No 24 - 2023
Screening of pregnant women for hepatitis B, HIV and syphilis, 2022
Screening of pregnant women for hepatitis B, HIV and syphilis, 2022
- In 2022, pregnancy screening detected 112 pregnant women with hepatitis B, 26 with HIV and 12 with confirmed syphilis.
- In 2022, 21 of the 26 pregnant women with HIV had previously been diagnosed with HIV and were undergoing treatment.
- Half of the pregnant women with syphilis were Danish.
- All pregnant women, including pregnant women previously diagnosed with hepatitis B, must be screened for all three conditions as a positive test result from the pregnancy screening requires special measures at the maternity ward.
- All pregnant women with hepatitis B, syphilis or HIV are to be referred to a specialised department.
- Midwives and other healthcare workers who vaccinate neonates whose mothers are hepatitis B carriers must register this in the JMC (Joint Medicine Card)/DVR (Danish Vaccination Register).
- The GP must conclude vaccination of children born by hepatitis B carrier mothers and ensure serological testing of vaccination effect in the children one month after they have concluded the vaccination series.
Screening of pregnant women for hepatitis B virus (HBV) was introduced on 1 November 2005, and screening for HIV and syphilis was initiated on 1 January 2010.
The 2022 annual report is now available.
In 2022, a total of 64,841 blood type analyses were performed in pregnant women. Practically all of these women (99.9%) were tested for hepatitis B virus, HIV and syphilis.
Thus, the overwhelming majority of pregnant women accept the offer of hepatitis B, HIV and syphilis screening; and therefore nearly all potential cases of mother-to-child transmission with the three conditions can be avoided.
The majority of pregnant women with hepatitis B, 109 among 112, were born abroad and the remaining three women were born in Denmark by mothers from endemic countries. In 2022, 6 out of 12 pregnant women with syphilis were Danish. This shows that, in Denmark, syphilis is not exclusively a condition that occurs among men who have sex with men or immigrants from high-incidence countries; it has been re-introduced among heterosexual Danes.
In 2022, two women failed to have an extended confirmatory syphilis test performed despite several attempts to trace these patients.
Whereas the overwhelming majority of HIV and hepatitis B screening tests are confirmed positive, a very large share of the syphilis screening tests performed are false positives, indicating previous infection, etc. In 2022, 90 pregnant women received a positive syphilis screening test result, 88 of whom (98%) also had confirmatory serological tests performed, of which 12 tested positive.
In case of a positive screening result, the pregnant woman therefore needs to be informed that the majority of screening findings are false positives, but that an extended analysis is needed to confirm or disprove the result.
Furthermore, the pregnant woman needs to be informed that - if she does, indeed, have syphilis, HIV or hepatitis B - the conditions are treatable so that she will not transmit the condition to her child.
Additionally, the pregnant woman needs to be informed of the importance of having her sexual partner(s) tested and, if needed, treated.
The general practitioner's tasks in relation to pregnancy screening
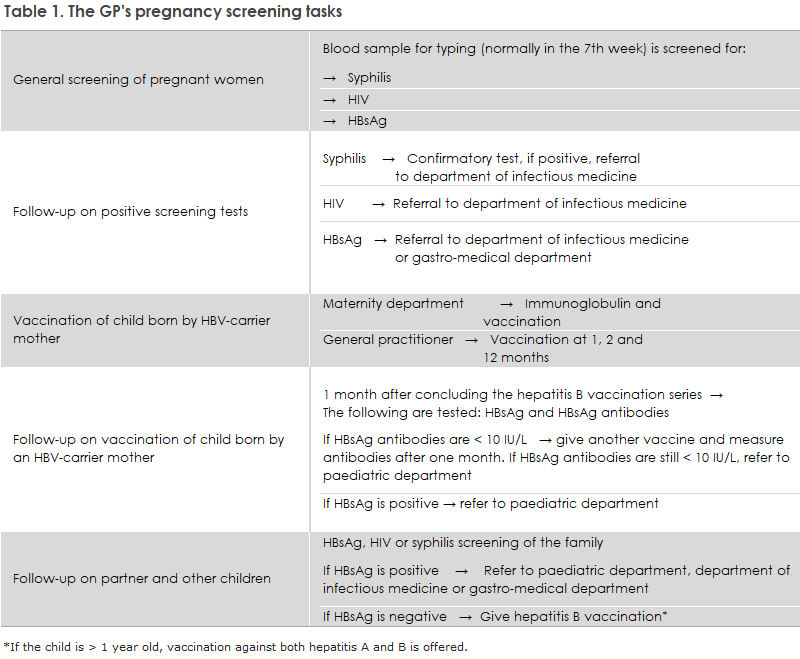
The general practitioner's tasks in relation to pregnancy screening are presented in Table 1.
