No 22 - 2016
HIV 2015
HIV 2015
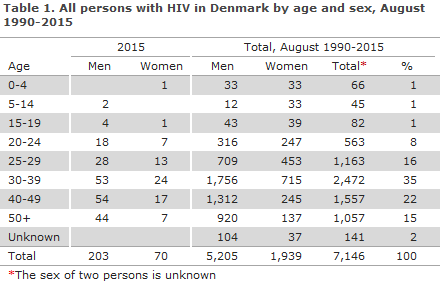
2015 saw a total of 273 notified cases of HIV, including 203 men and 70 women, Table 1. Among these cases, 65 had previously been diagnosed with HIV abroad, including seven Danish-born persons.
Among the 65 previously diagnosed persons (44 men and 21 women), 3 were cases of mother-to-child transmission (including one adopted child), 25 were homosexually infected (MSM), 30 were heterosexually infected (HTX), 2 were infected via intravenous drug use (people who inject drugs (PWID)), and in 5 cases the mode of infection was unknown or other. Of the 25 MSM with known HIV, 17 (68%) were from Europe or the US, whereas 25 out of 30 HTX (83%) were from Sub-Saharan Africa or Thailand.
The number of HIV positive immigrants who have been diagnosed before their arrival to Denmark is increasing; from 23 persons in 2010 to 65 in 2015, Figure 1. These persons thus contribute with an increasing number to the total number of persons who live with HIV (PLWH) in Denmark.
On the basis of models that are based on several data sources, it is estimated that PLWH comprised nearly 6,000 persons as per 31 December 2015, Box 1.
In the period from 2010 to 2015, a total of 236 previously diagnosed immigrants were notified with HIV in Denmark. Among these, there was information in 125 (53%) cases about current HIV treatment and/or CD4 counts that indicated that the patient was in treatment. This applied to 57 of 81 MSM (70%). The majority of the previously diagnosed cases thus represented no infectious potential.

Box 1. The estimated number of HIV positives in Denmark, the undiagnosed share and the number of cases who were tested late as per 31 December 2015
|
Newly diagnosed HIV positives in 2015: 208 The undiagnosed share (the dark figure): 600 |
Among the 208 (159 men and 49 women) who were diagnosed with HIV for the first time, a total of 104 (50%) were Danish-born (including one second-generation immigrant) and 104 (50%) were immigrants.
Among the 104 immigrants, three were notified as victims of human trafficking and/or undocumented migrants, and four were tourists. Apart from one person from Lithuania, the remaining six were all from Sub-Saharan Africa or from Thailand. All had AIDS or a very low CD4 count at the time of their diagnosis.
Among the remaining 97 immigrants, 34 (35%) were from Sub-Saharan Africa, 14 (14%) from Eastern Europe incl. Russia, 13 (13%) from Western Europe, 19 (20%) from South-east Asia (including Nepal), 9 (9%) from the Middle East and Northern Africa (including Turkey and Afghanistan), 5 (5%) from South America and 1 from Greenland, USA and Australia, respectively. Information was available about time of entry into Denmark for 63 out of 78 (81%) immigrants who were notified as having been infected prior to their arrival to Denmark.
Among these, 35 (56%) had stayed in Denmark for more than one year before they were diagnosed, particularly family reunified persons. Among six women from Thailand, five (83%) had stayed in Denmark for more than one year before being diagnosed.
A total of 101 were MSM, 93 HTX and 6 PWID. One case of mother-to-child-transmission was observed. In seven cases, the mode of infection was unknown.
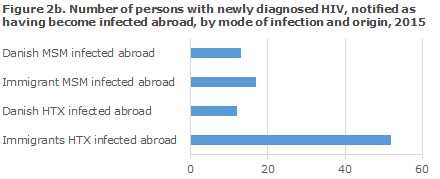
A total of 104 (50%) were infected in Denmark and 104 (50%) abroad. The median age was 39 years for men (range 5-77 years) and 35 years for women (range 21-75 years). The distribution on origin and mode of infection for persons notified as having been infected in Denmark and abroad, respectively, is presented in Figures 2a and 2b.
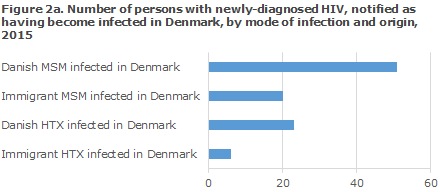
MSM infected in Denmark
A total of 51 Danish MSM were notified as having been infected in Denmark. For immigrant MSM, the corresponding number was 20. Among MSM-infected immigrants in Denmark, a total of seven were from Western Europe, four from South-East Asia, four from Eastern Europe and the remaining from various other parts of the world.
