No 36/37 - 2025
Syphilis 2024
Syphilis 2024
- In 2024, 628 syphilis cases were reported to Statens Serum Institut (SSI), 62% of which were among men who have sex with men (MSM).
- The increase in syphilis among MSM from 2019–2022 was followed by a small decline from 2023–2024. From 2022 to 2023 there was a slight increase in heterosexual transmission. This increase has continued among women who have sex with men, while it has leveled off among men who have sex with women.
- The vast majority of syphilis cases, among both men and women, were infected in Denmark (95%). The most common countries of infection after Denmark were Germany, Spain, and Greenland.
- Information about HIV status was available for 90% of reported syphilis cases in 2024. In total, 95 of those reported also had HIV. Most were already known to be HIV-positive, but two MSM, as well as one man and one woman infected heterosexually, were newly diagnosed with HIV.
- Syphilis occurred most frequently among people aged 30–59 years; the median age was 40.5 years for men and 35 years for women.
- In 2024, 15 women had confirmed syphilis detected in pregnancy screening, eight of whom were born in Denmark and seven born outside Denmark.
- One case of congenital syphilis was reported in 2024.
- Frequent testing of relevant risk groups can help break chains of transmission and thereby contribute to reducing the number of syphilis cases.
In 2024, 628 cases of syphilis were reported to the Department of Infectious Disease Epidemiology and Prevention at Statens Serum Institut (SSI), see Figure 1. The 628 cases involved 615 individuals, as 12 of these were reported with more than one occurence during the year.
For a detailed epidemiological description of the 2024 occurrence, please refer to the 2024 annual syphilis report .
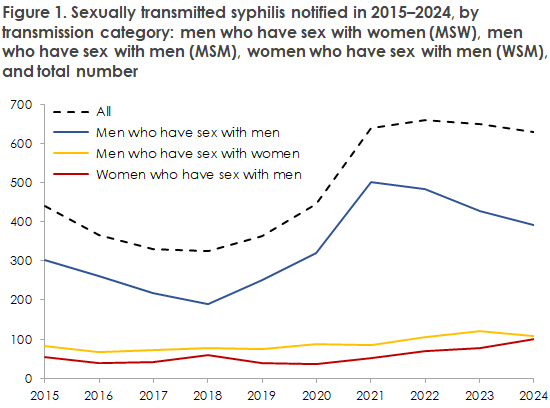
From 2022 to 2023, there was a small but concerning increase among heterosexuals, indicating that syphilis is establishing itself in the general population. This increase continued in 2024 among women who have sex with men, while it has levelled off among men who have sex with women. It continues to be important for physicians to consider syphilis as a possible differential diagnosis, also in heterosexual patients.
It is essential for us in Denmark to maintain screening during pregnancy so we can prevent an increase in congenital syphilis. Among the 102 reported syphilis cases found in women in 2024, 15 (15%) were identified through pregnancy screening; eight of these women were born in Denmark and seven were born abroad. Syphilis in a pregnant woman can have potentially serious consequences for the child.
In 2024, one case of congenital syphilis was reported. An ethnically Danish woman, pregnant for the second time with a previously uncomplicated pregnancy and birth, presented at the maternity ward at 37+2 weeks’ gestation because of reduced fetal movements for one day. She was diagnosed with intrauterine fetal death (IUFD). Early ultrasounds in the first and second trimesters were normal, as were growth scans at 30 and 35 weeks. The woman had been, as is recommended during pregnancy, screened for HIV, hepatitis, and syphilis in the first trimester, with negative results.
Ten days before admission, the screening was repeated by chance. The new screening test was positive for syphilis less than 24 hours before the IUFD was diagnosed. A confirmatory syphilis test showed active infection. For further information on this case, see the article in Ugeskrift for Læger . This case underscores the importance of pregnancy screening in identifying infections and enabling timely treatment. It also highlights the need to continuously ask about risk behavior throughout pregnancy in order to identify late infections and prevent transmission to the child.
In 95 cases, the person reported with syphilis also had HIV; 91 were known HIV-positive and four were newly diagnosed. Of the newly diagnosed, two were MSM, and one man and one woman were infected heterosexually. While there is already a strong focus on HIV testing among MSM with sexually transmitted infections, including syphilis, it is important also to remember testing for HIV when exposure is relevant among heterosexuals, transgender people, and sex workers.
Of the 469 HIV-negative syphilis cases, 126 were reported to be on PrEP (pre-exposure prophylaxis), the majority of which were MSM. It is encouraging that MSM are being offered appropriate PrEP, as this prevention method has proven to be a highly effective tool in reducing HIV in this group. It therefore remains important that healthcare personnel remember to offer PrEP when they encounter individuals in the target group.
According to the Executive Order on Notification of Infectious Diseases (BEK 865 of 20/06/2025), all stages of syphilis must now be reported via the Danish Health Data Authority’s Electronic Notification System (SEI2).
(L.H. Holm, S. Voss, M. Wessman, Department of Infectious Disease Epidemiology and Prevention)