No 51 - 2024
Mycoplasma genitalium in Denmark, 2011 – 2023
Mycoplasma genitalium in Denmark, 2011 – 2023
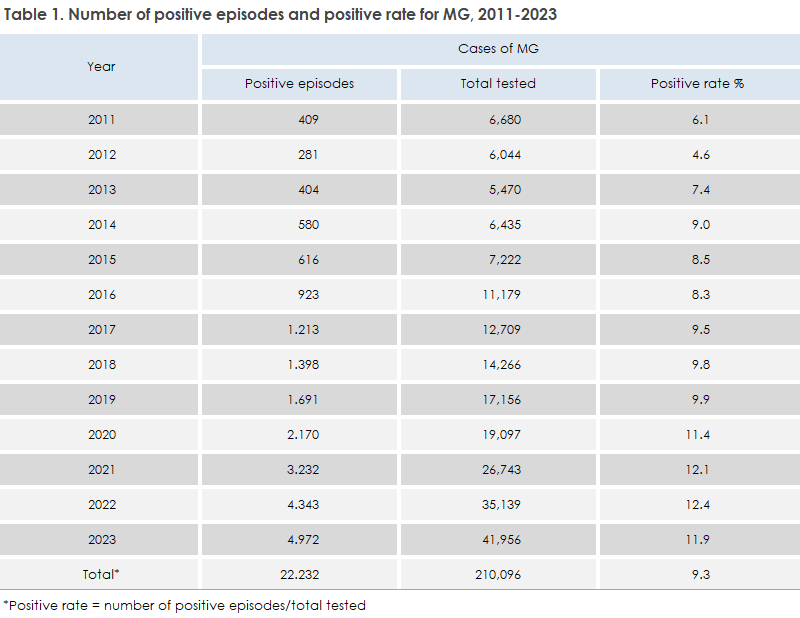
Mycoplasma genitalium (MG) is a sexually transmitted infection that can cause urethritis, cervicitis, and pelvic inflammatory disease. The infection is detected exclusively through molecular methods (nucleic acid amplification tests, NAAT). Below is a description of the prevalence and antibiotic resistance of MG in Denmark from 2011 to 2023, with a special focus on 2023, based on data collected from the Danish microbiology database, MiBa. Since October 27, 2023, MG has had the same status as chlamydia in the form of laboratory-based notification and surveillance, and the number of episodes is defined by the first positive test result within a 42-day period.
For a more detailed description, refer to Mycoplasma genitalium – Report of prevalence and antibiotic resistance, 2011 – 2023.
Data on quinolone resistance is based on a subset of samples submitted for MG analysis. This report includes samples from January 2018 to December 2023, though with a maximum of 200 samples per year, and builds on the MG overview published in 2023.
In 2023, 41,956 episodes were investigated, and MG was found in 4,972 cases (11.9%), distributed across 1,995 men (positive rate 16.4%) and 2,977 women (positive rate 10%). Overall, the MG positive rate has increased from 6.1% in 2011 to 11.9% in 2023, Table 1. Among men and women, the highest positive rates are observed in the 20-24 age group of 22.8% for men and 14.9% for women in 2023, whereas the highest positive rate for chlamydia is seen in the 15-19 age group. In 2023, the highest incidence was observed among 22-year-old women (754 cases per 100,000) and 25-year-old men (406 cases per 100,000). Compared to chlamydia in 2023, the highest incidence was in 19-year-old women and 21-year-old men. The majority of cases (75% in 2023) were recorded in the 15-29 age group.
The largest number of individuals tested came from Copenhagen city and surrounding suburbs, for both men (test incidence per 100,000 inhabitants 1,575 and 509) and women (3,646 and 1,439, respectively). There has been a significant increase in the number of tests and incidence since 2011, across the country. In contrast, the incidence of laboratory-confirmed chlamydia cases has decreased for both men and women from 2022 to 2023 nationwide (Chlamydia - Report of disease prevalence 2023).
The Danish treatment recommendation is based on the European guidelines from IUSTI (International Union against Sexually Transmitted Infections) supported by WHO and ECDC. Resistance to macrolide and quinolone antibiotics complicate treatment, and the guidelines recommend that treatment of MG infections always be preceded by macrolide resistance testing. Quinolone resistance testing is not performed unless treatment with moxifloxacin has failed, and quinolone resistance testing is currently only conducted at SSI.
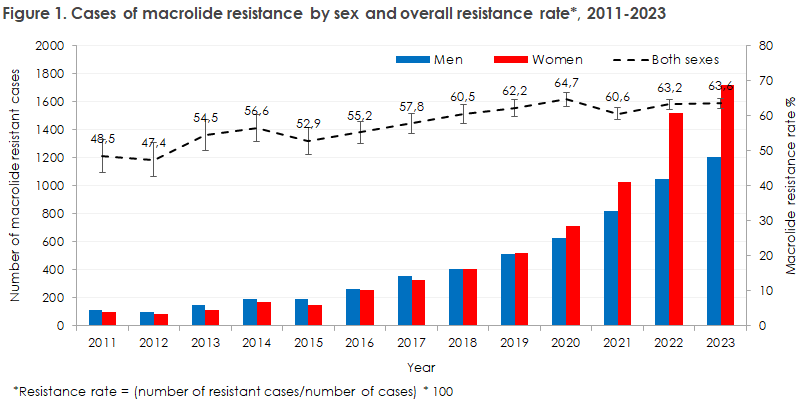
Between 2011 and 2023, there has been a significant increase in the macrolide resistance rate regardless of sex, from 40% to approximately 63%, Figure 1. The highest rates have been observed in the 15-24 age group for both sexes and rates of up to 70% have been recorded in both sexes in East Jutland and Funen. Between 2018 and 2023, quinolone resistance-associated mutations (QRAM) were detected through sample-based testing in 1,651 MG-positive patients. In 2023, 347 samples were tested, of which 22 had QRAM (6.3%). The quinolone resistance rate was slightly higher among men (7.7%) than women (5.2%) in 2023, and higher than in previous years. In 2023, a dual resistance rate of 5.2% was observed.
Testing activity for MG has increased over the years, and this report is the first attempt to compile national figures. It is noteworthy that there are significant regional differences in test incidence. It appears that in some areas, testing for MG is conducted without clinical symptoms, which goes against recommendations. The positive rate has been increasing and is now almost at the same level as for chlamydia. A similar upward trend is seen in resistance to macrolides. Data from the Prescription Registry indicate that the use of azithromycin for treating chlamydia has decreased but still accounts for about half of treatments. Usage should be further reduced. The prevalence of resistance to quinolones is still limited in Denmark, but when over half of the diagnosed cases already have macrolide resistance, a large number of patients will be treated with moxifloxacin, and treatment failures will occur. These patients cannot be treated with drugs registered in Denmark and must therefore be referred to sexual health clinics with special permits to dispense pristinamycin or other third-line treatments. Export restrictions on pristinamycin have been introduced, which has resulted in some patients with dual resistance being untreatable, emphasizing that testing for MG should only be conducted when symptoms are present.
(S. Tulsiani Drud, T. Roland Pedersen, J. Skov Jensen, Section for Reproductive Microbiology, Department of Bacteria, Parasites, and Fungi)