No 42/43 - 2023
Update on the whooping cough epidemic and vaccination of pregnant women /
Respiratory infections in Denmark: Results from the extended sentinel surveillance in season 2021/22 and 2022/23
Update on the whooping cough epidemic and vaccination of pregnant women
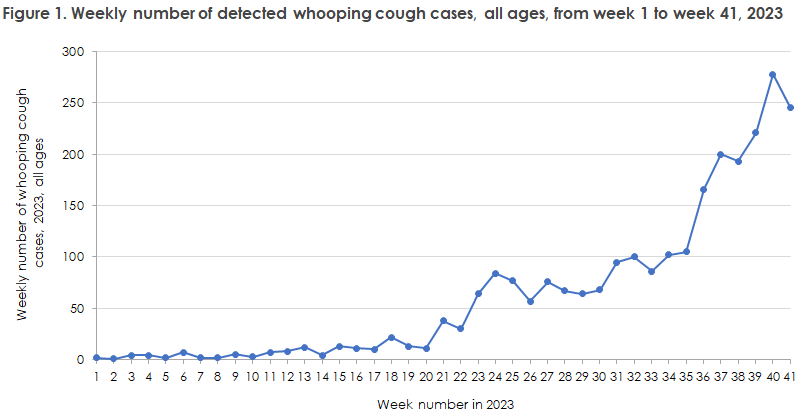
In early July, Statens Serum Institut informed that - following a prolonged period with very few cases during the COVID-19 epidemic - the whooping cough occurrence was on an increasing trend, EPI-NEWS 27/2023. The observed increase continued throughout summer and in late summer it reached an epidemic level, EPI-NEWS 36/2023. The epidemic is currently still ongoing with an average of 227 confirmed cases per week from week 37 to 41, Figure 1.
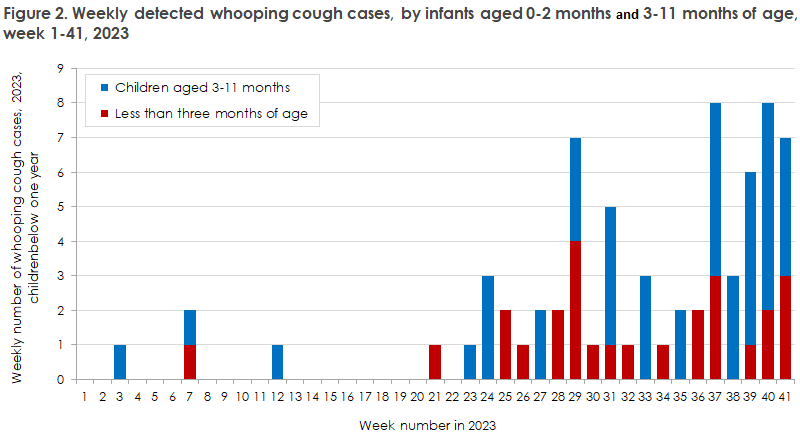
Whooping cough can be a very serious condition in infants, and, regrettably, this spring recorded an infant fatality due to whooping cough, EPI-NEWS 27/2023. Currently, 2-3 confirmed weekly cases are recorded among infants younger than three months, and 7-8 weekly cases among all children below one year of age, Figure 2. This is approx. four times higher than the normal level between epidemics.
Children in Denmark receive their first whooping cough vaccination at age three months. It is important that this vaccination is given timely. To protect the youngest children optimally until they are old enough to receive their first childhood vaccination, pregnant women are presently recommended whooping cough vaccination, normally in gestational week 24-32, EPI-NEWS 28-31/2023.
Based on the specific service code for whooping cough vaccination during pregnancy (8803), a total of 4,124 pregnant women were vaccinated in August. Based on the average number of 0-year-olds per month in the five Danish regions (used as a proxy for the number of pregnant women), the coverage in August was highest in the Capital Region of Denmark, the Central Denmark Region and in the Region of South Denmark, but somewhat lower in the North Denmark Region and lowest in Region Zealand. Data remain incomplete for September, but nearly 2,500 pregnant women were vaccinated in the first three weeks of the month.
If the pregnant woman has not yet been vaccinated, whooping cough vaccination may be given until one week before the expected labour date.
