No 46 - 2024
DANMAP 2023
DANMAP 2023
The DANMAP program monitors antibiotic consumption and resistance in bacteria from humans, animals, and food in Denmark. The DANMAP collaboration has existed since 1995 and publishes annual reports describing the most significant findings regarding antibiotic use and the occurrence of antibiotic resistance.
Below are the key findings from 2023.
Antibiotics for Humans
In 2023, total human antibiotic consumption was 16.54 Defined Daily Doses per 1,000 inhabitants per day (DID), which is 6.6% higher than in 2022 (EPI-NEWS 44a/2024) and 6.3% lower than 10 years ago (17.64 DID in 2014). Thus, antibiotic consumption in 2023 was higher than in 2019 (15.77 DID), before the COVID-19 pandemic.
Antibiotics for Children
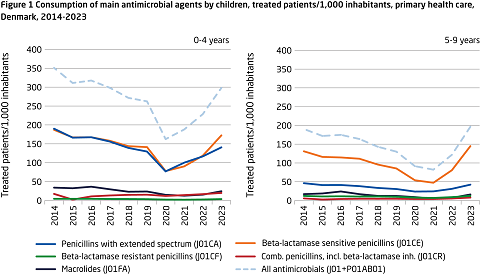
In primary care, antibiotic consumption was 14.56 DID, with penicillins accounting for 67%. The use of antibiotics for children in primary care has increased significantly since 2021. Among the youngest children (aged 0–4 years), 298 patients per 1,000 inhabitants was treated with antibiotics, 13.6% higher than in 2019 (262.4 patients per 1,000 inhabitants). Among older children (aged 5–9 years), consumption increased by 51% over the same period, from 130 to 197 patients per 1,000 inhabitants in 2019 and 2023, respectively (Figure 1).
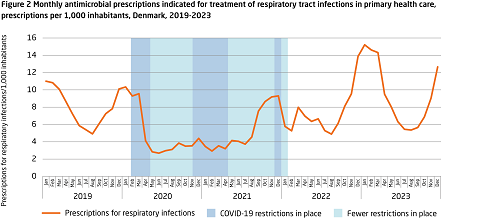
In the winter of 2022–2023, the usual seasonal peak in antibiotic use reached a higher level than observed in 2018–2019. This was likely due to an early RSV epidemic, the flu season, and an outbreak of Group A Streptococcus infections (Figure 2). These infections can lead to secondary bacterial infections requiring antibiotic treatment, thereby increasing antibiotic consumption.
Antibiotics for the Elderly
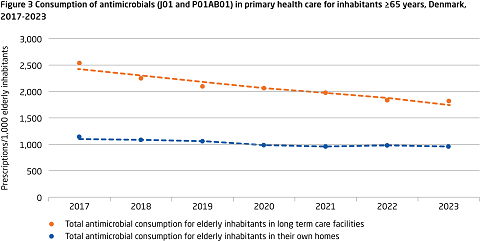
Antibiotic use among elderly individuals in nursing homes was 90% higher than among elderly individuals living at home. The most significant difference was seen in antibiotics used to treat urinary tract infections. This difference persisted despite a 28% reduction in antibiotic use in nursing homes between 2017 and 2023, from 2,540 prescriptions per 1,000 inhabitants to 1,819 prescriptions per 1,000 inhabitants. Over the same period, antibiotic use among elderly individuals living at home decreased by 16%, from 1,144 prescriptions per 1,000 inhabitants to 957 prescriptions per 1,000 inhabitants.
Antibiotics for Hospital Patients
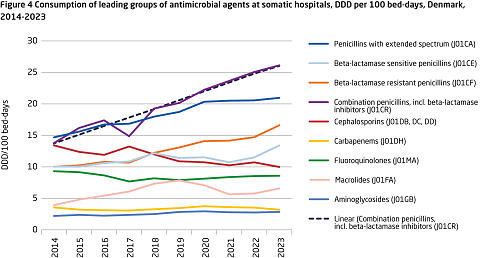
The trend in antibiotic consumption in hospitals depends on the measurement unit used. Unlike primary care, hospital antibiotic consumption increased over the past decade, from 99.40 to 135.66 DDD/100 bed-days and from 502.6 to 569.02 DDD/100 admissions. Measured in DDD/1,000 inhabitants/day, hospital consumption showed less pronounced changes in 2023 compared to ten years ago.
