No 51a - 2023
Syphilis 2022
Syphilis 2022
- In 2022, the Notification System for Infectious Diseases (NSID) received 676 notifications of syphilis cases, 80% of which occurred among men who have sex with men (MSM).
- The overwhelming majority of syphilis cases, in men and women alike, were acquired in Denmark.
- To some extent, syphilis is associated with HIV among MSM. However, the HIV status was known in advance for all MSM who were notified with syphilis in 2022. In contrast, among nine heterosexually infected persons who were concurrently notified with HIW, three were new detected cases.
- Syphilis occurred most frequently in the 30-49-year age group; the median age was 41 years for men and 38 years for women.
- In 2022, 12 of the 70 notified cases with syphilis in women were found in pregnant women, six hereof were Danish born. A single case of congenital syphilis was notified in 2022, in a child born abroad.
- Frequent testing of relevant groups may contribute to breaking infection chains thereby, in turn, helping to reduce the number of syphilis cases.
In 2022, 676 syphilis cases were notified to the NSID, Department of Infectious Disease Epidemiology and Prevention (DIDEP), Statens Serum Institut (SSI), Figure 1. The 676 cases occurred in 668 persons as 9 persons had more than one case notified in the course of the year.
For a detailed epidemiological description of the 2022 occurrence, please see the 2022 annual report on syphilis.
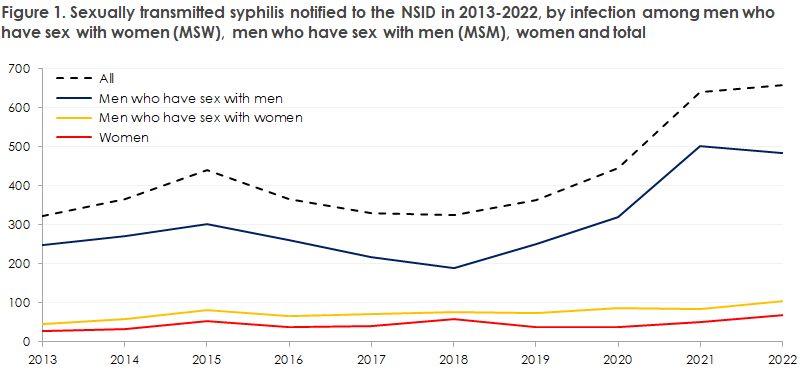
The number of notified syphilis cases has fluctuated somewhat in recent years, and even though MSM remains the group that accounts for the far greatest number of syphilis cases, a slight increase is observed among heterosexually infected persons. This trend is cause for concern as it may indicate that syphilis is gaining a foothold in the general population. For a considerable amount of time, focus and attention have been devoted to ensuring testing of MSM at risk of syphilis infection who may therefore be treated and avoid late sequelae. The increase observed among heterosexuals should be considered an important issue for doctors who need to consider syphilis as a possible differential diagnosis, also among heterosexuals. We may possibly also expect an increase among pregnant women as a direct consequence of the increase recorded among heterosexual people. In various countries, including the US, a considerable increase is seen in the number of congenital syphilis cases. Since 1 January 2010, the general screening of pregnant women has included syphilis, EPI-NEWS 27-33/2010.
In case of a positive screening test, confirmatory serological tests need to be conducted to confirm or refute the screening result. In several cases, it has been necessary to remind the patient’s GP about this, and in some cases syphilis that obviously needed treatment was detected through confirmative tests in these women. It is essential that we maintain screening of pregnant women in Denmark, particularly as an increase is observed in the number of syphilis cases among heterosexual people. Among 70 cases of syphilis detected in women in 2022, 12 were found in pregnant women, of whom six were Danish born. 2022 brought one case of syphilis in a child who was not born in Denmark. Even so, the case underpins the importance of screening.
A total of eight heterosexually infected people (men as well as women, including a transsexual) were notified as HIV positives, among whom around half had newly detected HIV. The newly detected cases were men who had become infected by sex workers abroad. The newly detected cases in heterosexuals, which were diagnosed concurrently with syphilis, underpin the importance of testing heterosexuals for HIV if their exposure is relevant.
The typical chancre carries no symptoms and furthermore is often localised to places where it goes undetected by the patient (the pharynx, vagina and/or rectum). Interruption of chains of infection therefore cannot be based on visits to the physician triggered by symptoms. Thus, it is essential that MSM at risk of infection are tested frequently, even if they have no symptoms. This ensures diagnosis and treatment of otherwise unacknowledged syphilis, whereby infection chains can be broken.
Swabbing for PCR is expedient for detection of Treponema pallidum DNA in chancre material and is typically positive approx. 14 days before any antibodies can be detected. Even so, serological testing also needs to be performed in order to monitor treatment effect.
(M. Wessman, S. Cowan, Department of Infectious Epidemiology and Prevention)
20 December 2023