(T. Dalby, P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention)
Respiratory infections in Denmark: Results from the extended sentinel surveillance in season 2021/22 and 2022/23
Summary
Previously, the sentinel surveillance was only active in the winter semester, when influenza infection typically occurs. However, as of week 40 of 2021, surveillance was extended to include the rest of the year in connection with the COVID-19 pandemic. This improves the chance of discovering an increase in the incidence of influenza-like illness. Hence, the sentinel surveillance detects community infection among Danes of all ages with moderately severe respiratory symptoms who contact their general practitioner and therefore do not necessarily take sick leave, become hospitalised or are recorded by other monitoring systems. The laboratory-based component of the surveillance analyses swabs for a wide range of respiratory viruses. After two seasons of expanded sentinel surveillance, it is clear that this is a useful tool for monitoring respiratory infections in the Danish population all year.
Introduction of the sentinel system
Statens Serum Institut (SSI) has been monitoring influenza and other respiratory viruses for many years, and one of the surveillance systems used is sentinel surveillance. The sentinel surveillance scheme was developed primarily to monitor the occurrence of influenza in the population, thereby allowing the occurrence to be compared at different time points and across various European countries in the course of the influenza season.
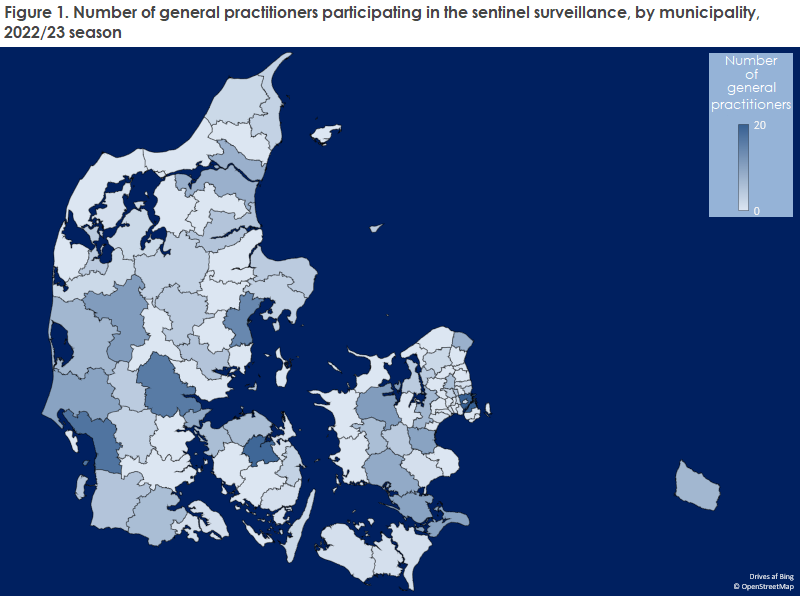
The sentinel surveillance consists of a number of general practitioners from all of Denmark who voluntarily and weekly report how many patients they have seen in their clinic and how large a share of these patients was seen due to influenza-like symptoms (ILS). Furthermore, throat swabs are taken from up to two patients per general practitioner per week. The swabs are sent to the influenza laboratory of the SSI where they are tested for a wide range of respiratory viruses in addition to influenza.
As the general practitioners who participate in the surveillance efforts are distributed across Denmark, the surveillance findings provide a good overview of whether community infection is occurring and if primary healthcare is burdened, Figure 1.
Previously, the sentinel surveillance was active only in the winter semester when influenza infection is typical, but surveillance was extended to also include the rest of the year in the wake of the COVID-19 pandemic. This improves the chance of monitoring any changes in the occurrence of influenza-like illness. The extended surveillance proved its worth in connection with the COVID-19 pandemic and also after the COVID-19 restrictions were lifted. For example, two unusual epidemics of respiratory syncytial virus (RSV) have occurred beyond the expected RSV season.
Influenza-like illness in the clinic
The participating general practitioners report the number of patients with influenza-like illness (ILI) and the total number of patients seen in their clinic each week. The diagnosis is based exclusively on the patient’s symptoms, that is without any laboratory testing. The definition of ILI is rapid presentation of symptoms, a minimum of one respiratory symptom (coughing, sore throat or difficulty breathing) and at least one constitutional symptom (fever > 38 °C, body aches, headache or malaise).
Disease occurrence is stated as a consultation percentage, i.e. the share of patients with influenza-like illness in the total number of consultations. This share is compared with a calculated base curve showing the expected share of influenza consultations for the season of the year, based on the five preceding seasons.
