No 45 - 2021
False positive influenza samples following vaccination of children with the live, attenuated influenza vaccine
Botulism
Participate in a European conference on infectious disease epidemiology
False positive influenza samples following vaccination of children with the live, attenuated influenza vaccine
Statens Serum Institut (SSI) wants to draw attention to the fact that children who have received the live attenuated influenza vaccine Fluenz Tetra® may have a false positive influenza test in the days following their vaccination due to secretion of vaccine virus. According to the summary of product characteristics, secretion peaks 2-3 days after vaccination, but in some cases secretion has been observed for nearly 14 days. The treating physician should therefore be attentive to whether the child has been vaccinated within the past 14 days.
As described in EPI-NEWS 38-39/21, children aged 2-6 years are recommended vaccination with the nasal spray vaccine Fluenz Tetra®, which contains live attenuated vaccine virus. In the days after vaccination, the vaccine virus will replicate in the nasal mucosa. Vaccine virus usually does not cause influenza illness and normally does not transmit from the vaccinated person to others. Even so, in connection with diagnostic work up of a vaccinated child, the treating physicians must be aware that vaccine virus may be detected by a diagnostic test, i.e. yield a false-positive test result. The influenza vaccine contains influenza A as well as influenza B virus. Therefore, in some cases, the test result will be a false positive for both types of virus. Furthermore, the sample may test positive to one type of virus only.
Despite the low risk of transmitting the infection from a vaccinated child, we recommend not using the vaccine in immunocompromised persons and their household contacts, as previously stated in EPI-NEWS.
Most children will not experience any side effects following vaccination with Fluenz Tetra®, but side effects may occur. As described in the vaccine’s summary of product characteristics, the most frequent side effects are reduced appetite, malaise and nasal congestion, whereas the less frequent side effects are headache, fever and muscle aches. In some cases, these symptoms may resemble influenza and may therefore trigger influenza diagnostics.
When a need arises for specific vaccine virus work up, sample material may be submitted to the SSI Influenza Laboratory, where virus sequencing analysis may determine if vaccine virus is in play. Completing this analysis, typically takes a few days.
(R. Trebbien, Department for Virus and Microbiological Special Diagnostics, L.S. Vestergaard, Department of Infectious Disease Epidemiology and Prevention)
Botulism
Botulism is a rare disease caused by the spore-forming Clostridium botulinum bacterium. The bacterium forms a toxin that destroys the nerve terminals, thereby paralysing the muscles of the body, including the muscle function of the chest cavity. The paralyses may be prevented by employing an antidote, but once paralysis has occurred, it may be healed only by leaving the nerve cell to form a new nerve terminal, which may take months. Three forms of botulism exist: food-borne botulism, infant botulism and wound botulism.
In foodborne botulism, symptoms are typically due to ingestion of botulinum toxin that propagate in tainted foods - often in home-preserved/fermented fruits and vegetables. Ingestion of the bacterium itself is often associated with contaminated honey, fish or vegetables. Primary ingestion of the bacterium spores is seen in infant botulism, whereas intestinal colonisation is only rarely seen in larger children and adults.
In wound botulism, the bacterium occurs in wounds where the toxin is produced and passed on (mainly in drug users). This form is rare in Denmark, and no cases have been recorded in the past 30 years.
No vaccine is available to counter botulism. On clinical suspicion of botulism, a botulinum antitoxin that reduces mortality is given.