MSM infected abroad
A total of 13 Danish MSM were notified as having been infected abroad, including eight in Western Europe or the USA and three in South-East Asia. A total of 17 foreign MSM were notified as having been infected abroad. Five were from South-East Asia, four from Europe (two from Western Europe and another two from Eastern Europe) and three were from South America. The overwhelming majority had become infected in their country of origin.
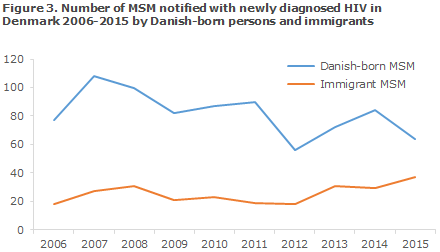
In the course of the past 10 years, the number of newly diagnosed, Danish-born MSM has decreased, whereas the number of newly diagnosed MSM born abroad has increased, Figure 3.
HTX infected in Denmark
A total of 23 Danes were notified as heterosexually infected in Denmark, including 15 men and 8 women. For the men, a known risk situation existed in seven (47%) of the cases (sex with sex workers or women from high-endemic areas). Among the women, a known risk existed in two (25%) cases (sex with an IV drug user and with a man from a high-endemic area). In the remaining cases, no known risk situation existed.
A total of six immigrants were notified as having been infected in Denmark, two men and four women. Only in two cases was a known risk described (sex with a person from a high-endemic area).
HTX infected abroad
A total of 12 Danes were notified as having been infected abroad, 11 men and one woman. Nine of the 11 men (82%) had become infected in South-East Asia (seven in Thailand and two in the Philippines).
A total of 52 immigrants, 18 men and 34 women, were notified as having been infected abroad. For all except five (10%), a known risk of infection existed. The majority, i.e. 32 (62%) were infected in Sub-Saharan Africa, whereas 11 (21%) were infected in Thailand. Among the women, 10 were detected thanks to the pregnancy screening, nine from Sub-Saharan Africa and one from Eastern Europe. Only three of the ten women who were diagnosed owing to the pregnancy screening and had entered Denmark in 2015.
PWID
Three Danish men were infected through IV drug use in Denmark. Three Eastern Europeans were infected in their countries of origin, including two men and one woman who was found in the pregnancy screening.
Perinatally infected persons
One immigrant child aged five years was notified. The child had become infected at birth in its country of origin.
Unknown mode of infection
Seven persons, two Danes and five immigrants, were notified with unknown mode of infection. This included one under-aged fugitive for whom infection due to dirty syringes in connection with torture was suspected.
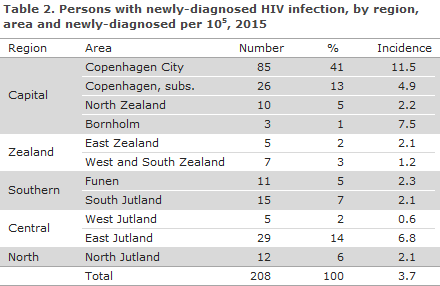
Table 2 shows the distribution by area and region. A total of 124 (60%) resided in the Capital Region of Denmark. The high incidence seen in 2015 on Bornholm does not reflect a chain of infection, but is simply a random geographical variation as they are not newly-infected persons.
CD4 count at diagnosis
Among 208 persons who were diagnosed with HIV for the first time, information on CD4 counts at their diagnosis and/or information about AIDS at their diagnosis was available for 196 persons (94%). In the remaining 12 cases, CD4 counts were unavailable.
The CD4 count is a marker that indicates how the HIV virus affects the cellular immune response. For a long period of time, a CD4 count below 350 cells per µl blood has been indication for initiation of highly active antiretroviral therapy (HAART) in Denmark if the patient had not wanted to initiate such treatment earlier. The guidelines have now been changed so that everyone who is diagnosed with HIV is offered to start treatment immediately, regardless of the CD4 count at the time of diagnosis. CD4 counts below 350 and/or AIDS at the time of diagnosis are still used in this report as markers for late testing.