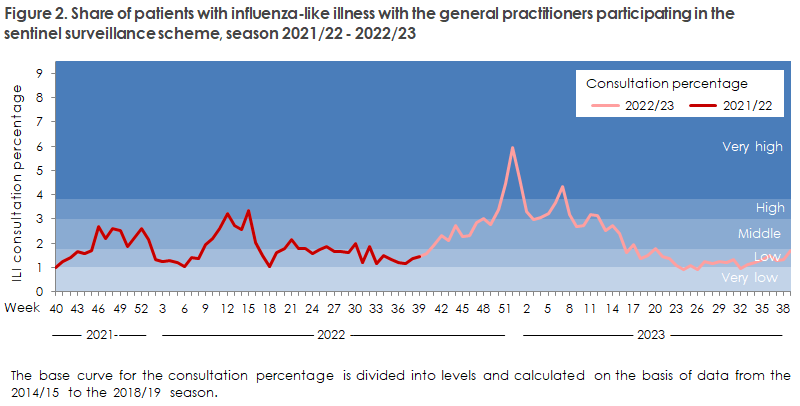
In the 2021/22 season, an average of 112 general practitioners per week electronically reported the occurrence of ILI patients in their clinic. From autumn until the end of the year, the ILI share remained at a low to moderate level compared with expectations. The share then declined to a very low level in the first eight weeks of 2022 when the share normally follows an inclining trend. However, as from week 9/2022 and coinciding with the lifting of all community restrictions due to COVID-19, a rapid increase was observed in the share of patients with ILI, and most other monitoring systems recorded a steep influenza activity increase. Influenza activity peaked in week 15/2022, after which the sentinel surveillance recorded a rapid decline to a low level of influenza activity.
In the recently completed 2022/23 season, an average of 123 physicians a week reported to the sentinel surveillance scheme. In autumn/winter, the share of ILI patients was generally moderate, but later in the season, the share repeatedly reached a high/very high level, Figure 2. It should be noted that the consultation percentage is not specific to influenza and therefore reflects influenza, COVID-19 and other influenza-like likenesses for which patients see their general practitioner.
Laboratory-based monitoring
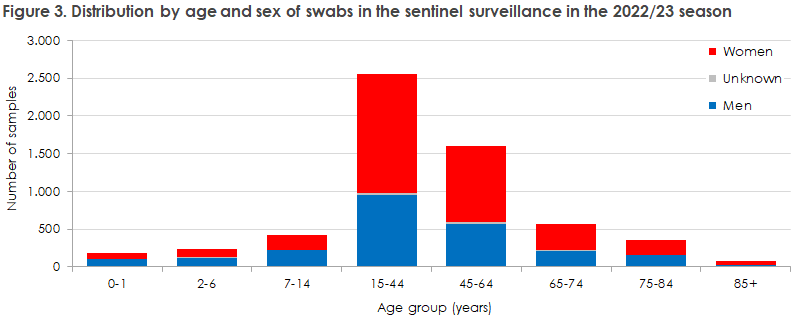
Since the 2021/22 season, the SSI has received a total of 10,251 swabs from the sentinel physicians. For the 2021/22 and the 2022/23 seasons, the swabs were collected from patients of all ages. More women than men were swabbed in nearly all age groups, but among the youngest children, more boys than girls were swabbed, Figure 3.
Virus findings
The laboratory-based component of the sentinel surveillance analyses the submitted samples to detect various respiratory viruses: influenza virus (type A and B, and the subtypes A(H1N1), A(H3N2), B/Victoria and B/Yamagata), respiratory syncytial virus (RSV) (type A and B), SARS-CoV-2, other common coronaviruses (HKU1, 229E, NL63, OC43), metapneumovirus, adenovirus, parainfluenza virus (types 1-4) and rhino- and enterovirus.
