No 46a - 2021
DANMAP 2020
DANMAP 2020
The DANMAP report describes the results of the national monitoring of antimicrobial resistance and antimicrobial consumption in humans, animals and foods in Denmark. In the DANMAP 2020 report, we also analyse the impact of the COVID-19 pandemic on the consumption of antimicrobials for humans. The DANMAP cooperation has been in place since 1995, publishing new annual reports annually. The publication of the DANMAP 2020 report celebrates the 25th anniversary of the DANMAP collaboration which marks the introduction of Summary DANMAP 2020. Summary DANMAP 2020 describes the primary findings related to the consumption of antimicrobials and the prevalence of antibiotics resistance.
DANMAP 2020 and the Summary DANMAP 2020 are available at www.danmap.org.
Below, we describe the main findings for 2020.
Antimicrobial consumption in humans
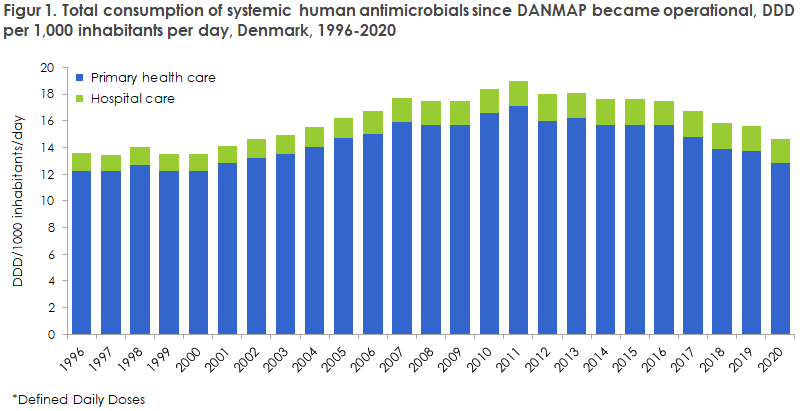
In 2020, the overall human antimicrobial consumption was 45.1 tonnes, corresponding to 14.71 defined daily doses per 1,000 inhabitants per day (DID), which is 6.7% lower than the 2019 consumption (15.77 DID) and 22.3% lower than the consumption recorded ten years ago (18.95 DID). In Denmark, primary healthcare is responsible for 90% of the antimicrobial consumption, whereas the remaining 10% are used in hospitals. Figure 1 presents the development in the consumption of human antimicrobials over the past 25 years.
Antimicrobials in primary healthcare
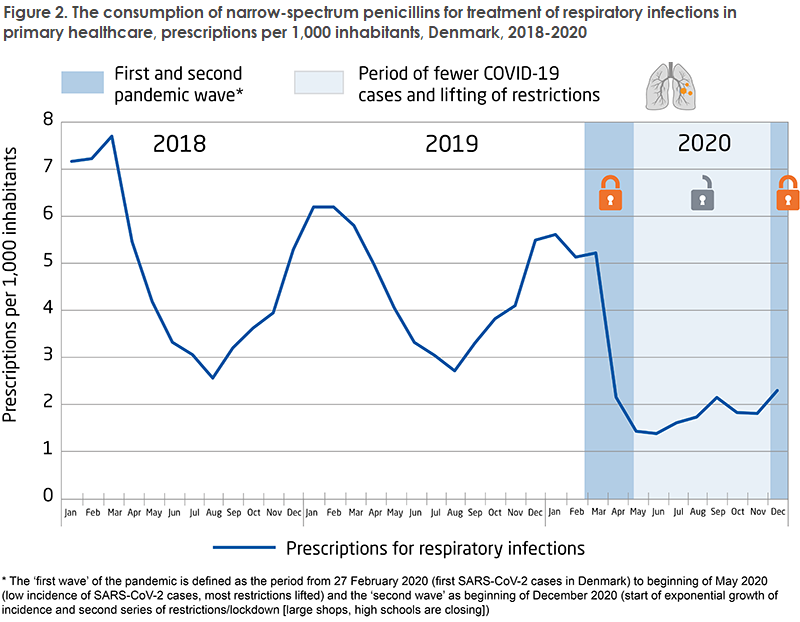
In primary healthcare, consumption of antimicrobials peaked in 2011. Subsequently, consumption has declined by 25%. From 2019 to 2020, consumption decreased by approx. 6.8%. The decrease observed from 2019 to 2020 was driven by a considerable decline in the consumption of narrow-spectrum penicillins (-17%). Figure 2 shows that the consumption of narrow-spectrum penicillins for treatment of respiratory infections was considerably lower in 2020 than in 2018 and 2019. This was very likely owed to COVID-19 restrictions, which also reduced the spreading of respiratory infections. This was particularly evident among the youngest age group (0-9-year-olds), where the consumption of antimicrobials declined by up to 54%.
