C, and gonorrhoea.
PCR testing is expedient for detection of Treponema pallidum in chancre material and is often positive before any antibodies can be detected.
Correct diagnosis and staging are important for the treatment of the individual syphilis patient as well as for monitoring efforts. Tentative diagnoses based on positive serological screening results should therefore be verified trough extended serological tests.
Newly acquired syphilis, i.e. primary and secondary syphilis, is notified to the Department of Infectious Disease Epidemiology, Statens Serum Institut (SSI) on Form 1510, which is available for download at www.ssi.dk
(S. Cowan, Department of Infectious Disease Epidemiology, S. Hoffmann, Microbiology and Infection Control)
Hospital departments and rehabilitation centres can now order hepatitis B vaccines
In pursuance of Executive Order on free hepatitis vaccination for particularly exposed groups of persons, persons with hepatitis C may receive hepatitis B vaccination free of charge.
The vaccination used may be a combination of hepatitis A and B vaccine, or simply hepatitis B vaccine, at the discretion of the vaccinating physician.
Until now, the vaccine has only been available from the SSI at the expense of the region and provided that the person placing the order had a provider number. In practice this means that only GPs could order the vaccine.
Now, however, the SSI's Order Office can provide the vaccine, at the expense of the region, for hospital departments and rehabilitation centres. Hospital departments order the vaccine through their hospital pharmacy. When ordering, the patient's civil registration number shall be provided.
At larger departments and rehabilitation centres, persons covered by the executive order can receive the vaccination without a prior appointment. In these cases, it is not possible to order the vaccine beforehand to the person in question. It may therefore prove practical to store a limited supply of the vaccine, and then order the free vaccine after the vaccination has been administered.
(Department of Infectious Disease Epidemiology)
Link to previous issues of EPI-NEWS
20 August 2014