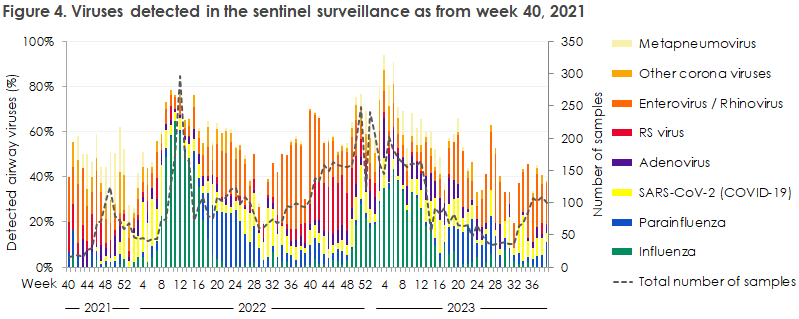
The extended sentinel surveillance has been operational since week 40/2021 when rhino-/enterovirus circulated, and the final part of the unusual RSV summer season was also recorded in samples from the sentinel physicians, Figure 4. Subsequently, the autumn period brought metapneumovirus and the other corona viruses. From week 46/2021, SARS-CoV-2 was also detected in the samples. This coincided with relaxed restrictions in relation to the COVID-19 pandemic. In early 2022, influenza activity rose substantially for the first time since the arrival of the COVID-19 pandemic, coinciding with the majority of the restrictions being lifted as of 1 February 2022. Influenza peaked in week 11/2022 and started receding as from week 21/2022. Parainfluenza virus increased as the influenza occurrence declined and continued throughout the summer of 2022. Rhino/enterovirus once again increased during spring and summer. In the late summer of 2022, another early RSV season started. This season peaked in the course of autumn, concurring with a rather large occurrence of rhino/enterovirus. In both years, RSV was followed by an increase in the occurrence of metapneumovirus. Sporadic influenza cases were observed from week 41/2022 until the influenza activity gained momentum in December. The 2022/23 season was a long season comprising three waves, which only receded by March. Once again, an increase was seen in the number of detected parainfluenza cases after the influenza level had declined. The late summer of 2023 recorded an increasing number of SARS-CoV-2 cases.
Co-infections
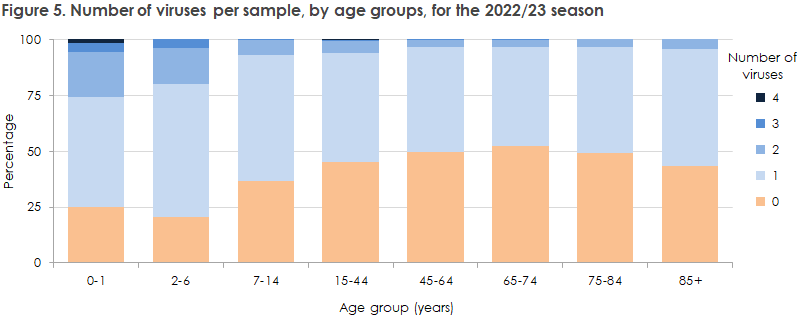
Some patients have more than one respiratory virus detected in their swab, Figure 5. Children, in particular, have more than one respiratory virus detected. In some cases, as many as four respiratory viruses are detected in a single swab. In contrast, the oldest patients typically only have one respiratory virus detected and in rare cases two viruses.
Influenza types
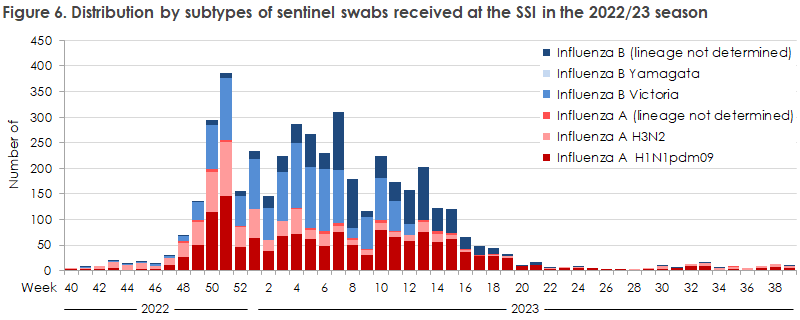
The 2021/22 season was dominated by influenza A of the H3N2 subtype. In contrast, the 2022/23 season was mixed. Influenza B/Victoria dominated, but co-circulation was recorded primarily of influenza A(H1N1) and, to a more limited extent, influenza A(H3N2), Figure 6. A fourth influenza virus, B/Yamagata, has not been recorded since the COVID-19 lockdown in 2020.
