No 3 - 2023
Increase in infections with group A streptococci in Denmark
Off-label primary vaccination with variant-updated COVID-19 booster vaccines
Increase in infections with group A streptococci in Denmark
As described in EPI-NEWS 51/2022 various European countries are currently observing a steep increase in disease caused by group A streptococci (also coined “GAS”, “haemolytic streptococci of group A” or “Streptococcus pyogenes”). Internationally, this increase is primarily seen in children and paediatric fatalities have been reported. Some countries have also recorded an increase in the number of invasive disease cases caused by the same bacterium. Preliminary reports do not indicate increased bacterial virulence of the bacterium, and one possible explanation for the increase in case numbers may be a rebound effect following the COVID lock-downs imposed in many countries.
Currently, Denmark is also witnessing an increase in the number of cases affected by group A streptococci. On 12 January 2023, the Danish Health Authority issued an AMC statement instructing pediatricians, general practitioners and on-call doctors to be extra attentive to these infections and particularly to signs of worsening despite relevant management with penicillin/antibiotics. Due to the situation in the remaining European countries, it is important to remain attentive to cases, including paediatric cases.
Denmark is currently recording a considerable increase in the number of GAS-positive non-invasive culture tests such as throat swabs, wound swabs and similar (e.g., pharyngitis, scarlet fever), Figure 1. The highest incidences are being recorded in East Jutland, Copenhagen City and suburbs and North Zealand. In all areas of Denmark, apart from the island of Bornholm, the level of non-invasive cases is 2-3 times higher than is normally the case during seasonal peaks.
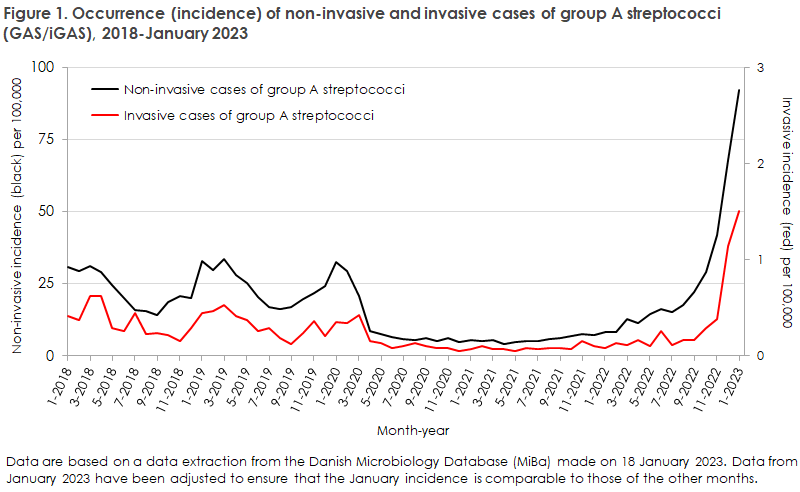
*Footnote for the trend graph: Data are based on a data extraction from the Danish Microbiology Database (MiBa) made on 18 January 2023. Data from January 2023 have been adjusted to ensure that the January incidence is comparable to those of the other months.
A considerable increase in the number of invasive cases (iGAS) was also observed, i.e. sepsis or meningitis, Figure 1. These trends were mainly observed among elderly people aged more than 65 years, but also, in part, among children below five years of age. The iGAS increase is being observed in all Danish areas apart from the island of Bornholm. In addition to sepsis and meningitis the bacterium may cause necrotising soft tissue infections and streptococcal toxic shock syndrome. Currently, no signs have been recorded of increased mortality in relation to the invasive cases in Denmark.
Management in general practice
In general practice, GAS pharyngitis is easily diagnosed using specific antigen tests. These tests enjoy a high sensitivity. In the absence of allergy, these infections are treated with penicillin as penicillin resistance does not occur. Antimicrobial treatment mainly reduces the risk of complications and to some extent also shortens the duration of the condition and the risk of spreading the infection.
GAS is transmitted through droplets and by contact. Patients should be informed that pharyngitis caused by GAS is a highly infectious condition that carries a high risk of transmission within the household and in institutions, etc. and should be instructed to follow the general prophylactic advice of the Danish Health Authority. As a rule of thumb, patients are non-infectious 24 hours after initiating antimicrobial treatment. The Danish Health Authority recommends that children do not attend day-care and similar institutions in the 48 hours after initiating treatment.
In case of iGAS, other countries including, e.g., England, Canada and Holland, offer antimicrobial prophylaxis for close contacts belonging to specific risk groups. General recommendations to this effect are not in place in Denmark. However, following medical assessment, post-exposure antibiotics may be considered in case of GAS or iGAS for close contacts belonging to a risk group, e.g., immunosuppressed patients. Family members and other close contacts should be informed of the infection risk and be encouraged to see a doctor in case of symptoms of illness.
Due to the situation in the remaining European countries it is important to remain attentive to cases, including paediatric cases.
The SSI has prepared a risk assessment and will establish an outbreak website where data will be updated regularly for as long as the increased incidence of GAS/iGAS pertains. The European Centre of Disease Prevention and Control (ECDC) monitors the situation in Europe.
(C. Munkstrup, S. Nielsen, T. Funk, P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention, D. Kristensen and Hervig Jacobsen, Department for Data Integration and Analysis, S. Hoffmann, Department for Bacteria, Parasites and Fungi, P. Jokelainen, the Joint Medical Secretariat of Infection Preparedness).
Off-label primary vaccination with variant-updated COVID-19 booster vaccines
In its latest guidelines, the Danish Health Authority has assessed that the variant-updated vaccines Comirnaty Original/Omicron BA.4-5 and Spikevax Original/Omicron BA.4-5 may be used off-label for primary vaccination if the monovalent Wuhan-based vaccines are unavailable at the vaccination site. This is in line with the statement published by the European Medicines Agency on 6 December 2022. Primary vaccination with Comirnaty Original/Omicron BA.4-5 or Spikevax bivalent Original/Omicron BA.4-5 is not comprised by the approval basis why such vaccination will be off-label.
Furthermore, please note that primary vaccination with variant-updated Comirnaty Original/Omicron BA.4-5 and Spikevax Original/Omicron BA.4-5 does not trigger a EU-certified Corona Certificate (corona passport), EPI-NEWS 47/2022.
(Department of Infectious Disease Epidemiology and Prevention)