No 6a - 2024
Another two measles cases
Leishmaniasis diagnosed in Denmark, 2011-2022
Another two measles cases
Last week, Statens Serum Institut (SSI) detected a case of measles, EPI-NEWS 5/2024. The SSI has now detected two additional measles cases in a child and an adult person residing in the North Denmark Region.
The child and the adult family member both had a history of travel to Eastern Europe, where they had stayed with their family for Christmas. During their stay, a family member of the adult was diagnosed with measles.
The above description reflects that cases are currently being observed in various European countries.
Through the international reporting systems, the SSI has been warned of two travellers who transited through Copenhagen Airport, Kastrup, and were subsequently diagnosed with measles.
Measles is transmitted by airborne infection why non-immune travellers who, e.g., stayed in the same section of a transit area as the two affected people may have been exposed to infection.
The Danish Patient Safety Authority has been informed and has initiated infection tracing measures in relation to the contacts of the infected persons, private as well as any healthcare and transport sector contacts who may have been exposed to infection before being diagnosed.
Physicians are encouraged to remain extra attentive to the measles diagnosis in weeks to come. Additionally, the current cases of infection may serve as an opportunity to inform non-immune patients of the opportunity to be vaccinated free of charge. For practical purposes, it is safe to assume that anyone born before 1975 is naturally immune to measles.
It is important that any person who is suspected of having measles avoids being in waiting rooms with other patients as measles is extremely infectious.
Sampling
On suspicion of measles, the following samples should be taken:
- Pharyngeal swab and urine for detection of measles virus (morbili virus) RNA by PCR. The greatest possibility for detecting measles virus is in the early phases of the disease course, but the virus is frequently detectable for several weeks after the acute disease occurs. A negative finding does not exclude measles.
- A blood sample for measles virus IgM/IgG antibody determination. IgM antibodies may be confirmed by rash.
We recommend that all measles virus-positive samples be sent to the National WHO Reference Laboratory for Morbilli and Rubella, Laboratory for Virus Surveillance and Research, SSI, for characterisation, which is free of charge.
On suspicion of measles disease, it is important that the diagnostics and work-up are performed as rapidly as possible with a view to continued isolation of the patient and also tracking and, if relevant, treatment of any non-immune persons who may have become exposed to infection. Serological detection is insufficient for measles diagnostics, and virus detection by PCR is necessary.
Virus detection by PCR analysis is the quickest and safest method for laboratory diagnostics of measles. The analysis may be performed at the SSI, among others.
The National WHO Reference Laboratory for Measles and Rubella at the SSI handles the characterisation (sequencing and typing) of all measles virus-RNA-positive samples in Denmark. As characterisation of the measles virus is important in relation to infection tracing and mapping, all suspected and confirmed measles virus-positive samples should be forwarded to the Reference Laboratory as quickly as is practically possible. We recommend contact by phone to the virologist in charge at the SSI (in the daytime pho.: 40336379, after 15.30 to the virologist on call pho.: 41317404) to inform the laboratory that samples are underway and thereby avoid any unnecessary delay of the diagnosis.
For further details, please see the SSI's measles theme page.
Vaccination and prophylaxis following exposure
The primary form of prevention is MMR vaccination. In Denmark, MMR vaccination is offered to all children at 15 months and four years of age as part of the Danish childhood vaccination programme. Currently, no recommendation has been made to advance the time of vaccination. However, upon request, the initial MMR vaccine may be given as from 12 months of age and will then still count as part of the vaccination programme, also if given concurrently with the third Pentavac and the third Prevenar13.
Following certain exposure to infection, i.e. contact to a laboratory-confirmed or epidemiologically linked case, MMR vaccination may be given within three days of exposure to infection and normally human immunoglobulin within six days as post-exposure prophylaxis (PEP) to non-immune contacts. Delimitation of the contacts who need PEP is done by the on-duty physician at the Danish Patient Safety Authority, Division for Supervision and Guidance of the area in question. Subsequently, expenses are reimbursed by the regional authorities.
For more details on post-exposure prophylaxis, please see here.
Notification
As from 1 November 2023, measles is notifiable by phone to the Danish Patient Safety Authority, Supervision and Guidance East/West in case of enhanced suspicion or confirmed measles disease, EPI-NEWS no. 44b/2023. Additionally, confirmed measles cases are notifiable in writing to the Danish Patient Safety Authority, Division for Supervision and Guidance East/West as well as to the SSI. Notification is made via the electronic notification system (SEI2). See link for further information and guidance.
(K. M. Jørgensen, K.T. Franck, Virus Monitoring & Research, National Reference Laboratory for Measles and Rubella, L.K. Knudsen, J. Grau. P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention, I. Brandenburg, Danish Patient Safety Authority, Supervision and Guidance West)
Leishmaniasis diagnosed in Denmark, 2011-2022
Leishmaniasis is caused by the Leishmania parasite, which is transmitted to humans by sand flies (of the Phlebotomus and Lutzomyia genera). Globally, the condition is mostly found in a number of tropical and subtropical areas, including some parts of Southern Europe. Three main leishmaniasis disease types exist: Cutaneous leishmaniasis, which causes wounds in exposed body areas; muco-cutaneous leishmaniasis, which affects the mucous membranes, primarily in the nose and mouth; and visceral leishmaniasis, which mainly affects the internal organs and may cause fever, weight loss, enlargement of the liver and spleen, and can be fatal without specific treatment. It is important to remain aware that immuno-suppressed people are at special risk of serious manifestations and that the infection can remain latent only to cause symptoms when the immune system is weakened.
