No 49/50 - 2020
Effect of the HPV vaccine on invasive cervical cancer and an update on the Danish HPV vaccination programme
Effect of the HPV vaccine on invasive cervical cancer and an update on the Danish HPV vaccination programme
The largest study conducted to date demonstrates that HPV vaccination effectively prevents cervical cancer and that an early intervention makes the biggest difference.
Researchers from Karolinska Instituttet and Lund University (Lei et al., 2020), among others, have used Swedish register data to compare the risk of developing invasive cervical cancer in girls and women who have received a minimum of one four-valent HPV vaccination to the risk among girls and women who have not received any HPV vaccination. The study includes more than 1.5 million Swedish girls and women aged 10 to 30 years, who were followed from 2006 to 2017.
It has previously been shown that HPV vaccination provides superior protection against genital warts and cervical cell changes when given at a young age – the new study confirms that this is also the case for protection against cervical cancer. Lei et al. have shown that the risk of cervical cancer declines by 88% if girls are vaccinated before they turn 17 years old, by 64% if they are vaccinated before turning 20 years old and by 62% if women are vaccinated before they are 30 years old. Thus, the cumulative incidence for cervical cancer cases was 47 per 100,000 vaccinees and 94 per 100,000 non-vacinees. The researchers adjusted their analyses to account for various factors that may affect vaccine uptake and risk of developing cervical cancer, such as cervical cell changes and other types of cancer than cervical cancer in the mother. The protective effect of vaccination confirms previous studies from Finland (Luostarinen et al., 2017), which recorded a vaccine efficacy of up to 100% (95% confidence interval: 16-100%), and the US (Fangjian et al., 2018) where the cervical cancer incidence was observed to decline following the introduction of a HPV vaccination programme. The study by Lei et al. is the largest study so far to show a protective effect against cervical cancer, and not just precursors to cervical cancer.
Normally, chronic HPV infection takes up to 20 years to develop into cervical cancer. Therefore, the 11-year follow-up period of the study is relatively short. Despite this, the researchers found significant protection from cervical cancer in the vaccinated compared with non-vaccinated girls and women.
HPV vaccination in Denmark
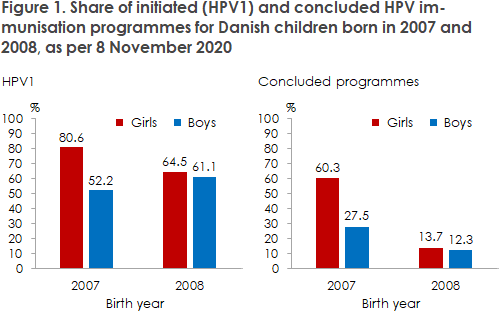
In Denmark, boys and girls are offered a full HPV vaccination programme when they are 12 years old, as protection against cervical and anal cancer, among others. As per 8 November 2020, the share of initiated immunisation programmes (HPV1) for girls in Denmark exceeds 80% for all birth cohorts born between 1997 and 2007 - i.e. the girls who have been vaccinated since the programme became operational in early 2009 (see statistik.ssi.dk). In connection with a crises of confidence in the HPV vaccination programme from 2013 to 2016, the share of vaccinees declined for several cohorts, and in particular for girls born in 2003 and 2004. It is therefore encouraging to see that coverage has reached the level recorded among the birth cohorts preceding the crisis. In the 2008 birth cohort, who will turn 12 years during 2020, 64.5% had received the initial HPV vaccination (HPV1) as per 8 November 2020, see Figure 1. Not everyone in this birth year have received two HPV vaccinations yet and thereby concluded their immunisation programme.
Figure 1 also shows the vaccination coverage of boys born in 2007 and 2008. For the birth cohort of 2007, the vaccination programme only includes boys born after 1 July 2007, whereas those born in the first half of 2007 are covered by a catch-up programme. It is clear that for this birth year, the vaccination coverage is somewhat lower than that of girls, both for initiated and concluded immunisation programmes. The current cohort of 12-year-olds (born in 2008) is the first full birth year of boys to be covered by the childhood vaccination programme, and here the observed vaccination coverage is now largely in line with that of the girls from the same birth year. Thus, it seems that the recommendation to vaccinate has been well received by boys and their parents. The share of completed vaccination programmes is low because a minimum of five months must pass between the HPV1 and HPV2 vaccination, and so the majority of the children born in 2008 are still midway in their immunization programme.
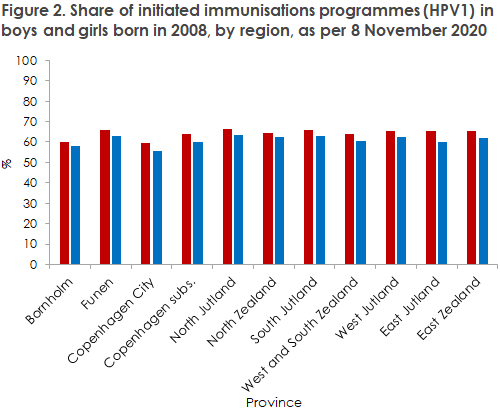
Looking at vaccination coverage by province, the same trend is seen among girls and boys for the birth year 2008, see Figure 2. For both sexes, the City of Copenhagen has the lowest coverage; 59% for girls and 56% for boys. The highest vaccination coverage is seen in North Jutland, where 67% of the girls and 64% of the boys have been vaccinated. The low vaccination coverage in the City of Copenhagen is not a new phenomenon – this trend is also seen among girls if we go further back in time (see statistik.ssi.dk). We are still some way away from the goal of 95% coverage, but the fact that the boys are now also accepting vaccination increases community immunity and indirectly contributes to protect unvaccinated persons of both sexes.
(K. Finderup Nielsen, P. Valentiner-Branth, Department of Infectious Disease Epidemiology and Prevention)