No 1/6 - 2022
Syphilis 2019 and 2020
Syphilis 2019 and 2020
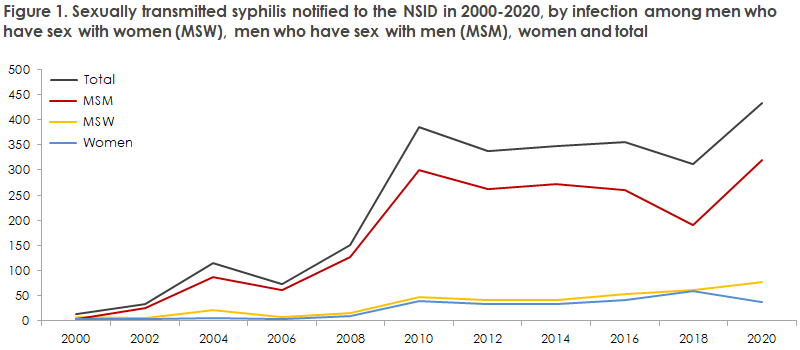
- Following a decline in the number of notified syphilis cases among men who have sex with men (MSM) in the 2015-2018 period, syphilis has again followed an increasing trend in 2019 and 2020. A corresponding increase has not been observed among heterosexual (HTX) men and women. In 2019, the Notification System for Infectious Diseases (NSID) received 365 notifications of syphilis cases, 69% of which occurred among MSM. In 2020, the number was 446, of which 72% occurred among MSM.
- In 2019, 84% of the notified men and 81% of the notified women had become infected in Denmark. In 2020, the corresponding figures were 92% and 94%, respectively. The increase in the share of syphilis cases acquired in Denmark was probably due to COVID-19-induced travel restrictions. Even so, fewer travel-related cases have not produced a reduction in the total number of notified cases.
- Syphilis is, in part, linked to HIV among MSM. In 2019 and 2020, 28% and 24% of the syphilis cases notified among MSM for whom the HIV status was not provided tested HIV positive. Hereof, 87% and 94% were known HIV infectees.
- Syphilis occurred more frequently among 40-49-year-olds in 2019 and 2020 alike: the median age in both years was 40 years for men, whereas the median age for women was 32 year in 2019 and 34 years in 2020.
- In 2019, seven of the 39 notified cases with syphilis in women were found in pregnant women, five hereof were Danish born. In 2020, a total of 37 syphilis cases were notified among women, whereof nine were pregnant, five hereof were Danish born. This indicates that an undiagnosed share may exist among women and probably also among heterosexual men. A single case of congenital syphilis was notified in 2019.
- Frequent testing of relevant groups can help break infection chains and thus contribute to reducing the number of syphilis cases.
In 2019, 365 syphilis cases were notified to the NSID, Department of Infectious Disease Epidemiology and Prevention (DIDEP), Statens Serum Institut (SSI). The 365 cases occurred in 353 persons as 12 persons had two cases notified in the course of the year.
In 2020, the figure was 446 cases occurring in 435 persons, as 11 persons had two cases notified in the course of the year.
For a detailed epidemiological description of the 2019 and 2020 occurrence, please see the 2019 and 2020 annual report on syphilis.
In 1994-2001, syphilis was very rare in Denmark; the period saw less than 20 notified cases per year. As from the turn of the millennium, an increase has been observed in the number of cases. This increase was particularly pronounced in the 2006-2011 period. Following a decline in the number of notified syphilis cases in 2012, the number has subsequently fluctuated somewhat: in the 2015-2018 period, a decline was observed in the number of notified syphilis cases, whereas an increase is currently being recorded. The current increase is observed among MSM only. The number of notified syphilis cases diagnosed in 2021 was not calculated as we still expect to receive quite a few notifications for 2021. Already in late December 2021, a total of nearly 600 syphilis notifications had been received. Thus, we may conclude that the increase observed in the previous two years continued in 2021.
Since 1 January 2010, the general screening of pregnant women has included syphilis, EPI-NEWS 27-33/2010. In case of a positive screening test, confirmatory serological tests need to be made to confirm or refute the screening result. In several cases, it has been necessary to remind the patient’s GP about this, and in some cases syphilis that obviously needed treatment was detected through confirmative tests in these women.
Among 39 cases of syphilis detected in women in 2019, seven were found in pregnant women, five of whom were Danish born. In 2020, a total of 37 women were notified, whereof nine were pregnant - five of whom were Danish born. This seems to indicate that an undiagnosed share exists among non-pregnant women and heterosexual men who are not tested because they have no symptoms. Even though heterosexual men and women do not belong to the groups that should regularly undergo syphilis testing because they account for only a limited share of those infected, syphilis today needs to form part of the differential diagnostic considerations when relevant symptoms are observed, and syphilis testing should be considered more frequently than was previously the case.
The typical chancre carries no symptoms and furthermore is often localised to places where it goes undetected by the patient (the pharynx, vagina and/or rectum). Interruption of chains of infection therefore cannot be based on visits to the physician triggered by symptoms. Thus, it is essential that MSM are tested frequently, even if they have no symptoms. This ensures diagnosis and treatment of otherwise unacknowledged syphilis, whereby infection chains can be broken.
Swabbing for PCR is expedient for detection of Treponema pallidum DNA in chancre material and is typically positive approx. 14 days before any antibodies can be detected. Even so, serological testing also needs to be performed in order to monitor treatment effect.
Since 2019, MSM have had the opportunity to be offered PrEP (Pre Exposure Prophylaxis, HIV medicine taken prior to exposure). The introduction of PrEP has brought a decline in the number of HIV diagnoses among MSM, EPI-NEWS 47/48 2021. Concurrently, an increase has been observed in both syphilis and gonorrhoea among MSM, EPI-NEWS 51/2021. The increases may, in part, be explained by the fact that medicinal protection against HIV has reduced the use of condoms. This may lead to more infections with other sexually transmittable conditions than HIV.
Furthermore, the increases may, in part, be explained by increased testing activity in connection with the dispensing of PrEP, which is done 1-4 times annually.
(S. Cowan, A.K. Hvass, Department of Infectious Disease Epidemiology and Prevention, J. Tolstrup, Department of Dermatology, Zeeland University Hospital, Roskilde, S. Hoffmann, Department of Bacteria, Parasites and Fungi)
9 February 2022