Antimicrobials in hospitals
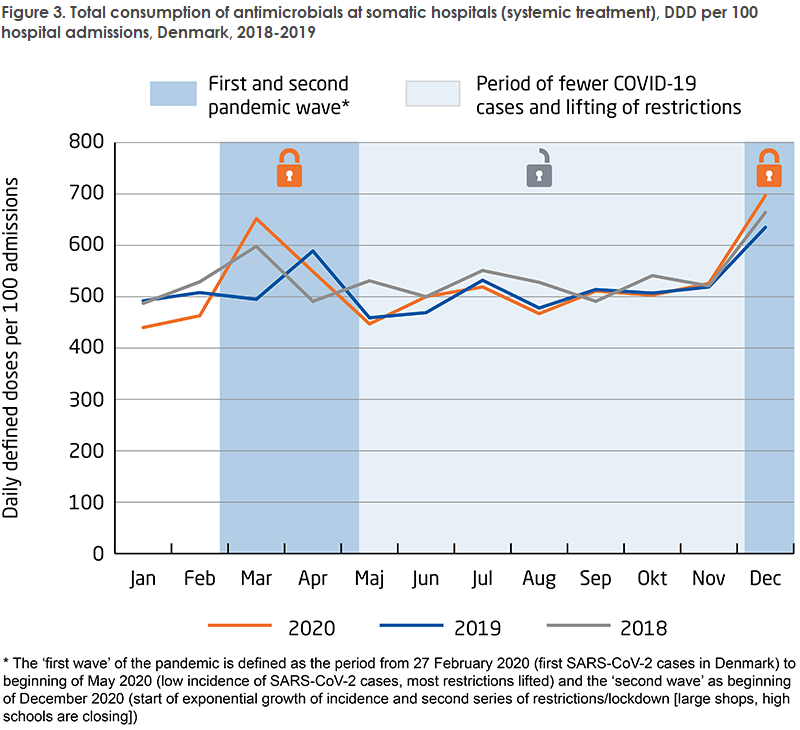
The consumption of antimicrobials in hospitals continues to follow an increasing trend, even when stated relative to hospital activity. In ten years, the consumption of antimicrobials in hospitals has increased by 33% (stated as DDD per 100 bed days); and from 2019 to 2020, consumption increased by 3.8%. The COVID-19 pandemic also affected antimicrobial consumption at hospitals, which was higher during the first and second pandemic wave compared to the same period in 2018 and 2019, Figure 3. This may possibly be explained by fewer but more seriously ill patients in the period.
National action plan for antimicrobials for humans
The National Action Plan for Antimicrobials for Humans published in 2017 aims to reduce consumption of antimicrobials, to increase the use of narrow-spectrum rather than broad-spectrum antimicrobials and to reduce consumption of critically important antimicrobials in hospitals (cephalosporins, fluoroquinolones and carbapenems). In 2020, the objective of reducing antimicrobial consumption in the primary sector was reached (329 prescriptions per 1,000 inhabitants per year). However, the share of Penicillin V was not increased, but decreased to 27% of the total consumption in 2020.
The consumption of critically important antimicrobials at hospitals declined by 7.2% in the period from 2016 to 2020. However, the consumption increased by 3.8% from 2019 to 2020. The objective in the action plan was a 10% reduction from 2016 to 2020.
The Danish Ministry of Health has decided to extend the action plan through 2021, as COVID-19 exerted pressure on Danish healthcare in 2020, thereby limiting the opportunities to engage in targeted work to meet the established objectives.
Antimicrobial consumption in animals
In 2020, the total consumption of antimicrobials for animals was 99.5 tonnes. Consumption has declined by 28 tonnes (22%) in the course of a decade but increased by 2% from 2019 to 2020. Consumption of antimicrobials for animals is driven by pig production, which accounts for 76% of total consumption. For comparison, consumption for cows accounted for 12%, and other animals (horses, birds, fur animals, fish farming and pets) accounted for another 12%.