Among the 196 cases for whom the CD4 count was stated, 103 (53%) had CD4 counts below 350 cells per µl at diagnosis, including eight persons assessed as newly infected based on primary HIV disease and/or a recent negative HIV test, whereas 93 (47%) had CD4 counts of 350 or above.
Among 98 MSM for whom the CD4 counts were stated, a total of 69 (70%) had a CD4 count > 349 or signs of new infection at the time of diagnosis, whereas this applied to 31 out of 88 (35%) HTX.
The time from infection to diagnosis was estimated on the basis of the information on CD4 counts at the time of diagnosis, previous negative tests and acute HIV disease. If information was available on acute HIV disease and/or a negative test within 1 year, the patient was assessed as having been "infected within 1 year"; if there was information on AIDS and/or a CD4 count below 200, the patient was assessed as "infected more than 8 years ago". If no information was available concerning a test within 1 year or about AIDS, and the patient's CD4 count was above 200, the person was assessed as having been "infected 1-8 years ago". A total of 103 of 104 Danish-born and 95 of 104 foreign-born persons had information on the notification that allowed for their placement into these categories, including 98 sexually infected Danish-born persons and 88 sexually infected persons born abroad, Figure 4.
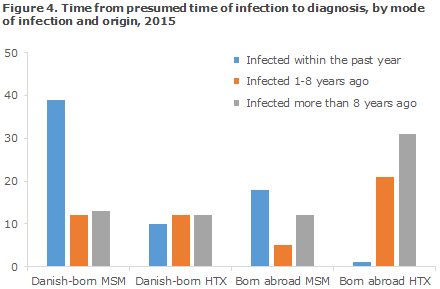
A clear trend was seen towards MSM being diagnosed early and HTX being diagnosed late. This trend was clearer for foreign-born HTX, among whom only 2% were assessed as having been infected less than 1 year before their time of diagnosis. For Danish-born HTX, this share was 29%, whereas it was 61% and 51% for Danish-born MSM and foreign-born MSM, respectively.
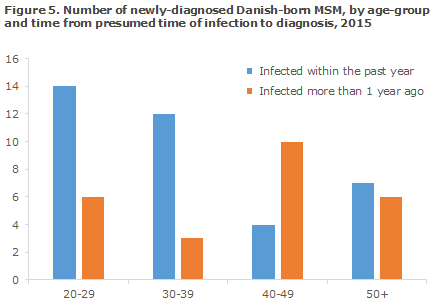
Furthermore, for Danish-born MSM, a substantial difference was seen with respect to time from infection to diagnosis depending on age, Figure 5, whereas this difference was not seen for foreign-born MSM.
AIDS
Among 208 newly-diagnosed persons, a total of 37 (18%) were diagnosed with an AIDS-defining condition concurrently with their HIV diagnosis, including 25 HTX, 10 MSM and 2 for whom the mode of infection remained unknown. Furthermore, six persons who had previously been diagnosed with HIV were now notified with AIDS. The period from HIV diagnosis to AIDS diagnosis lasted from 1 to 14 years. The most frequently seen AIDS-defining diagnoses were Pneumocystis carinii pneumonia (12 cases) and pulmonary tuberculosis (8 cases).
Checkpoint
The Checkpoint is the Danish AIDS Foundation's test sites for MSM and immigrants. Here, you can be tested for HIV and syphilis without scheduling an appointment and you will receive the results immediately. A total of 15 of the 208 newly diagnosed (7%) persons were tested at the Checkpoint, eight Danes and seven immigrants. All were MSM. One additional heterosexually infected woman from sub-Saharan Africa tested positive at the Checkpoint, but was not notified to the Department of Infectious Disease Epidemiology.
Transmitted resistance in persons with newly diagnosed HIV
The statement comprises all newly diagnosed HIV patients who are referred to a department of infectious diseases and have a genotypic resistance test performed within 1 year after diagnosis and prior to treatment initiation. Between 40% and 50% of the newly diagnosed HIV patients are every year enrolled in this study, corresponding to between 121 and 156 patients annually in the period. The shown data only include people notified as infected in Denmark and diagnosed with HIV in the year in question. From this subgroup, sequences were used from 79, 100 and 67 patients who were newly diagnosed in 2013, 2014 and 2015, respectively.
