No 44a - 2023
RS virus vaccine (RSV) authorised for use in elderly above 60 years of age and for vaccination of pregnant women /
DANMAP 2022
RS virus vaccine (RSV) authorised for use in elderly above 60 years of age and for vaccination of pregnant women
The Abrysvo® vaccine is authorised by the European Medicines Agency (EMA) for protection against RSV disease in the lower airways in persons aged 60 years or above. Furthermore, Abrysvo® is approved for use in pregnant women, who are vaccinated in gestational week 24-36. Hereby, passive protection is transferred to the infant from birth to six months of age against disease in the lower airways caused by respiratory syncytial virus (RSV).
A single 0.5 mL dose is given.
Read more about the vaccine in the SSI Vaccine Encyclopaedia.
National guidelines on the use of the vaccine have yet to be published. The vaccine does not form part of any vaccination programme, and vaccine costs are therefore defrayed by the person who
receives the vaccine.
The vaccine may be ordered at the SSI, using item number 105633.
(Department of Infectious Disease Epidemiology and Prevention)
DANMAP 2022
The DANMAP programme monitors antimicrobial consumption and resistance in humans, animals and foods in Denmark. The DANMAP collaboration has been operational since 1995. It publishes an annual report describing the primary findings related to the consumption of antimicrobials and the prevalence of antimicrobial resistance.
Below, we describe the main findings for 2022.
Antimicrobial consumption in humans
In 2022, the overall human antimicrobial consumption was 15.50 defined daily doses per 1,000 inhabitants per day (DID), which is slightly below the consumption observed in 2019 (15.77 DID), but 15% lower than the consumption recorded ten years ago (18.44 DID in 2013). In Denmark, primary healthcare is responsible for 87% of the antimicrobial consumption, whereas 12% is used in hospitals. The remaining consumption takes place in mental health services, private hospitals and hospices.
Antimicrobials and airway infections
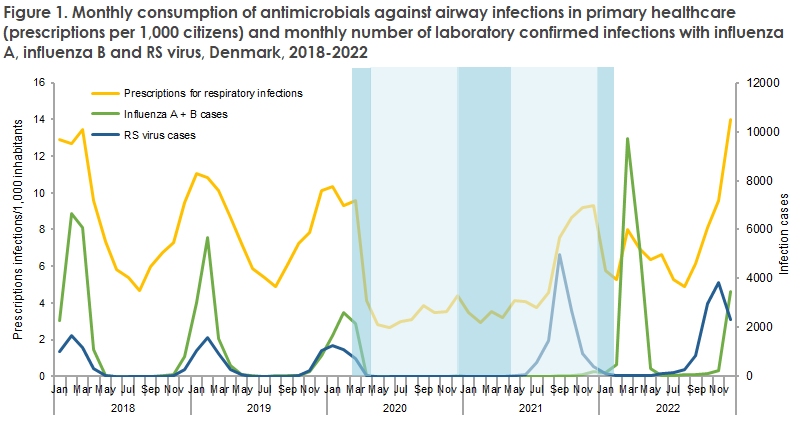
In primary healthcare, antimicrobial consumption was 13.59 DID, of which penicillins comprised 65%. The consumption of antimicrobials in primary healthcare is, in part, seasonal and follows the occurrence of various airway infections. In 2022, the habitual winter peak in the consumption of antimicrobials exceeded the level observed in 2018-2019. This was probably due to an early RSV epidemic in the autumn of 2022, which overlapped with an early influenza season and an outbreak of Group A streptococcal infections in the winter of 2022.