Specifically, for pig production, the consumption increased by 4.5%. Thus, it has not been possible to reach the national action plan objective of reducing antimicrobial resistance in production animals and foods in the 2021-2023 period by 2% annually relative to the 2018 consumption. Furthermore, the consumption of medical zinc increased by 4% from 2019 to 494 tonnes in 2020. As from June 2022, the consumption of medical zinc must cease in the EU for environmental reasons and to reduce the risk of developing antimicrobial resistance.
Antimicrobial resistance in clinical bacteria in humans
The occurrence of antimicrobial resistance in human pathogenic bacteria in Denmark remained largely stable in 2020. However, a decline was observed in travel-related and community-acquired infections. The number of invasive infections continued increasing, driving antimicrobial consumption at hospitals which is relatively high, even in a European perspective. Therefore, it remains important to focus on reducing antimicrobial consumption and to use narrow-spectrum antimicrobials whenever possible.
Invasive infections
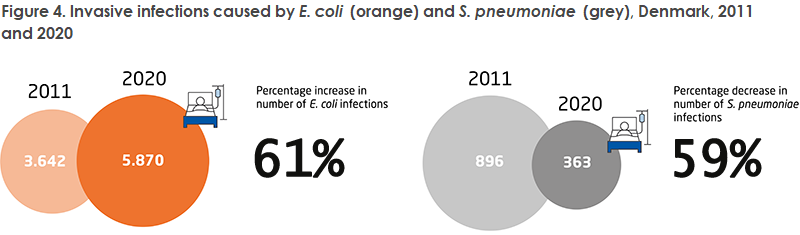
Escherichia coli (E. coli) is the most frequent cause of invasive infections in humans. The number of invasive infections caused by E. coli has increased by 61% in ten years. This may, among others, be due to an increasing number of risk-group patients (elderly, immunosuppressed and comorbid patients, among others) and an increase in the number of invasive and advanced procedures performed.
Streptococcus pneumoniae (S. pneumoniae) is the only bacterium that has caused fewer invasive infections. From 2011 to 2020, the number of invasive infections caused by S. pneumoniae declined by 59%. This coincides with the introduction of the pneumococcal vaccine in the childhood vaccination programme in 2007. In 2020, the national COVID-19 restrictions may be the reason why even less spreading of S. pneumoniae occurred.
The number of ESBL- and/or AmpC-positive E. coli isolates decreased by 6% from 2019 to 2020. Monitoring of these E. coli is important as ESBL- and/or AmpC-positive bacteria are resistant to most betalactam antimicrobials.
For K. pneumoniae isolates from invasive and urinary tract infections, a decrease has also been seen in the resistance to important antimicrobials (3rd-generation cephalosporins, gentamicin, cefuroxime and ciprofloxacin) over the past ten years. The reduced resistance to 3rd-generation cephalosporins is a positive trend, which coincides with a lower consumption of 2nd and 3rd generation cephalosporins at hospitals as from 2017.
On the other hand, the number of carbapenem-resistant invasive K. pneumoniae isolates has increased since 2011 and comprised 0.8% in 2020. Additionally, a decrease was observed in the sensitivity to piperacillin-tazobactam in 2020, which may have been caused by increased consumption of piperacillin-tazobactam at hospitals. Carbapenems and piperacillin-tazobactam are important antimicrobials for treatment of infections in humans, why the occurrence of resistance to these antimicrobials is followed closely.
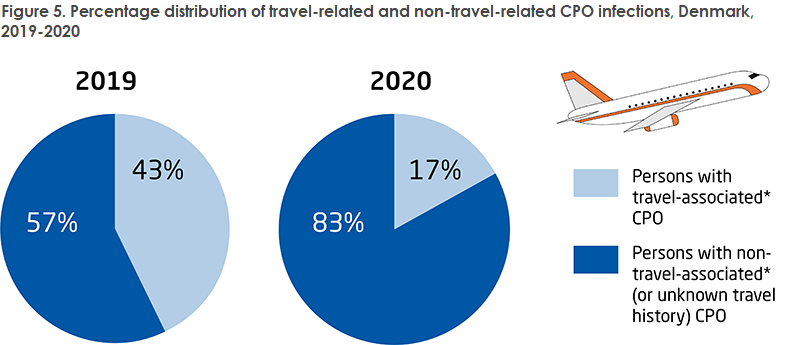
The occurrence of multi-resistant bacteria CPO (carbapenemase-producing organisms) has also continued its increasing trend from 2019 to 2020 despite far more limited travelling activity due to COVID-19 restrictions (from 221 cases in 2019 to 238 cases in 2020). Nine new hospital outbreaks caused by carbapenemase-producing enterobacteriaceae (CPE) were identified in 2020 in addition to the already existing 11 outbreaks in Danish hospitals. It is worrying that the continued increase is primarily caused by spreading of the infection at hospitals. It is therefore still important to focus on the general and supplementary infectious hygiene precautions in daily work.
