No 36 - 2021
Purulent meningitis 2019 and 2020
Purulent meningitis 2019 and 2020
- 2019 saw a total of 106 notified cases of purulent meningitis. This was a considerable decline compared with 2018, when a total of 159 cases were registered. The decline was mainly caused by a considerable drop in the number of pneumococcal meningitis cases; from 77 cases in 2018 to 44 cases in 2019.
- In 2020, the decline in the number of purulent meningitis cases continued. Thus, at the end of 2020, a total of 72 cases had been recorded. The decline should be understood in the context of the comprehensive and prolonged lock-down of the community in connection with the COVID-19 epidemic. The social restrictions produced a drop in various airway and food-borne infectious diseases. Thus, the decline in the number of purulent meningitis cases was distributed on all types of agents between 2019 and 2020. The most substantial decline observed was that of meningococcal meningitis, which dropped from 25 cases in 2019 to ten cases in 2020.
- In both 2019 and 2020, more than half of the purulent meningitis cases occurred in persons with underlying disease or meningitis risk factors.
- In 2019 and 2020 overall, a total of 43 of 88 (49%) cases of pneumococcal meningitis were caused by serotypes included in the 23-valent pneumococcal vaccine (PPV23).
Persons who have turned 65 years old and persons who are at a specially high risk of invasive pneumococcal disease (IPD) are offered 23-valent pneumococcal vaccination free of charge. We expect that at some point in 2021, the programme will be extended to include more risk groups who have not yet turned 65 years old. At the SSI website, you can read more about the vaccination offer for persons who are at a specially high risk of invasive pneumococcal disease. - In 2019, one case of vaccine failure was notified; a child with Haemophilus influenzae serotype b infection who had been vaccinated twice.
- 2020 also saw one case of vaccine failure in a child who had been vaccinated with three doses of the Prevenar 13 vaccine, but even so was affected by pneumococcal infection caused by a serotype included in the vaccine (serotype 19A).
- In 2019, two cases of purulent meningitis were caused by infection with the bacterium Capnocytophaga canimorsus, which forms part of the normal flora in the oral cavity of cats and dogs, among others. Both patients had come into close contact with a dog.
- In 2019, the overall mortality for purulent meningitis was 17% (18 deaths). The corresponding figure for 2020 was 14% (ten deaths).
For a detailed description of the incidence, please see the 2019 and 2020 annual reports on purulent meningitis.
Meningococcal meningitis in 2019 (25 cases) and 2020 (10 cases) is described in EPI-NEWS 3-5/21 and in the 2019 and 2020 annual reports on meningococcal disease.
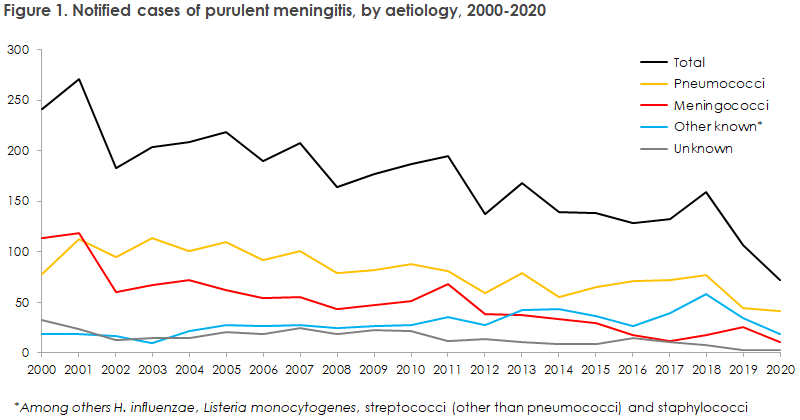
As presented in Figure 1, in 2019 the number of purulent meningitis cases was in line with the lowest number recorded since the turn of the millennium, a number which declined further in 2020. 2020 was characterised by a number of comprehensive and prolonged social restrictions in connection with the COVID-19 epidemic, which presumably produced a decline in various infectious diseases.
This includes airway diseases like influenza as well as food-borne diseases. Thus, the decline in purulent meningitis from 2019 to 2020 was distributed on all types of agents, but the more substantial decline was seen in the number of cases of meningococcal meningitis.
The marked decline in purulent meningitis from 2018 to 2019 was primarily caused by a drop in the number of notified cases caused by pneumococci, which declined from 77 cases in 2018 to 44 cases in 2019. This occurred following the 2014 to 2018 period when the number of notified cases of pneumococcal meningitis had increased steadily. Furthermore, the number of meningitis cases with “other streptococci” declined from 24 in 2018 to 11 in 2019.
As from 22 April 2020, vaccination with the 23-valent pneumococcal vaccine has been given free of charge to persons belonging to a number of defined risk groups, and as from 15 June 2020, a free pneumococcal vaccination offer has been in place for all persons aged 65 years or more. In 2019 and 2020 overall, a total of 43 of 88 cases of pneumococcal meningitis were caused by serotypes included in the 23-valent pneumococcal vaccine.
In 2019 and 2020 overall, one case of vaccine failure following pneumococcal vaccination was notified. The case occurred in a two-year-old child who had been fully vaccinated with Prevenar (13-valent) as part of the childhood vaccination programme, but who, nevertheless, was affected by a pneumococcal meningitis infection (serotype 19A).
The number of meningitis cases caused by Haemophilus influenzae remained stable at eight cases from 2018 to 2019, but declined to just three cases in 2020. Vaccination against H. influenzae serotype b (Hib) became part of the childhood vaccination programme in 1993. In 2019, two Hib cases were seen; both in patients aged less than one year. One of the children had been vaccinated in accordance with the Danish childhood vaccination programme with two of the three vaccinations containing the Hib component, of which the more recent one had been given four months prior to symptom onset. Therefore, this case was notified as vaccine failure. The other child had received its first Hib component vaccination only two days before symptom onset and was therefore not counted as vaccine failure. In 2020, one case of Hib meningitis was observed in a child aged one year, but the child was unvaccinated.
The number of deaths related to purulent meningitis is defined as the number of deaths within 30 days after the time of diagnosis. In 2019, a total of 18 deaths related to purulent meningitis were recorded, corresponding to a 17% mortality. In 2020, ten deaths were recorded, corresponding to a 14% mortality.
In 2021, a digital solution will be launched for notification of purulent meningitis and other notifiable diseases. This will be described in a later issue of EPI-NEWS.
(N.U. Friis, P. Valentiner-Branth, Department of Infectious Disease Epidemiology and Prevention, S. Hoffmann, H-C. Slotved, K. Fuursted, Department of Bacteria, Parasites & Fungi)