Antimicrobials at nursing homes
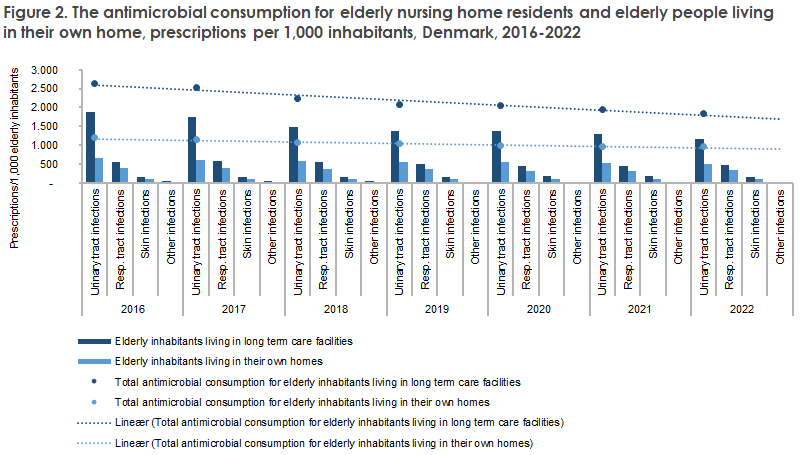
The consumption of antimicrobials for elderly nursing home residents was found to be 88% higher than the consumption for elderly people who live in their own home. The main difference is observed for antimicrobial consumption for treatment of urinary tract infection. This difference is observed despite the fact that antimicrobial consumption in nursing homes declined by 30% from 2016 to 2022 (from 2,636 prescriptions/1,000 citizens to 1,833 prescriptions/1,000 citizens). In the same period, antimicrobial consumption for elderly people who live in their own home declined by 18% (from 1,195 prescriptions/1,000 citizens to 976 prescriptions/1,000 citizens)
Antimicrobials in hospitals
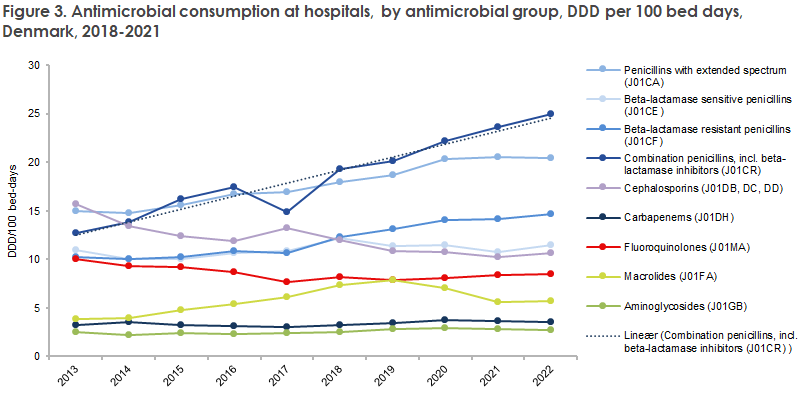
In contrast to antimicrobial consumption in primary healthcare, the consumption at hospitals has increased by 24% in the past ten years, stated per hospital bed in use (103.51 DDD per 100 bed days (DBD) in 2013 and 127.89 DBD in 2022). The increase was particularly pronounced for the combination of penicillins and beta-lactamase inhibitors, which has increased by 96% in the past ten years. In July and August 2022, the consumption of this type of antimicrobials declined steeply as the vaccine was on back order. Physicians, however, had access to penicillin/beta-lactamase inhibitor combinations via the special issue permits of the Danish Medicines Agency. Approx. 70,000 DDD penicillin/beta-lactamase inhibitors were purchased thanks to special issue permits in 2022, whereas the corresponding number for 2019-2021 was approx. 4,000.
Even though the total antimicrobial consumption at hospitals has increased in recent years, the consumption of the critically important antimicrobials (cephalosporins, fluoroquinolones and carbapenems) declined by 22% in the same period.
Antimicrobial resistance in clinical bacteria in humans
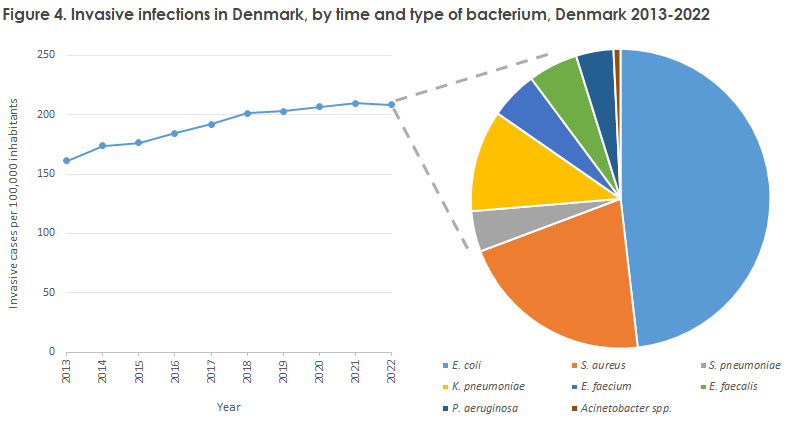
The occurrence of invasive bacterial infections in Denmark reached a plateau of 12,373 cases for the monitored species after having followed an increasing trend for the past ten years (8,954 cases in 2013, a 38% increase). One remarkable exception is invasive infections with Streptococcus pneumoniae, which has followed a declining trend for the past decade (789 cases in 2013, 538 cases in 2022), with considerable decreases in 2020 and 2021 (a total of 363 and 333 cases, respectively) during the COVID-19 epidemic. Escherichia coli remained the most frequent cause of invasive infections (50% of all cases), followed by Staphylococcus aureus and Klebsiella pneumoniae.