The number of invasive vancomycin-resistant and vancomycin-variable enterococci (VRE/VVE) remained stable from 2019 to 2020. This is a positive finding and the result of joint efforts made by clinicians and infectious hygiene teams to fight outbreaks in Danish healthcare in combination with the implementation of preventive measures. The number of linezolid-resistant enterococci (LRE) and linezolid-vancomycin-resistant enterococci (LVRE) continued to be low in 2020 (seven and eight isolates, respectively). The treatment options are very limited in LVRE infections, and therefore the development is followed closely.
The number of patients who had Staphylococcus aureus detected in their blood increased by 5% from 2019 (2,233 cases) to 2020 (2,342 cases). Of these, methicillin-resistant Staphylococcus aureus (MRSA) comprised 2% (38 cases), among which 11 cases were of the livestock MRSA type CC398.
Monitoring of MRSA (infections and healthy carriers) showed a 21% decrease in 2020 compared with 2019. This is probably owed to reduced travel activity, social contact and access to hospitals in 2020 due to COVID-19 restrictions. Even so, 2020 saw more MRSA outbreaks at Danish hospitals and nursing homes where neonatal departments, in particular, were heavily affected with seven outbreaks involving a total of 59 patients, EPI-NEWS 25-26/21. However, the outbreaks observed in 2020 involved fewer patients (31 outbreaks with 130 patients in 2020 compared with 23 outbreaks with 157 patients in 2019).
Resistance in zoonotic bacteria, i.e., bacteria that transmit (directly or indirectly) from animals to humans
Like in the preceding years, 2020 recorded a high level of resistance in Campylobacter jejuni (C. jejuni) in patients who had recently been travelling abroad compared with infections acquired in Denmark. Macrolide (erythromycin)-resistant C. jejuni were observed in 3% of patients with a known travel history, whereas no macrolide resistance in C. jejuni was detected in patients who had acquired the infection in Denmark. In contrast, fluoroquinolone resistance (ciprofloxacin) was observed frequently in travel-related cases and also in cases acquired in Denmark, as 79% and 47% of C. jejuni isolates, respectively, were resistant to ciprofloxacin.
With respect to Salmonella, the DANMAP monitoring efforts are focused specifically on S. Typhimurium. For this serotype, more than half of the human infections are caused by a closely related clone that is resistant to ampicillin, sulfonamide and tetracycline. The COVID-19 pandemic caused a reduction in the number of travel-associated Salmonella infections, and therefore it was not meaningful to report resistance data separately for the travel-associated cases. Among Salmonella, resistance to critical antimicrobials, i.e., 3rd-generation cephalosporins, carbapenems, gentamicin and colistin, is only rarely observed (< 1% for cephalosporin and no carbapenem-resistance in S. Typhimurium in 2020). Resistance to fluoroquinolones (ciprofloxacin) was observed in < 1% of isolates from infections acquired in Denmark and in 3% of all isolates. Less than one percent of S. Typhimurium isolates were resistant to azithromycin.
International antimicrobial day on 18 November 2021
In collaboration with DTU FOOD, Statens Serum Institut celebrates the European Antibiotic Awareness day on 18 November 2021 by inviting people to attend the DANMAP seminar. At the seminar, the DANMAP team will present the primary highlights from DANMAP 2020, after which invited speakers will present other relevant topics.
The campaign material is available, in Danish language, here: Antimicrobials or not. Finally, the European Centre for Disease Prevention and Control (ECDC) also publishes campaign material to mark the day. These materials are available here: Home | EUROPEAN ANTIBIOTIC AWARENESS DAY (europa.eu).
(B. Borck Høg, DTU Food, M. Attauabi, J. Boel, M. Lindegaard, B. Müller-Pebody, A. Rhod Larsen, Department of Bacteria, Parasites and Fungi)
17 November 2021