No 21-22 - 2017
Syphilis 2016
Syphilis 2016
|
In 2016, the national surveillance system, stewarded by Statens Serum Institut (SSI), recorded 742 cases of newly acquired syphilis in 720 persons.
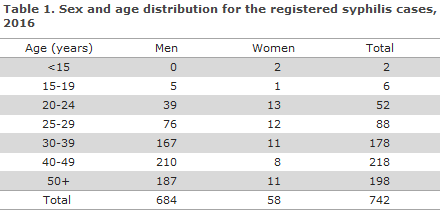
A total of 684 (92%) of the cases occurred in 664 men and 56 (8%) in 54 adult women, as 20 men and 2 women had 2 cases in the course of the year.
The median age was 42 years for men (range 17-85 years) and 31 years for women (range 18-78 years). Furthermore, two girls aged 0 and 6 years had syphilis, Table 1.
A total of 358 (48%) of the cases, 321 men, 36 women and one neonate, were reported to the Notification System for Infectious Diseases (NSID), the Department of Infectious Disease Epidemiology and Prevention (DIDEP).
The NSID received one notification for which the diagnosis was based on dark-field microscopy exclusively. A total of 384 (52%) cases had not been notified to the NSID. As in previous years, the majority of the patients resided in the Copenhagen area, Table 2.
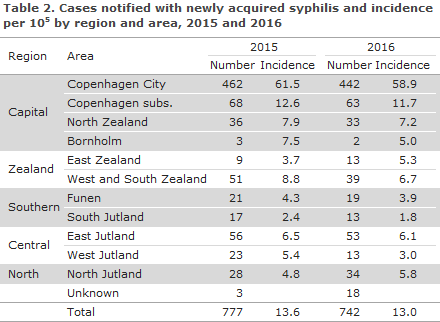
The total number of cases registered in 2016 remained largely in line with the preceding year (777), Table 2.
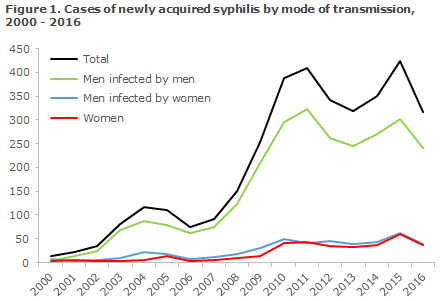
It seems, therefore, that the increase observed for a number of years has halted, Figure 1.
Congenital syphilis and syphilis in pregnant women
Among the 56 syphilis cases that were detected in women, 11 were found owing to the pregnancy screening. In one of these cases, no notification had been made to the NSID. Seven of the pregnant women were of Danish origin, one was from Greenland, and the remaining were from countries in Eastern Europe, Asia and Africa.
Additionally, one woman tested positive for syphilis in connection with the birth of her child. She had immigrated to Denmark a few days earlier and had therefore not participated in the screening. The new-born child had congenital syphilis. Furthermore, congenital syphilis was diagnosed in a 6-year-old child who was born in Denmark by an immigrant mother prior to the introduction of pregnancy screening for syphilis. The latter child was not notified with the NSID.
Transmission
Among the 357 notified adult cases, 321 were men (90% of those notified), including 56 who were notified as heterosexual transmission (17% of all notified men), 225 were notified as men who have sex with men (MSM, 70% of the notified men); and in 40 cases the mode of transmission was not stated (13% of the notified men). A total of 36 heterosexually infected women were notified (10% of all notified cases), including one who was notified as a bisexual. Figure 1 presents the number of persons notified with sexually transmitted syphilis since 2000.
Among the 337 cases in which origin was stated, 247 (73%) were of Danish origin, 79 (23%) were immigrants, 8 were second-generation immigrants and 3 were tourists. The number of persons who had not been born in Denmark totaled 82 from 37 countries around the globe.
The country of infection was stated for 305 (85%) of those who had been notified, 274 men and 31 women. A total of 214 (78%) men and 23 women (74%) had become infected in Denmark. In all, 21 (91%) of the women who had become infected in Denmark were of Danish origin. Among heterosexually infected men, 38 of 53 (72%) had become infected in Denmark, while this was the case for 167 of 206 (81%) of the MSM.
Syphilis and HIV
Information about HIV status was available for 295 (92%) men and 32 women (89%).
