No 48 - 2024
World AIDS Day
HIV 2023
World AIDS Day
December 1st is World AIDS Day (WAD). One of the biggest obstacles to achieving the global goals is the lack of adherence to human rights, which is this year’s theme for WAD. By focusing on human rights, there is hope that the world can end AIDS as a public health threat by 2030.
Although the number of new HIV cases has fallen globally by 39% since 2010, three regions are experiencing an increase in new HIV infections: Eastern Europe, Latin America, and the Middle East/North Africa.
As the proportion of late testers in Denmark remains high, it is important to remember to test the population groups where human rights, or the lack thereof, still play a significant role and can pose barriers to testing.
HIV 2023
In 2023, 110 people were reported with newly diagnosed HIV, as well as 117 people who were already diagnosed abroad. As in 2022, a high number of refugees from Ukraine were reported with HIV in 2023. 56 HIV-positive Ukrainians were reported, of which 45 were known and in treatment from their home country. The remaining 11 were diagnosed with HIV for the first time in Denmark.
For a detailed epidemiological description of the incidence in 2023, please refer to the annual report on HIV 2023.
- Among the newly diagnosed, 60 were either Danes infected in Denmark or abroad, or immigrants infected after arriving in Denmark. The remaining 50 were immigrants infected before arriving in Denmark. These 50 could not have been reached by Danish HIV prevention measures.
- Among the newly diagnosed, there were 39 men who have sex with men (MSM) and 56 heterosexually infected (HTX), of which 28 were men and 28 were women (including two trans women). The remaining 15 were reported with another (6) or unknown mode of transmission (9).
- 46% of MSM and 33% of HTX were infected in Denmark.
- Among newly diagnosed MSM, 64% were immigrants. The proportion was 63% for HTX.
- Among MSM, 41% were late testers. The same applied to 66% of HTX.
- Immigrants, asylum seekers, etc., should be tested for HIV as soon as possible after arriving in Denmark. This allows for rapid treatment of HIV-positive individuals and reduces the risk of further transmission.
- All MSM who do not have known HIV should be tested for HIV once a year. Additionally, MSM who have an active sex life and do not consistently use condoms should be tested for HIV and other sexually transmitted infections more frequently, e.g., every 3 months, and possibly offered PrEP (Pre-Exposure Prophylaxis, HIV medication taken before exposure). PrEP has been proven to provide the best prevention against HIV and can be credited for the significantly declining incidence of HIV among MSM in Denmark.
- Immediate treatment after diagnosis ensures that people who are known to be HIV-positive do not pose any risk of further transmission of HIV, as well-treated HIV-positive individuals cannot transmit the virus.
- HIV prevention includes:
o Condom use
o TasP (Treatment as Prevention, i.e., only unprotected sex with HIV-positive individuals known to be in effective treatment).
o PrEP (Pre-Exposure Prophylaxis, HIV medication taken before exposure).
o PEP (Post-Exposure Prophylaxis, HIV medication taken immediately after exposure).- The prevalence of HIV resistance has not changed significantly in recent years. Resistance to non-nucleoside inhibitors (NNRTI resistance) is by far the most common.
- None of the 130 patients who were tested for resistance had a resistance score ≥15 against both emtricitabine (FTC) and tenofovir (TDF), the two nucleoside inhibitors (NRTI) that make up PrEP (Truvada®).
Decrease in the number of infected in Denmark, but no decrease in the total number of reported HIV cases
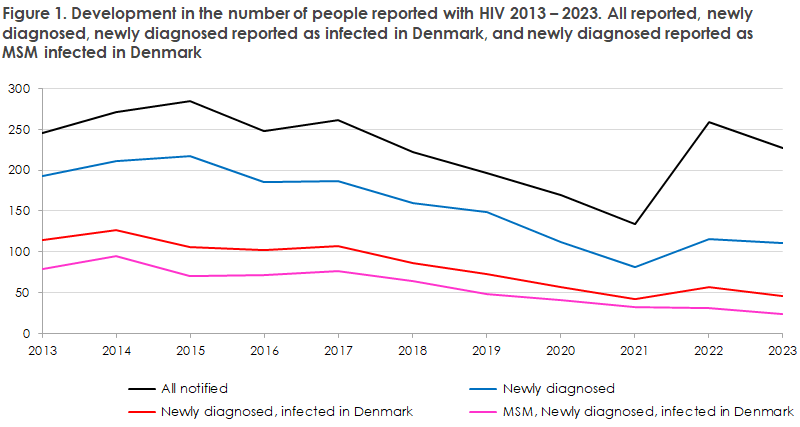
Since 2017, there has been a sharp decline in the number of HIV cases reported as infected in Denmark, especially among MSM, Figure 1. This decline coincides with the introduction of PrEP (Pre-Exposure Prophylaxis, HIV medication given preventively to prevent HIV infection) and has continued since 2017.
The increase in the number of reported cases observed in 2022 was primarily due to the large contingent of Ukrainian refugees that Denmark has received, some of whom are HIV patients. There were still a number of Ukrainian HIV-positive individuals reported in Denmark in 2023, most of whom were previously tested in their home country and therefore do not fall under the “newly diagnosed” group, which is why the two top lines are not parallel.
