No 49/50 - 2022
Children who are to receive two doses of influenza vaccine need to start their vaccination course no later than 21 December 2022
Syphilis 2021
Children who are to receive two doses of influenza vaccine need to start their vaccination course no later than 21 December 2022
Children aged 2-6 years are recommended influenza vaccination in the current influenza season. Children who have not previously received influenza vaccination and who therefore require primary vaccination are recommended two doses at a 28-day interval. Children who have received influenza vaccination in a past year only need a single dose this season.
The influenza vaccines used for children in Denmark (Fluenz Tetra) expire on 18 January 2023. In practice, this means that those children in the target group who are to receive their first vaccination dose should do so no later than 21 December 2022 in order for them to have time to receive their second dose 28 days before 18 January 2023 when the vaccines expire. Therefore, 21 December 2022 is the last day that children may receive their first dose in a primary vaccination course. Children who received influenza vaccination in a previous year or who have already received their first dose may be vaccinated until 15 January 2023.
(The Danish Health Authority)
Syphilis 2021
- Following a decline in the number of notified syphilis cases among men who have sex with men (MSM) in the 2015-2018 period, syphilis has again followed an increasing trend in this group. An increase has also been observed among heterosexual (HTX) men and women, but this increase is much more limited than that observed among MSM. In 2021, the Notification System for Infectious Diseases (NSID) received 634 notifications of syphilis cases, 493 (86% of the notified cases for which the mode of infection was stated) of which occurred among MSM.
- In 2021, 93% of the notified men and 94% of the notified women had become infected in Denmark. As was the case in 2020, this was probably due to COVID-19-related travel restrictions. In 2021, like in 2020, the fewer travel-related cases did not produce a reduction in the total number of notified cases.
- Syphilis is still, in part, linked to HIV-positive MSM. In 2021, 102 (22%) of the 465 MSM for whom a HIV status was stated were already HIV positive at the time of their syphilis diagnosis. No cases were notified of a concurrent diagnosis of syphilis and HIV. No heterosexually infected men or women with syphilis were notified as HIV positives.
- Syphilis occurred more frequently among 30-39-year-olds; the median age was 37 years for men and women alike.
- In 2021, nine of the 52 notified cases of syphilis among women affected pregnant women, including five women who had been born in or adopted to Denmark. This relatively high share of women with syphilis who are pregnant indicates that an undiagnosed fraction may exist among women and probably also among heterosexual men. The pregnancy screening found a total of 15 women with confirmed syphilis Thus, six of the pregnant women with syphilis found as part of the pregnancy screening (40%) had not been notified to the NSID.
- No cases of congenital syphilis were notified in 2021.
- Frequent testing of relevant groups may contribute to breaking infection chains thereby, in turn, helping to reduce the number of syphilis cases. All MSM are recommended annual testing for HIV and other relevant sexually transmittable infections. MSM who lead an active sex life and who do not always use a condom are recommended testing 2-4 times annually. MSM who are offered medical HIV prophylaxis, pre-exposure prophylaxis (PrEP), are tested two or four times annually when receiving their prophylactic medicine.
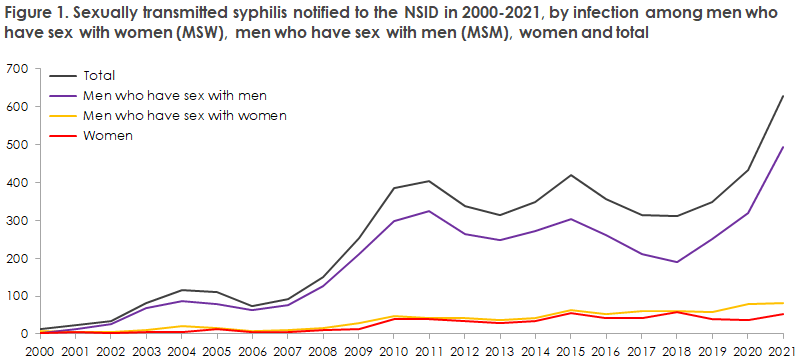
In 2021, 634 syphilis cases were notified to the NSID, Department of Infectious Disease Epidemiology and Prevention (DIDEP), Statens Serum Institut (SSI). The 634 cases occurred in 622 persons as 12 persons had two cases notified in the course of the year. A total of 582 of the cases occurred in men and 52 in women. A total of 493 cases were notified among MSM who therefore continue to comprise the main share of the notified syphilis cases, Figure 1.