The observed increase in DDD/100 bed-days was driven by a rising use of penicillins combined with beta-lactamase inhibitors (90% increase from 2014 to 2023) and beta-lactamase-resistant penicillins (66% increase). During the same period, the use of critically important antibiotics (cephalosporins, fluoroquinolones, and carbapenems) decreased by 17% (Figure 4).
Antibiotic Shortages
The supply of antibiotics is increasingly challenged by delivery difficulties. In 2022, penicillin/beta-lactamase inhibitors were unavailable in July and August due to supply issues. Approximately 70,000 DDD of penicillin/beta-lactamase inhibitors were imported under special authorization from the Danish Medicines Agency to meet hospital needs (compared to 4,000 DDD imported in 2019–2021).
In 2023, nitrofurantoin faced prolonged supply challenges, and despite importation under special authorization, the total demand could not be met. Consequently, the use of other antibiotics for treating urinary tract infections increased during this period.
Antibiotic Resistance in Clinical Bacteria from Humans
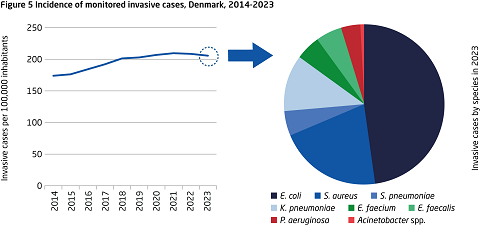
The incidence of invasive bacterial infections in Denmark reached 12,205 cases for monitored species in 2023 (Figure 5). The incidence has been rising for many years but appears to have stabilized since 2021. Compared to ten years ago, the number of invasive bacterial infections has increased by 25% (9,790 cases in 2014). Escherichia coli remained the most frequent cause of invasive infections (50% of all cases) in 2023, followed by Staphylococcus aureus and Klebsiella pneumoniae.
Vaccination efforts have reduced the incidence of invasive Streptococcus pneumoniae infections (709 cases in 2014, 602 cases in 2023), with significant declines in 2020 and 2021 (363 and 333 total cases, respectively) during the COVID-19 pandemic. Since then, incidence has risen again during the winter of 2022–2023.
Following a decline in resistance rates for many monitored bacterial species during the COVID-19 pandemic, resistance rates have stabilized or increased since 2022, albeit remaining at a low level.
It remains crucial to focus on reducing antibiotic consumption and prescribing narrow-spectrum antibiotics whenever possible.
After a significant decline in cases of ESBL- and pAmpC-producing E. coli bloodstream infections from 2020 to 2021 (352 and 254 cases, respectively), the number rose to 346 in 2023, similar to 2022 levels (336 cases). Compared to 2021, incidence increased by 36%. CTX-M-15 remained the most frequent ESBL enzyme, present in 57% of cases. Monitoring these E. coli strains is essential, as ESBL- and/or AmpC-positive bacteria are resistant to most beta-lactam antibiotics.
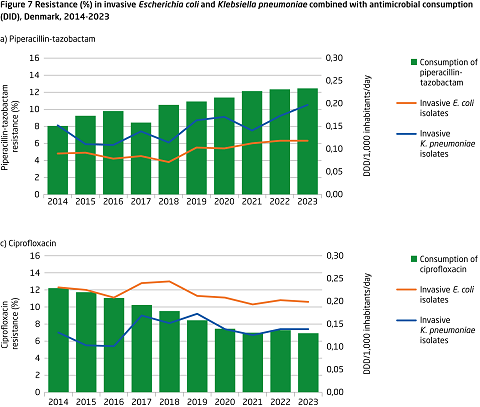
Resistance to piperacillin-tazobactam in K. pneumoniae has increased over the past decade, exceeding 10% in both invasive infections (8.1% in 2014, 10.5% in 2023) and urinary tract infections (6.0% in 2014, 10.5% in 2023) among hospitalized patients.