Botulism 2011-2021
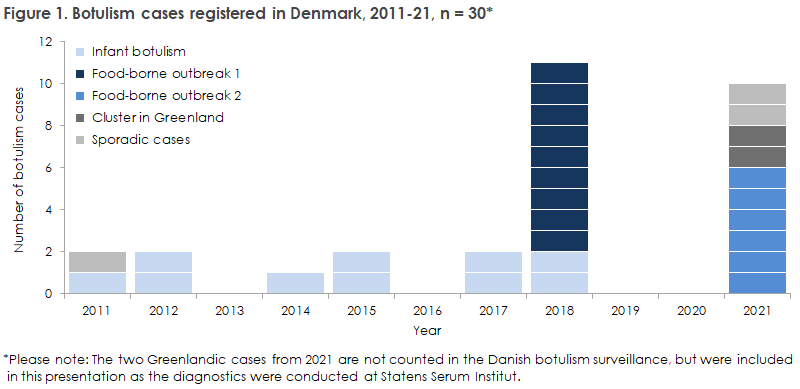
From 2011 onwards, a total of 28 cases of botulism were recorded in Denmark, including ten cases of infant botulism, Figure 1. Six of the ten infant botulism cases are described in EPI-NEWS 5/13 and EPI-NEWS 17/15, respectively.
In July 2011, a young man was admitted to hospital with botulism. The investigation showed that he had probably become infected from a single contaminated jar of tofu, EPI-NEWS 34b/11.
In June 2018, a total of nine cases of food-borne infection were notified as part of the first food-borne outbreak ever recorded in Denmark, EPI-NEWS 25/18. Despite rapid suspicion of botulism and a quick response from the clinicians at Sønderborg Hospital, a total of six persons fell seriously ill and required prolonged admission to hospital, including artificial respiratory support. All patients survived the infection. Tracking of the source of infection was conducted in collaboration with the Danish Veterinary and Food Administration and DTU Food and revealed that the outbreak was caused by a home-made jelly rim with shrimp and lumpfish roe. Botulinum toxin type A was found in the leftovers.
Ten botulism cases in the first half of 2021
In January 2021, a woman was admitted to hospital and subsequently died following severe botulism poisoning. The woman was of Asian origin, and it was suspected that she fell ill due to home-fermented fish or cabbage.
In March 2021, an unusual time-limited cluster of botulism cases was observed with three independent events counting two, one and six cases, respectively. At all three events, Statens Serum Institut was able to detect the infection, either via PCR or via the so-called mouse test. During the mouse test, serum from the patient is injected into mice that are then tested for botulism.
The first samples were submitted for testing at the SSI from Greenland. The samples were from two male family members. Both samples tested positive for botulism. One of the two men died. The two men had probably become infected after ingesting seal meat that had been stored inappropriately in a plastic bag (anaerobic environment). Botulinum toxin E was detected in the seal meat.
The individual case was a man who was admitted to hospital in early March with paralysis of the eye muscles, ptosis, difficulty swallowing, fixed, dilated pupils and slightly impaired speech. He tested positive for botulism by the mouse test. The man was of Rumanian origin and had arrived in Denmark shortly before symptom onset. The man had reportedly become infected at a large dinner arrangement in Rumania where another person also developed similar symptoms.
Concurrently with this investigation, a report was received on a possibly food-borne botulism outbreak in Denmark. Please see the description below.
Outbreak in Denmark following ingestion of contaminated lumpfish roe
In the beginning of March 2021, six family members met for dinner. Five of the six family members were subsequently admitted to hospital with botulism symptoms.
The dinner included a fish dish with fish fillets, shrimp and tuna mousse with lumpfish roe. Botulinum toxin type A was detected in an open jar of red lumpfish roe used at the dinner party.
Trace-back investigation conducted by the Danish Veterinary and Food Administration revealed that the lumpfish roe was of the same type and had been sold by the same manufacturer as the ingredient in the jelly rim that caused the 2018 outbreak. The batch of red lumpfish roe in question was withdrawn from the Danish market on 19 March 2021.
The clinical picture
The symptoms vary depending on the type of botulism, but typical symptoms include symmetrical cranial nerve affection (most frequently causing blurred vision, double vision and difficulty swallowing and muscular paralysis spreading sub-acutely downwards (descending pareses).