For a detailed epidemiological description of the 2021 occurrence, please see the 2021 annual report on syphilis.
In 1994-2001, syphilis was very rare in Denmark; the period saw fewer than 20 notified cases per year. As from the turn of the millennium, an increase has been observed in the number of cases.
This increase was particularly pronounced in the 2006-2011 period. Following a decline in the number of notified syphilis cases in 2012, the number has subsequently fluctuated somewhat: in the 2015-2018 period, a decline was observed in the number of notified syphilis cases, whereas an increase is currently being recorded. The current increase is mainly observed among MSM.
Since 1 January 2010, the general screening of pregnant women has included syphilis, among others EPI-NEWS 27/33-2010. In case of a positive screening test, confirmatory serological tests need to be made to confirm or refute the screening result. In several cases, it has been necessary to remind the patient’s GP about this, and in some cases syphilis that obviously needed treatment was detected through confirmative tests in these women.
Among 52 cases of syphilis detected in women in 2021, nine were notified as pregnant women, five of whom were born in or adopted to Denmark. The relatively high share of women with syphilis who are pregnant indicates that an undiagnosed fraction may exist among women and probably also among heterosexual men who are not tested because they have no symptoms. Even though heterosexual men and women do not belong to the groups that should regularly undergo syphilis testing because they account for only a limited share of those infected, syphilis today needs to form part of the differential diagnostic considerations when relevant symptoms are observed, and syphilis testing should therefore be considered more frequently than was previously the case in this group.
In 2021, the pregnancy screening observed a total of 15 women with confirmed syphilis, among whom six pregnant women with syphilis (40%) had not been notified to the NSID.
Syphilis occurs in one of the following disease stages: primary, secondary, early latent, late latent - including latent of unknown duration - and tertiary syphilis. Primary and secondary syphilis cases have symptoms. Tertiary syphilis occurs rarely in the Western world, and at this stage patients may also have symptoms. Generally, the syphilis screening is rooted in a combination of medical histories, clinical particulars and serology. The serological findings in secondary and early latent syphilis overlap considerably and are distinguished by the presence or absence of symptoms.
Syphilis serology can be difficult to interpret why consultation should be sought from relevant specialised healthcare professionals (dermatologists and/or specialists of infectious medicine) whenever the slightest doubt exists concerning syphilis infection.
The typical chancre in the primary syphilis stage is typically pain free. Furthermore, these chancres are often localised to places where they go undetected by the patient (the pharynx, vagina and/or rectum). Interruption of chains of infection therefore cannot be based on visits to the physician triggered by symptoms. Therefore, it is essential that MSM who lead an active sex life undergo frequent serological testing even though they have no symptoms. This ensures diagnosis and treatment of otherwise unacknowledged syphilis, whereby infection chains can be broken.
Swabbing for PCR from chancre-suspicious ulcers is expedient for detection of Treponema pallidum DNA and is typically positive approx. 14 days before any antibodies can be detected. Even so, serological testing always needs to be performed in order to monitor treatment effect.
Clinical notification of syphilis is mandatory and should be effected electronically. It is important that healthcare professionals notify any syphilis cases that come to their attention. An increased notification rate will improve monitoring efforts thereby ensuring notification even of the syphilis cases that are not notified by the treating healthcare professional who is responsible for doing so.
(S. Cowan, L.H. Holm, Department of Infectious Disease Epidemiology and Prevention, J. Tolstrup, Department of Dermatology, Zeeland University Hospital, Roskilde, S. Hoffmann, Department of Bacteria, Parasites and Fungi).
14 December 2022