Combined resistance to 3rd-generation cephalosporins, ciprofloxacin, and gentamicin remained low in E. coli and K. pneumoniae invasive infections (1.2% and 1.9%, respectively, in 2023).
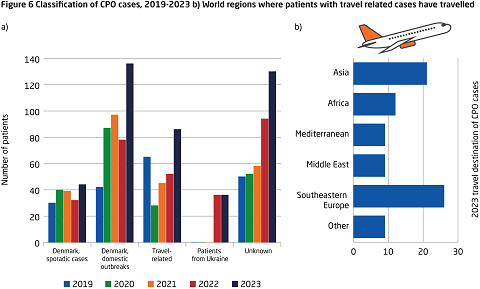
The number of carbapenemase-producing organisms (CPO) increased by 50% in 2023 (589 cases) compared to 2022 (392 cases). This rise is primarily due to outbreaks in Danish hospitals, as well as intensified screening and the reception of Ukrainian patients (Figure 6).
It is concerning that there is still high transmission of infections in hospitals. Therefore, it is important to continue focusing on general and supplementary infection control measures in daily operations.
While invasive infections with enterococci have declined since 2022, the number of vancomycin-resistant enterococci (VRE) increased until 2022, before falling by 17% in 2023 (845 isolates in 2022, 722 isolates in 2023). Despite the decline, infection prevention and control measures remain essential to prevent transmission and outbreaks.
After a decline in methicillin-resistant S. aureus (MRSA) cases during the COVID-19 pandemic, numbers increased by 20% in 2023 (3,649 cases) compared to 2022 (2,982 cases). MRSA screenings accounted for 45% of cases, while infections accounted for 55%. A total of 41 MRSA outbreaks were recorded in hospitals, nursing homes, and other institutions, involving 199 cases, 80 of which were infections.
Relationship Between Antibiotic Use and Resistance
Over the past decade, changes in antibiotic use for humans have been followed by changes in resistance patterns. For example, the steep rise in hospital use of penicillins and beta-lactamase inhibitors has coincided with increased resistance to piperacillin-tazobactam in invasive E. coli and K. pneumoniae infections (Figure 7a). Conversely, decreased use of fluoroquinolones (ciprofloxacin) has been followed by lower resistance rates in invasive E. coli and K. pneumoniae infections (Figure 7b).
Antibiotic Use and Resistance in the Veterinary Sector
The veterinary sector has also seen significant changes in antibiotic use and resistance in bacteria from livestock and food. For example, following the ban on zinc oxide in pig production, antibiotic use for piglets increased in 2023. Notably, the use of aminoglycosides such as neomycin and apramycin rose sharply. Simultaneously, resistance to aminoglycosides, particularly neomycin and gentamicin, increased in hemolytic E. coli and Salmonella enterica isolated from pigs.
For further information on antibiotic use in animals, see DANMAP 2023, Chapter 4, and on resistance in bacteria from livestock and food in Chapters 6, 7, and 9.
Want to Learn More?
Statens Serum Institut and DTU Food Institute invite you to the DANMAP seminar on November 18, 2024, focusing on key results from DANMAP, challenges in antibiotic treatment for humans and animals, and the real-world applicability of DANMAP.
The seminar will take place at Statens Serum Institut and online from 10:30 AM to 3:00 PM. It is relevant for all professionals who prescribe antibiotics or are interested in antibiotic use and resistance in Denmark. Registration is required via this link: DANMAP seminar on antibiotic use and resistance (ssi.dk).
The DANMAP 2023 report is already available at www.danmap.org. Summary DANMAP 2023 will also be available from November 18 2024.

(M. Attauabi, U.W. Sönksen, Department of Bacteria, Parasites, and Fungi)