Among report cases were 39 MSM, 28 men who have sex with women (MSW), 30 women who have sex with men (including two trans women (WSM)), four people with other reported modes of transmission, and nine reported with unknown transmission route.
Of the 39 MSM, 13 (33%) were born in Denmark and infected in Denmark, 12 (31%) were born abroad and infected after arriving in Denmark, while one (2%) was born in Denmark and infected abroad. These 26 represent the number of MSM for whom prevention efforts in Denmark have not been effective (67%). The remaining 13 (33%) were born abroad and infected before arriving in Denmark. The 39 newly diagnosed MSM, as well as the 14 Danish-born MSM, are the lowest numbers of MSM recorded since HIV surveillance began in 1990.
CD4 Count at Diagnosis – Late Testers
The proportion of late testers was 56% in 2023, slightly down from 2022, when it was 60% (the proportion was between 47% and 55% in 2018-2021).
There is a significant difference in the proportion of late testers depending on the mode of transmission and origin. Among all MSM, the proportion of late testers was 41% (16 out of 39). Among MSM born abroad, the proportion of late testers was 35% in 2023, while it was 54% for MSM born in Denmark. This is the first time that MSM born in Denmark have a higher proportion of late testers than MSM born abroad. This can be explained by the fact that MSM who are not on PrEP treatment in Denmark belong to a less resourceful and/or less self-aware group that, in addition to not receiving PrEP, does not follow the advice to get tested for HIV every year. Thus, fewer and fewer Danish MSM are being diagnosed with HIV, but they are being diagnosed later.
Prevention Potentials
Over the years, the number of new HIV diagnoses in Denmark has decreased. Contributing factors include frequent testing, especially among MSM, early treatment initiation (TasP, Treatment as Prevention), which prevents treated HIV-positive individuals from transmitting the virus, and especially PrEP (Pre-Exposure Prophylaxis, HIV medication taken before exposure, offered to MSM).
To further prevent HIV transmission among MSM, it is important that the doctor who finds an MSM positive for gonorrhea, syphilis, or chlamydia/LGV tests them for HIV and, if they are HIV-negative, offers the patient PrEP. The Danish Health Authority updated the specialty plan for infectious disease medicine in 2024, so PrEP can now be dispensed at the main function level . For some MSM, there may be a barrier to taking the initiative to seek PrEP treatment, so doctors can advantageously suggest this.
Likewise, being bisexual may negatively influence the patient’s initiative to seek both HIV testing and PrEP treatment, which staff at testing sites should also be aware of.
Regarding heterosexually transmitted HIV, it is especially important to test immigrants from countries with a high prevalence of HIV quickly after arrival. The Danish Health Authority’s 2013 guidelines state that people from Africa, Asia, South America, and Eastern Europe should be considered for HIV testing at the first contact with the healthcare system, regardless of the reason for the contact.
It can be difficult to identify people at risk of HIV infection among Danish-born heterosexuals. However, there are some possibilities for preventing infection in this group. These may include individuals who go on “sex holidays” to the East or Africa, or people who frequent swinger clubs. Additionally, in 2023, there was a relatively large proportion of reported HTX-infected individuals with information about homelessness, prostitution, etc. Thus, HIV has increasingly become a disease with a social bias, whereas in Denmark it was previously a disease most often diagnosed among resourceful, self-aware MSM.
To prevent further transmission from individuals with undiagnosed HIV, doctors should also be aware of patients with so-called signal diseases/indicator diseases, such as hepatitis (A, B, C), anal cancer, etc.
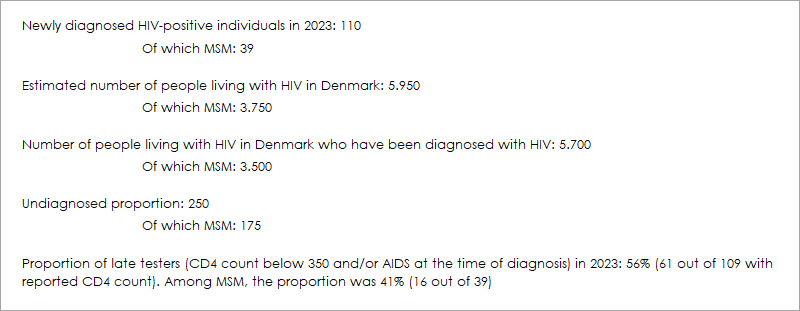
Box 1. The estimated number of HIV-positive individuals in Denmark, the undiagnosed proportion, and the number of late testers as of December 31, 2023
The figures have been underestimated compared to previous estimates, and the following is partly made using the ECDC’s model for incidence calculations, which has a large confidence interval, and partly using data from the Danish HIV Cohort (DHK). The adjustment is within the framework of the ECDC model but now aligns more closely with the actual figures from DHK.
(S. Cowan, C. Eves, M. Wessman, Department of Infectious Disease Epidemiology and Prevention, J. Fonager, M. Bennedbæk, R. Datcu, Department of Virus and Microbiological Special Diagnostics).