In the 2011-2022 period, the Danish National Patient Registry (NPR) recorded a total of 169 persons with the ICD10 diagnosis code (DB55) of leishmaniasis, corresponding to an average 14 persons annually. In the same period, Statens Serum Institut (SSI) performed 1,941 leishmaniasis tests in 1,526 patients. The tests included 590 PCR tests for detection of Leishmania DNA and 1,351 antibody tests for detection of visceral leishmaniasis, of which 121 were positive. For the period as a whole, the positive rate for PCR tests was 17% (85/494 persons), whereas the corresponding rate for antibody tests was 1.4% (17/1,254 persons). A trend was observed towards an increasing number of antibody analyses being performed, but the positive rate remained low. In contrast, an increase was seen in positive PCR tests in the period leading up to 2017, after which a decline was observed, followed by another increase in 2022. This may possibly be explained by increased travel activity and/or more migrants as from 2016 and then declining travel activity during the COVID-19 pandemic.
The number of tested and positive persons is presented in Table 1, by sex and age. Both were equally distributed across Denmark.
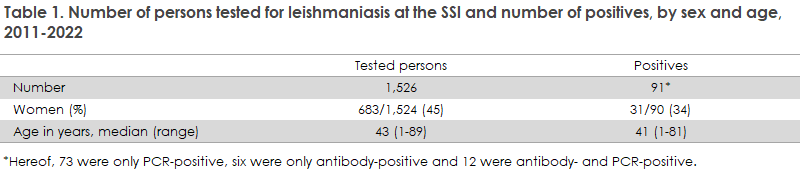
The difference between the number of patients with a diagnosis code (n=169) and the number with a positive microbiological test (n=91) is likely explained by some patients being diagnosed based exclusively on histological examination.
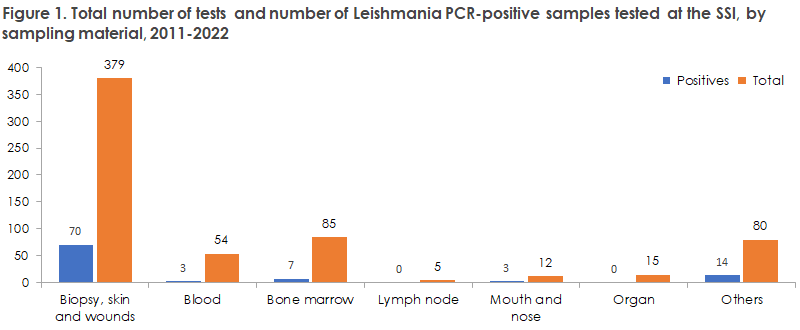
The overwhelming majority of samples submitted for PCR analysis were skin or wound biopsies, followed by blood and bone marrow. The total number of tests and the number of PCR-positive samples are presented by sample material in Figure 1.
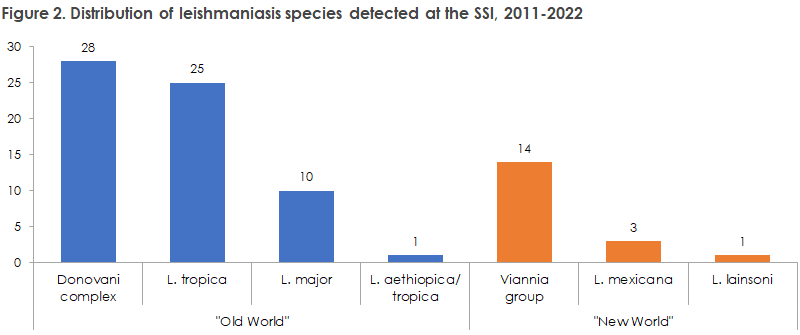
In Denmark, the most frequently detected species belonged to the Donovani complex (comprising L. donovani and L. infantum), followed by L. tropica, the Viannia group (L. braziliensis, L. guyanensis, L. panamensis and L. peruviana) and L. major and then, more rarely, L. mexicana, L. aethiopica and L. lainsoni, Figure 2. The species of samples from three patients could not be determined.
A total of 70 (70/85, 82%) presumed cases of cutaneous leishmaniasis were detected, along with nine (9/85, 11%) cases of presumed visceral leishmaniasis and one presumed case of muco-cutaneous leishmaniasis (1/85, 1%). Furthermore, the leishmaniasis type of the final five cases were unknown (5/85, 6%). As the above categorisation is based exclusively on data from sample orders and test results from the SSI, these results must be interpreted with caution. The antibody tests performed on the presumed cases of visceral leishmaniasis yielded either positive (6/7) or grey-zone (1/7) results.
This is the first report to be published on leishmaniasis diagnosed in Denmark since 2016, EPI-NEWS 51/2016. However, the report does not provide important information about exposures and travel history or symptoms and general epidemiology.
In the new executive order on notification of infectious diseases in Denmark (Executive Order on Notification of Infectious Diseases (retsinformation.dk)), which came into force on 1 November 2023, Leishmania is comprised by mandatory laboratory-based surveillance. We expect this will enhance the surveillance of leishmaniasis in Denmark.
(M. Zangenberg, R. Stensvold, H.V. Nielsen, Department of Bacteria, Parasites and Fungi, L. S. Vestergaard, Infectious Disease Epidemiology and Prevention)