Among HIV-tested men, 94 (32%) were HIV positives. There were 84 HIV positives among the 223 MSM (38%), 2 (4%) among the 52 men who were notified as heterosexually infected and 8 (40%) among the 20 men for whom sexual orientation was not stated. Among the 94 HIV-positive men, 10 (11%) had been diagnosed with HIV and syphilis simultaneously (8 MSM and 1 heterosexual and 1 for whom the mode of transmission was not stated), whereas 84 (89%) were known HIV positives prior to their current syphilis diagnosis (76 MSM, 1 heterosexual and 7 cases for whom sexual orientation was not stated). No women were notified as being HIV positives.
Commentary
Syphilis has been nearly eradicated in Denmark, but as from the turn of the millennium an increase has been observed in the number of cases, an increase that was particularly pronounced in the 2006-2011 period. Following a decrease in the number of cases in 2012, syphilis cases followed an increasing trend, but now the number of cases has once again decreased. The decrease has been observed for both sexes and applies to both homosexually and heterosexually infected persons, but the occurrence of syphilis remains higher among MSM. The dramatic increase observed in the years from 2006 to 2011 has thus not continued.
Campaigns have been run to motivate more MSM to undergo frequent testing for sexually transmitted infections, including HIV, syphilis and gonorrhoea. The campaigns seem to have been successful with respect to syphilis as the described increase in syphilis - an infection that is more common among MSM - has not continued. Something similar was observed for gonorrhoea in 2016, EPI-NEWS 18/2017; the increase in the number of new gonorrhoea cases has continued, but to a much lesser degree among MSM than among heterosexually infected persons.
The typical chancre is symptom-free and furthermore often localised to places where it goes undetected by the patient. Interruption of chains of transmission can therefore not be based on symptom-triggered visits to the physician. Therefore, it is essential that MSM are tested frequently, even if they have no symptoms. This leads to the diagnosis and treatment of otherwise unacknowledged syphilis, whereby transmission chains can be broken.
All MSM are recommended annual testing for sexually transmittable infections including HIV; and MSM who lead an active sex life and who do not always use a condom are recommended testing 2-4 times annually. This test frequency is also recommended by the US Centers for Disease Control (CDC) and the National Health Service (NHS) in the UK.
The share of the notified syphilis patients (particularly MSM) who has been tested for HIV is very high. This is encouraging, and it is important that MSM who are tested for syphilis also undergo testing for HIV, EPI-NEWS 46/09, chlamydia, lymphogranuloma venereum (LGV) and gonorrhoea, cf. the Danish Health Authority’s guidelines on the Prevention, Diagnosis and Treatment of Sexually Transmittable Infections.
Since 1 January 2010, the general screening of pregnant women has included syphilis, EPI-NEWS 27-33/2010. In 2016, a total of 11 cases of syphilis were detected among pregnant women, including 7 Danish women. All 11 women were treated, and none transmitted syphilis to their child.
Two cases of congenital syphilis were found. In one case, the mother had tested positive for syphilis in connection with the birth of her child. She had immigrated to Denmark a few days earlier and had therefore not participated in the screening. The new-born child had congenital syphilis. The second case was a 6-year-old who was born in Denmark before the introduction of the general screening.
It is important that the screening of pregnant women continues and that the pregnant women who screen positive to syphilis undergo full serological testing to ensure that the diagnosis may be confirmed or dismissed within the time period in which treatment may prevent infection of the foetus, EPI-NEWS 35/15, i.e. so early that sufficient treatment may be concluded no later than 4 weeks before the pregnant women gives birth.
PCR testing is expedient for detection of Treponema pallidum in chancre material and is often positive before any antibodies can be detected.
Newly acquired syphilis, i.e. primary, secondary and latent syphilis, is notified to the Department of Infectious Disease Epidemiology and Prevention, SSI, on Form 1510.
As from July 2015, the full civil registration number (CPR) of the patient needs to be stated on the form, whereby monitoring is improved. The new form also includes the questions that were previously stated on a separate white form from the SSI's syphilis laboratory and which, among others, facilitate staging. The latter form is therefore no longer used, which facilitates the work of the notifying physicians.
(S. Cowan, M. Wessman, J. Kähler, Department of Infectious Epidemiology and Prevention, S. Hoffmann, Bacteria, Parasites & Fungi)
Link to previous issues of EPI-NEWS
31 May 2017