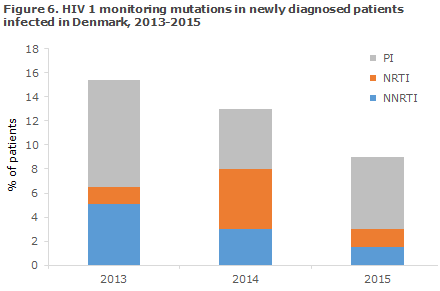
In 2015, the Section for Virology Surveillance and Research diagnosed a total of six new cases of transmitted HIV resistance monitoring mutations, corresponding to 9% of all the tested newly diagnosed HIV patients infected in Denmark. The prevalence of resistance monitoring mutations has thus decreased in the period from 2013-2014 to 2015, Figure 6. All of the samples tested were HIV-1.
In 2015, the resistance monitoring mutations were distributed on all of the three primary antiretroviral (ARV) therapy groups used for highly active anti-retroviral therapy (HAART): non-nucleoside inhibitors (NNRTI), one patient, nucleoside inhibitors (NRTI) one patient, and protease inhibitors (PI) four patients.
No patients were resistant to more than one treatment group, and all were therefore susceptible to a minimum of two ARV treatment groups. The 2013-2015 period recorded a total of 30 patients with resistance. A total of 28 of these were of subtype B, one was of subtype A and one was CRF01_AE. The period has not seen any changes in the molecular diagnosis or sequencing analysis that may explain the decrease in the prevalence of resistance monitoring mutations, which is therefore presumably owed to a decrease in infection from patients with resistant HIV.
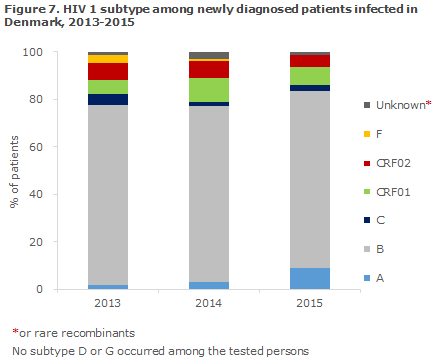
HIV subtypes among newly-diagnosed patients infected in Denmark
Among newly diagnosed HIV 1 patients who have been infected in Denmark, HIV 1 of subtype B comprised 75% in 2015, Figure 7. Subtypes A, B and C and the two recombinant forms CRF01_AE and CRF02_AG were seen every year in 2013, 2014 and 2015 with an average prevalence of: 9% for A, 75% for B, 3% for C, 8% for CRF01_AE and 5% for CRF02_AG. These subtypes and recombinants are also among the most frequently observed in the remaining European countries.
Commentary
The number of notified HIV cases in 2015 was in line with the numbers recorded in the previous years, and MSM and immigrants who were HTX-infected with HIV before their arrival in Denmark remained the main infection groups.
This year, the HIV report presents both persons who have received the HIV diagnosis for the first time and those who have previously been diagnosed abroad, but who test positive for the first time in Denmark. The majority of data in the report concern the first group only; and only the numbers pertaining to this group are passed on to the international HIV monitoring initiative.
Otherwise, the previously diagnosed persons would be counted more than once in the international statistics thereby producing an incorrectly high total number of new HIV diagnoses. The number of newly-diagnosed persons has remained relatively constant for a considerable number of years, and those previously diagnosed abroad therefore comprise an increasing share of the persons who live with HIV (PLWH) in Denmark. They are therefore described in detail in the introduction to the report. It is worth noting that MSM and HTX-infected persons contribute with about the same number to this group, but more MSM infected persons are in treatment when they arrive to Denmark.
Among the MSM who were newly diagnosed, foreign-born MSM comprised an ever increasing share. This should be considered when planning future HIV prevention, particularly in relation to the opportunity for providing easily accessible HIV testing of foreign MSM who may not be aware of the opportunities afforded by Danish healthcare, including the free-for-all HIV test.
The Checkpoint continues to account for a considerable share of the notified persons, and it may be expected that the HIV diagnosis will in future be made more often as a rapid test that provides a result immediately. These tests are not recorded by laboratories and therefore do not form part of the national monitoring of laboratory results.
Rapid tests are used at the Checkpoint and also at some hospital departments, e.g. at maternity wards. Here, women are tested who belong to risk groups but have not been tested in the general pregnancy screening as they arrive only shortly before giving birth. In this case, the rapid test is decisive in ensuring the necessary treatment of the woman in labour and her neonate as there is no time to wait for a result from the hospital’s laboratory.