Overall, the primary findings are:
- absence of fever
- symmetrical muscular weakness/flaccid paralysis (neurological manifestations)
- frequently respiratory fatigue and need for mechanical ventilation
- the patient is awake and lucid
- normal heart rhythm
- no sensory deficit
- normal spinal fluid biochemistry
For readers with special interest in the topic, the clinical disease courses of the six patients of the March 2021 outbreak are described below:
Patient 1
A middle-aged male awoke 1½ day after a dinner party (see above) with symptoms in the form of double vision, droopy eyelid and postural instability. One day later, he also presented with a feeling of difficulty swallowing and difficulty speaking clearly. The patient described that he felt a sense of heaviness in his lower extremities, but not reduced power per se. No respiratory discomfort. Initially, the man was examined for for apoplexy. At the physical examination, bilateral ptosis and bilateral peripheral facial palsy were detected along with slightly wide-based walking. Normal muscle strength. Opthalmological examination showed discrete bilateral abducens paralysis, no papilloedema. A lumbar puncture showed increased initial pressure, spinal fluid was without pleocytosis, but with slightly increased protein.
During the patient’s second admission day, information was provided that more persons who had attended the dinner party were presenting with similar symptoms, why the suspicion of botulism was raised. The patient was therefore given botulinum antitoxin, and a nerve conduction velocity test detected neuromuscular transmission defect, which underpinned the diagnosis of botulism. Blood and faeces were sent for botulism testing, and botulism was detected by the mouse test and by PCR toxin testing in faeces, whereas culture was negative.
During the initial days of his admission, the patient’s symptoms progressed slightly and he needed a nasogastric tube due to difficulty swallowing. He was monitored with frequent peak flow measurements and his respiration remained unaffected. The patient initiated pyridostigmine (acetylcholinesterase inhibitor) treatment on his seventh admission day and noted improvements in his condition the day after.
The patient was discharged for outpatient follow-up after ten days in hospital. At discharge, he still had light symptoms in the form of double vision and slight dysphagia, but he was able to ingest food and liquids without the use of a tube. Current status eight months after the infection is that the patient is still unwell, he is quickly fatigued and remains unable to hold full-time employment.
Patient 2
An elderly woman who also awoke 1½ day after the dinner party with double vision and dizziness. The symptoms progressed in the course of the next days and the woman additionally presented with difficulty swallowing and a feeling of excessive discharge in the throat. Due to the suspicion of botulism in Patient 1, Patient 2 was contacted by phone on her fourth day with symptoms. The patient then informed that as from earlier that day she had experienced difficulty breathing when in the upright position, a symptom that improved when lying in a dorsal position. The patient was admitted acutely to an intensive care unit for observation.
The physical examination showed speech dyspnoea, bilateral ptosis, double vision, free eye movements, dysarthria and dysphagia. The patient’s lung capacity was reduced with reduced peak flow. The next days, the patient’s lung function improved gradually and she did not need ventilatory support. Blood and faeces were submitted for botulism testing. A mouse test was positive, whereas culture and PCR toxin test in faeces were negative.
The patient was given botulinum antitoxin on the day of her admission and noted improvement the next day. On the fifth day of admission, treatment with pyridostigmine was initiated with good effect and improvement the next day. The patient was discharged in overall improvement after eight days, but she was still affected by slight double vision and general fatigue. Furthermore, the patient had a harsh, deep voice during the entire disease course. Only nearly eight months after her infection is the patient now returning to her usual condition.
Patient 3
An elderly man who had also attended the dinner party presented with symptoms at the same time as the other patients, primarily with double vision and ensuing dizziness. He presented with difficulty swallowing and problems chewing his food, but not with respiratory difficulty at the time of his admission three days after symptom onset.
The physical examination showed discrete ptosis and facial palsy and slight palsy during shoulder abduction, but otherwise normal muscle strength. His speech was dysarthic. Blood and faeces samples from the patient were submitted and tested positive for botulism by the mouse test, whereas faeces was culture negative as was the PCR toxin test.
