No 18 - 2021
Legionnaires' disease in Denmark 2020
Legionnaires' disease in Denmark 2020
In 2020, 278 cases of Legionnaires' disease (LD), a serious form of pneumonia, were recorded, including 165 men (26-96 years) and 113 women (25-99 years). The mortality rate was 14%, which is a slightly higher level than previously recorded (around 10%).
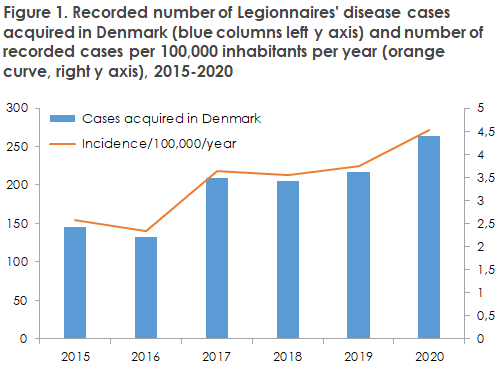
A total of 263 cases (95%) were probably infected in Denmark. This is a 25% increase compared with the mean number of cases registered in the past three years, Figure 1, and the highest number ever recorded.
For a detailed description, please see the 2020 annual report on Legionnaires’ disease in Denmark.
Only 15 cases (5.4%) were probably infected while traveling abroad: nine in Europe, five in Asia and one on the American continent. The proportion of travel-related cases is normally 20-25%.
The increase in the number of people infected in Denmark may be due to a higher test activity in 2020, which, in turn, may have been due to the fact that many admitted patients suspected of COVID-19 were also tested for legionella infection; see the annual report for a detailed description.
A relatively low overall male/female ratio of 1.5:1 and the higher-than-normal mortality rate observed in 2020 may be associated with the few travel-associated cases seen in 2020.
The male/female ratio for travel-associated LD is generally around 2.5:1, whereas the ratio for people who have become infected in Denmark is lower (1.5:1). Similarly, the mortality rate for travel-associated cases is lower (<5%) than the corresponding rate for non-travel-associated cases.
Legionella species diagnostics
Legionella species PCR is an important method for detection of legionellosis/Legionnaires’ disease. Legionella non-pneumophila species occur in the vast majority of water systems (up to 100%) and often in higher numbers than L. pneumophila, but most of the species cannot be cultured. Thus, cultures underestimate the real number of Legionella and legionella-like organisms (LLO) in environmental samples. The vast majority of these species have a very low or no infectiousness in humans, but the fact that they are very common produces a risk of “false” positive PCR results, particularly in patients who undergo upper airway sampling.
Therefore, it is recommended to always do a PCR for L. spp as well as L. pneumophila upon suspicion of legionella infection. If a result is positive for L. spp only, the analysis should be repeated to confirm the result.
In 2020, 254 of the 278 recorded cases were positive to LD by legionella PCR. Among these, 35 were recorded as positive for Legionella spp. only.
Furthermore, an additional 18 cases were registered as positive for L. spp. only and non-pneumonic. These cases were therefore assessed as not having LD.
Among the 53 samples from patients in whom only L. spp. was detected, Statens Serum Institut received 29 for repeat PCR and culture. For some of the patients, an L. pneumophila urine test (LUT) was also performed.
The results from the 53 samples are presented in Table 1.
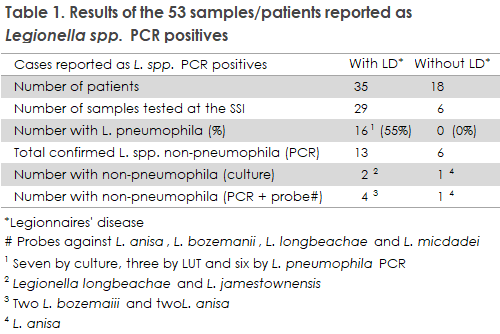
At least 16 of the 35 cases with pneumonia had an L. pneumophila infection and of the remaining 19 patients, 13 were confirmed as L. spp. non-pneumophila infection. Thus, the proportion of L. spp. non-pneumophila infections among all LD cases in 2020 was between 4.6% and 6.1%.
Eighteen patients with a positive L. spp. were considered not to have had LD, including one patient from whom L. anisa was isolated by culture. L. anisa is the second most frequent legionella species (following L. pneumophila) isolated by culture from environmental samples, and the frequency of samples with L. anisa is increasing. This species may cause both Legionnaires' disease and Pontiac fever, but as demonstrated above, the species may also be detected in patients who are free of classic symptoms and in whom the condition therefore cannot be verified clinically.
(S. Uldum, Bacteria, Parasites & Fungi, C. Kjelsø, Department of Infectious Disease Epidemiology and Prevention)