No 42 - 2025
Invasive meningococcal disease 2024
Invasive meningococcal disease 2024
- In 2024, 26 cases of invasive meningococcal disease (MD) were registered in Denmark, which is a decrease of about 20% compared with 2023.
- The median age among those affected was 37 years (range 0–93 years). The highest incidence was seen among children under 1 year of age, and there were more cases among women than men.
- Group B was dominant (46% of cases), followed by group Y (27%) and group W (15%). Group W, which had previously been increasing sharply, was again detected but in smaller numbers (4 cases). No cases of groups A, C, X, Z, or 29E were reported.
- Two patients died of MD in 2024 (groups W and Y), and three patients developed serious sequelae (two with hearing loss, one with arthritis).
- When MD is suspected, close contacts are offered antibiotics and vaccination if the identified group of Meningococcus allows for vaccination. In 2024, 103 close contacts were offered vaccination, but it was only a little over half that received the vaccine from Statens Serum Institut (SSI).
For a more detailed description, please refer to the annual report on invasive meningococcal disease in 2024.
Statens Serum Institut (SSI) surveils MD to ensure rapid contact tracing, prevention of secondary cases, and targeted vaccination of close contacts. MD includes invasive cases such as meningitis, sepsis, or detection of meningococci in normally sterile sites.
MD must be reported both by phone and in writing, ensuring coordination between the Danish Patient Safety Authority (STPS), SSI, and clinical microbiology departments. Reporting and submission of biological material are essential to determine the bacterial group and to provide targeted vaccination to close contacts.
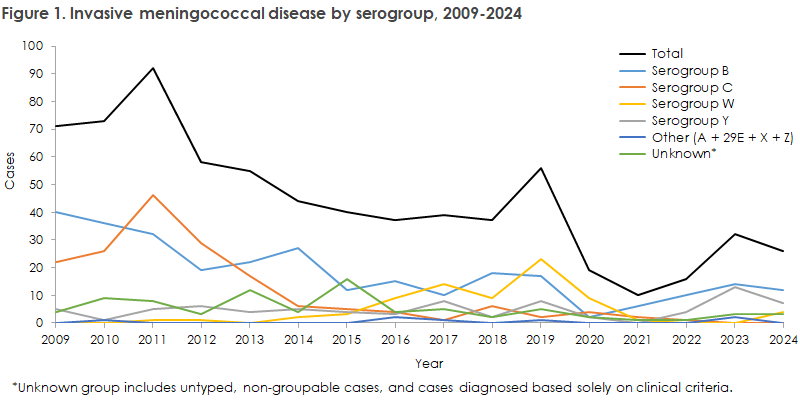
In 2024, 26 cases of MD were registered in Denmark, corresponding to an incidence of 0.4 per 100,000 inhabitants. The level was similar to recent years but lower than before the COVID-19 pandemic, when the incidence was up to 1.0 in 2019, see Figure 1.
The cases were spread across the country, though most were in the Greater Copenhagen area and East Jutland, with a median age of 37 years. The highest incidence occurred among infants under 1 year of age, and more cases were seen among women than men.
There were seven patients with meningitis, eight with sepsis, and nine with both. Two were reported based on clinical symptoms only. The most frequent serogroups were group B (46%), Y (27%), and W (15%), while in three cases the group was not determined. Group B occurred in all age groups, while group Y was mainly seen in people over 40 years of age. Group W, which peaked in 2019, was again detected in four patients after being absent in 2022 and 2023.
Most patients were infected in Denmark. Two deaths were recorded in 2024 (groups W and Y), and three patients had sequelae such as hearing loss or rheumatoid arthritis. All isolates were fully susceptible to relevant antibiotics (ceftriaxone, ciprofloxacin, penicillin, and rifampicin).
Prevention of infection occurs through rapid contact tracing, antibiotic treatment, and possible vaccination of close contacts. In 2024, 103 people were offered vaccination, but vaccines were only distributed to just over half. SSI is working to improve registration of vaccine distributions.
It is important that general practitioners pay attention to patients who are close contacts of an MD patient and who contact them after receiving a vaccination offer from STPS. Patients receive a letter in their digital mailbox (Digital Post/E-boks) from STPS with the vaccination offer, and it is important that they are scheduled for vaccination as soon as possible. The vaccine can be obtained free of charge by contacting the on-call epidemiologist at SSI (tel. 32683038), and the vaccine should be administered no later than 4 weeks after exposure.
(N. Filipsen, I.R. Moustsen-Helms, B. Søborg, Department of Infectious Disease Epidemiology and Prevention; S. Hoffmann, Department of Bacteria, Parasites, and Fungi, Infectious Disease Preparedness)