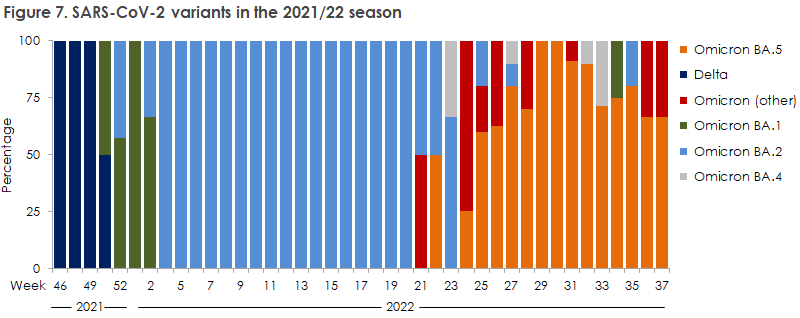
SARS-CoV-2 variants
A variant analysis of SARS-CoV-2 positive swabs was conducted for the 2021/22 season, Figure 7. In weeks 46-51, Delta was the dominant variant in the sentinel surveillance. Omicron BA.1 became dominant from around the end of 2021 but was swiftly surpassed by Omicron BA.2. From week 21/2022 onwards, Omicron BA.5 was detected along with other less frequent Omicron variants. Variant analyses covering the 2022/23 season are currently being conducted.
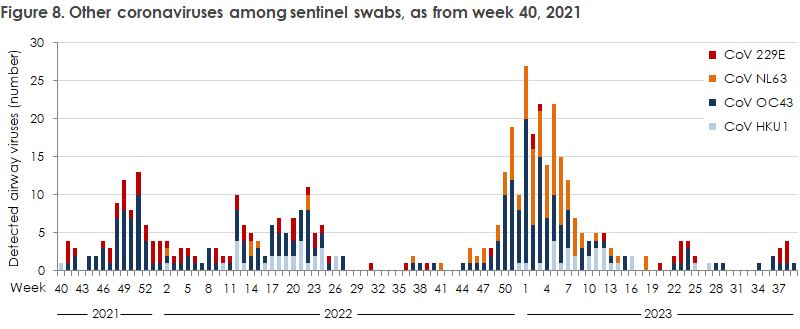
Other coronaviruses
The sentinel surveillance also distinguishes between four other coronaviruses: 229E, NL63, OC43 and HKU1. In the 2021/22 season, OC43 accounted for most cases, followed by 229E and HKU1.
The cases occurred in the course of the whole year, but slightly more cases were detected in December 2021 and in the spring of 2022. In the 2022/23 season, a wave of OC43 and NL63 was observed in the winter semester, followed by HKU1, Figure 8.
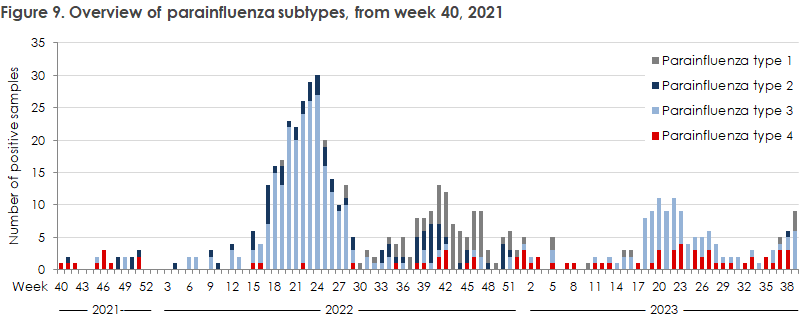
Parainfluenza virus
The sentinel surveillance distinguishes between four types of parainfluenza virus; type 1, 2, 3 and 4. In the 2021/22 season, an outbreak was recorded in spring and early summer of parainfluenza virus, mainly of type 3. The autumn of 2022 witnessed the beginnings of a minor outbreak of parainfluenza, primarily of type 1 and 2. This outbreak had largely receded by the end of January 2023.
As of week 18/2023, another parainfluenza virus outbreak was recorded; this time of type 3, Figure 9.
Symptom overview
When the sentinel physicians swab a patient, they also complete a questionnaire on the patient’s symptoms. The most frequently reported symptoms are coughing, general malaise and sudden-onset symptoms. Difficulty breathing and headache occur only rarely in patients positive for one of the respiratory viruses looked for in the sentinel system.
For more information about the sentinel system, including information about how to register to participate in the surveillance, please see Tilmelding til sentinelovervågning (Registering for the sentinel surveillance scheme).
(A.B. Botnen, R. Trebbien, the Influenza Section, L.D. Rasmussen, Virus Monitoring and Research, M. Rasmussen, Virus Research and Development, L.K. Knudsen, H-D. Emborg, C. Munkstrup, L.S. Vestergaard, Department of Infectious Disease Epidemiology and Prevention)