All pregnant women must be offered screening for HIV, hepatitis B and syphilis
Even if the pregnant woman or her GP knows that she has HIV or chronic hepatitis B, it is important that the pregnant woman is offered full pregnancy screening. This is because the communication between Statens Serum Institut (SSI) and the maternity wards is based on the information that the SSI receives from the laboratories performing the pregnancy screening blood samples. The SSI needs to notify the maternity wards of the need to administer hepatitis B vaccination and immunoglobulin to neonates born by carrier mothers and subsequently document this, and this can only be done if the SSI is informed by the laboratory of the positive test.
Pregnant women who stay in the country as undocumented immigrants may be examined by a physician at a Red Cross health clinic in Copenhagen or Aarhus. Here, pregnancy screening is also offered, but this service does not form part of the public offer of care for childbearing women. Maternity wards must remain attentive to taking blood samples to test for syphilis and hepatitis B, and perform a rapid HIV test, if a woman in labour of unknown status is admitted to hospital. See the guideline published by the Danish Health Authority on general screening of pregnant women for infection with hepatitis B virus, human immune deficiency virus (HIV) and syphilis.
Pregnant women who test positive must be referred to a specialised department
It is important that treating physicians refer any pregnant woman who has had one of the three infections detected in the screening to the relevant specialist department, even if the woman in question has no infection symptoms, Table 1. Just as pregnant women receive treatment for HIV and syphilis, pregnant women with a high HBV virus amount (>106 IU/ml) will typically be offered treatment at approx. 28 weeks of gestation, which may reduce the risk of intrauterine transmission, cf. guidelines on the treatment of hepatitis, prepared by the Danish Society for Gastroenterology and Hepatology (in Danish language).
In accordance with the Danish Health Authority's guideline on general screening of pregnant women for infection with hepatitis B, HIV and syphilis, the pregnant woman's partner and remaining children, should be scheduled for a blood sample.
According to the Danish Health Authority’s guideline on HIV, hepatitis B and C virus published in 2013, all children born by HBV carrier mothers who receive hepatitis B vaccination at birth and subsequently at the GP should be tested to confirm that the vaccination has taken and to test for current infection one month after the vaccination series has been concluded, Table 1, i.e. when the child is 13-15 months old. This is necessary because intrauterine infection occurs in some children, in which case the vaccine is ineffective. The responsibility for performing this test lies with the GP, Table 1. If the child has become infected, he or she is referred to a paediatric department. If the child is insufficiently covered (anti-HBs <10 IU/L) despite the vaccinations, an additional vaccination may be given after which antibodies are measured one month later. If the child is still insufficiently covered, he or she is referred to a paediatric department. Statens Serum Institut sends out reminders to the GPs about hepatitis B vaccination of children born by hepatitis B carrier mothers and about subsequent testing of these children.
Hepatitis B vaccination must be recorded in the JMC/DVR already at birth
Physicians, nurses and midwives who give the vaccine have a legal obligation to register this in the JMC/DVR.
Previously, it was a problem that neonates would appear in the JMC/DVR only some days after labour. This has been changed so that the children can be found by searching for their civil registration number (CVR number) shortly after birth.
Hepatitis B vaccination and the vaccination course termed “Hepatitis B post-exposure for neonates” (In Danish: ”Hepatitis B post-eksposition til nyfødte”) are added under Add new vaccination (In Danish: “Opret ny vaccination”) in the JMC/DVR. Immunoglobulin cannot be registered in the JMC/DVR as it is not a vaccine.
When a vaccination course is established, the parents and the GP will automatically gain access to the dates at which the next vaccinations are to be given.
(L.H. Holm , S. Cowan, Department of Infectious Disease Epidemiology and Prevention)