Following a declining occurrence of resistance for nearly all monitored bacterial species against the majority of antimicrobials during the COVID-19 epidemic, the resistance rates have now either stabilised or are increasing, even though they generally remain low. Even so, it remains important to focus on reducing antimicrobial consumption and to use narrow-spectrum antimicrobials whenever possible.
Following a considerable decline in the number of ESBL and pAmpC-producing E. coli in the blood stream from 2020 to 2021 (352 and 254 cases, respectively), the number increased to 336 in 2022; a 32% increase compared with the preceding year. CTX-M-15 remained the most frequent ESBL enzyme and was present in 52% of the cases. Monitoring of these E. coli is important as ESBL- and/or AmpC-positive bacteria are resistant to most betalactam antimicrobials. The occurrence of gentamicin resistance declined in the course of the decade (from 6.5% in 2013 to 4.5% in 2022), and carbapenem resistance remained below 1%.
Special attention should be devoted to the occurrence of resistance to piperacillin-tazobactam in K. pneumoniae as this resistance has increased in the past ten years and is close to 10% both for invasive infections (6.2% in 2013, 9.2% in 2022) and urinary tract infections (7.2% in 2013 and 9.9% in 2022) among hospitalised patients.
Combined resistance to third-generation cephalosporins, ciprofloxacin and gentamicin remained low for E. coli and K. pneumoniae in invasive infections (1.3% and 1.0%, respectively).
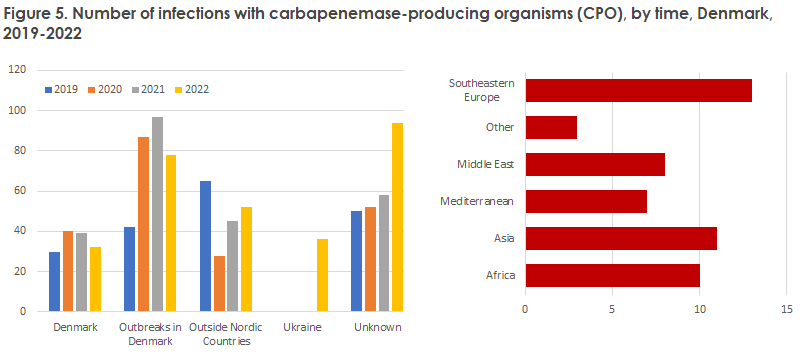
The number of carbapenemase-producing organisms (CPO) continued to increase in 2022 with 355 infected patients, compared with 242 in 2021. This was due, in part, to an influx of patients from the Ukraine, but also to an outbreak caused by contaminated Dicillin (dicloxacillin). The number of outbreaks at Danish hospitals remained stable, but for some of the existing outbreaks, the number of involved patients continued to increase. It is concerning that the transmission of infection remains high at hospitals. It therefore remains important to focus on the general and supplementary infectious hygiene precautions in daily work.
While a decline was observed in the number of invasive enterococcal infections, the number of vancomycin-resistant enterococci (VRE) continues to increase. In 2022, a total of 845 cases of VRE/vancomycin-variable enterococci (VVE) was identified, compared with 742 in 2021. This calls for intensified efforts in terms of infection prophylaxis and control.
Following a decline in the number of methicillin-resistant S. aureus (MRSA) during the COVID-19 pandemic, the number increased by 10% from 2021 to 2022 (2,996 cases). MRSA screening comprised 49% of the cases, whereas infections comprised 51%. A total of 39 MRSA outbreaks were registered at hospitals, nursing homes and other care facilities. The outbreaks counted a total of 143 cases, including 70 infections. A total of 50 bacteraemias were caused by MRSA, whereof seven were livestock-associated MRSA.
Want to learn more?
At the DANMAP seminar on 15 November 2023, Statens Serum Institut and DTU Food invite those interested to attend a summary of the main findings and results from adjacent research areas. The seminar is held in the Oticon Hall at the DTU in Lyngby from 10.30 a.m. to 3.00 p.m. The seminar is relevant for any professional who either prescribes antimicrobials or is interested in antimicrobial consumption and resistance in Denmark. Registering is mandatory, no later than 6 November 2023, to attend in person at the DTU, and no later than 13 November for online participation. The programme and a registration link are available here: DANMAP seminar on antibiotic consumption and resistance.
The DANMAP 2022 and Summary DANMAP 2022 reports are available at www.danmap.org.
(M. Attauabi, M. Lindegaard, U.W. Sönksen, Department of Bacteria, Parasites & Fungi, Statens Serum Institut
1 November 2023