Furthermore, it may be expected that home-testing will become increasingly normal, either as a public offer or as home tests bought on the internet. It is important that the date of any positive rapid test is stated on the HIV notification. In this manner only will it be possible to monitor the time that passes from the patient learns of his or her positive HIV status and until the final diagnosis is made at an infectious medicine clinic. This interval bears testimony to the efficiency of the healthcare system in ensuring that those infected with HIV are diagnosed as rapidly as possible, and then affiliated with an infectious medicine department so that they can start receiving effective treatment without delay. Treatment is initiated rapidly to achieve the best possible prognosis for the patient and because a well-treated HIV positive person cannot pass on the infection to others. In August 2015, the Danish Society for Infectious Disease updated its guidelines and started recommending antiretroviral treatment for all HIV infectees regardless of their CD4 counts at the time of diagnosis.
The share of MSM who was diagnosed as newly infected cases continues to increase, indicating that the message concerning frequent testing has gained foothold. Additionally, it is a symptom of considerable and continued spreading of the infection, which it has not been possible to contain through the prophylactic strategies presently in use. Both the European Centre for Disease Prevention (ECDC), the WHO and the UNAIDS recommend medical prevention of HIV, so-called pre-exposure prophylaxis (PrEP) for persons who are at a special risk of becoming infected with HIV. Several scientific studies have shown that countries with an HIV epidemic that is focused on MSM who have in place a good treatment strategy - such as Denmark - will be able to break the HIV curve among MSM by introducing PrEP. Several countries, including France, have recently started offering PrEP to MSM who are at a high risk of HIV infection, and it is expected that it will also become possible to treat HIV with PrEP in Denmark at some point in time.
Among Danish-born MSM who are diagnosed with HIV when they are more than 40 years old, the share of patients who are tested late is considerably higher than among younger patients. Focussing on having younger MSM undergo HIV testing regularly is therefore insufficient; elderly MSM should also undergo testing. The same trend is not observed among foreign-born MSM who were newly diagnosed with HIV in Denmark. In this group, both the young and the elderly were typically diagnosed shortly after the presumed time of infection. All sexually active MSM should be tested for syphilis, gonorrhoea and chlamydia at least once annually. MSM who practice anal intercourse without a condom should be tested more frequently for HIV, e.g. once a month. The Danish Health Authority's guidelines on which persons should be tested for HIV are described in EPI-NEWS 46/09.
Among the newly diagnosed HIV positives who had been infected in Denmark, 9% of the tested positives had transmitted resistance (TR) to 1 of the 3 primary ARV treatment groups that are used for highly active antiretroviral therapy (HAART). None had resistance against several ARV treatment groups, and they therefore posed no particular problem in relation to effective treatment. It is important to keep monitoring TR in Denmark as it may be expected that some MSM will obtain PrEP via the internet before it becomes a public prophylactic offer - without undergoing the prophylactic tests that should precede PrEP. They will therefore risk taking it even though they are already HIV positive, whereby the risk of developing resistance and of spreading of resistance increase.
More than half of the HIV-positive immigrants who were infected before entering Denmark had stayed in Denmark for more than a year before being diagnosed. Particularly women from Thailand who presumably entered Denmark through family unification and were therefore not offered a health check at their arrival in Denmark had stayed in Denmark longer than average before being diagnosed. According to the Danish Health Authority's guidelines on HIV testing, it is recommended that immigrants from areas where HIV occurs endemically undergo a HIV test when arriving to Denmark.
AIDS is no longer considered a separate condition, but is treated as part of the HIV disease, EPI-NEWS 37/14. That 37 (18%) also had an AIDS-defining diagnosis when they were diagnosed with HIV is thus a reflection of late testing.
The situation for those persons who were previously diagnosed with HIV and who presented with an AIDS-defining condition in 2015 is substantially different. Today, the opportunities for medical HIV treatment are so good that it should largely be possible to prevent AIDS. When AIDS is, nevertheless, still being reported among previous HIV infectees, this is generally due to lacking treatment compliance. The very low number (six persons in 2015) is indicative of an extremely successful treatment of HIV-positives in Denmark.
The efforts made to collect and update epidemiological information is carried out regularly between the EPI-NEWS reports; and minor changes to previous data may therefore occur as our knowledge improves. At the web site of Statens Serum Institut you will find continuously updated data including any received notifications of HIV and other conditions.
(A.H. Christiansen, S. Cowan, Department of Infectious Disease Epidemiology, J. Fonager, Virology Surveillance and Research)
Link to previous issues of EPI-NEWS
1. June 2016