The patient was given botulinum antitoxin on the day of the admission, felt a slight aggravation of his symptoms the day after but then improvement during the subsequent days. He was discharged after five days, and pyridostigmine treatment was initiated on the day of the discharge. Eight months after his infection, the patient still suffers from fatigue.
Patient 4
A middle-aged woman was admitted on suspicion of botulism as several family members also attending the dinner party had developed similar symptoms. She was admitted two days after the dinner party due to difficulty focusing her eyesight. The patient did not have double vision or other complaints. During the admission, the patient was completely stable with no further symptom progression.
Faeces and blood were submitted for botulinum toxin testing at the SSI, and both tested negative.
The patient was discharged after two days. At discharge, she was completely back to her habitual state, and she was affected only by minor difficulties focusing. She was otherwise neurologically intact. Status eight months after her infection is that the patient remains very fatigued.
Patient 5
An elderly male was admitted on suspicion of botulism two days after the dinner party based on blurred vision, particularly at a distance, and because several of his family members had experienced similar symptoms after having attended the dinner party.
During his admission, the patient experienced a stable course with slight improvement in his double vision and no aggravation or newly presenting symptoms. Faeces and blood were submitted for botulinum antitoxin testing at the SSI and were negative. During his admission, the patient initiated pyridostigmine treatment, which had no effect on his symptoms. The patient was discharged after one day. At discharge, he still experienced double vision but no progression or developments in any other respects. Eight months after discharge, the patient is back to his habitual state.
Patient 6
An elderly woman who had also attended the dinner party initially presented with no symptoms. Subsequently, though, she presented with symptoms in the form of blurred vision and problems focusing and suddenly impaired hearing. Samples were not taken from this patient for botulism diagnostics, and the patient was not admitted to hospital. The patient is back to her habitual state and has regained her hearing.
Commentary
Botulism is a rare infection in Denmark. Sporadic cases are seen at a rate of 0-2 annual cases, and food-borne botulism outbreaks in which several patients become infected simultaneously have been recorded twice in the past 10-year period. As rapid diagnostics and treatment are critical to avoid a serious or fatal disease course, this condition requires preparedness and alertness. The primary diagnosis is made clinically, and it is therefore essential that physicians remain attentive in particular to symmetrical cranial nerve affection with muscular paralysis and respiratory fatigue, as described above. In particular cases in which several patients develop these symptoms after sharing a meal, suspicion of foodborne botulism should be raised.
Assessment of indication for antitoxin treatment is made in consultation with the SSI’s 24-hour manned service of the Department of Infectious Disease Epidemiology and Prevention on phone +45 4131 7404, who can also hand out the antitoxin within the service’s opening hours. Suspected cases should be notified immediately to the Danish Patient Safety Authority and subsequently in writing on Form 1515 or electronically, EPI-NEWS 39/21.
(T. Fabricius, Department of Infectious Medicine, Odense University Hospital, M. Itani, Department of Neurology, Odense University Hospital, C. Stenør, Department of Neurology, Herlev University Hospital, H.C. Florian Sørensen, Tasiilaq Hospital, K. Fuursted, Bacteria, Parasites and Fungi, A. Koch, A. Kjerulf, L. Müller, P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention)
Participate in a European conference on infectious disease epidemiology
Once again, 16-19 November 2021 will see the celebration of The European Scientific Conference on Applied Infectious Disease Epidemiology (ESCAIDE), which is the leading European scientific conference on applied infectious disease epidemiology. Among others, the programme includes communicating science during an evolving pandemic, modelling epidemics, antimicrobial resistance and outbreaks. The conference is targeted at epidemiologists, veterinarians, microbiologists, clinicians, modellers, statisticians, politicians and others working in fields related to applied epidemiology.
This is a virtual conference and participation is free of charge. Deadline for sign-up is 12 November. For more information about the conference and to sign up, please see here.
(Department of Infectious Disease Epidemiology and Prevention)