No 47 - 2019
Prevent simple cystitis - and avoid antibiotics
Acute and Chronic hepatitis B 2018
"Prevent simple cystitis - and avoid antibiotics"
This is the headline for this year’s national antibiotics campaign, which recently kicked off.
On 18 November, once again the European Antibiotic Awareness Day took place, an annual event that has been celebrated since 2009.
Denmark has participated in the Antibiotic Awareness Day since 2013 with campaigns aimed at GP’s and their patients, focusing on the main simple infections that are attained in general practice. Conditions like ear pain, sinusitis, cough and other common infections, where a better understanding can contribute to a more rational use of antibiotics and bring down the overall consumption.
This year, SSI and collaborating partners - the Danish Ministry of Health, the Danish Medical Association, the Danish College of Medical Practitioners and the Danish Health Authority, among others - decided to focus on how women may prevent bladder infections - thereby avoiding antibiotics; this year’s campaign also mainly targets citizens.
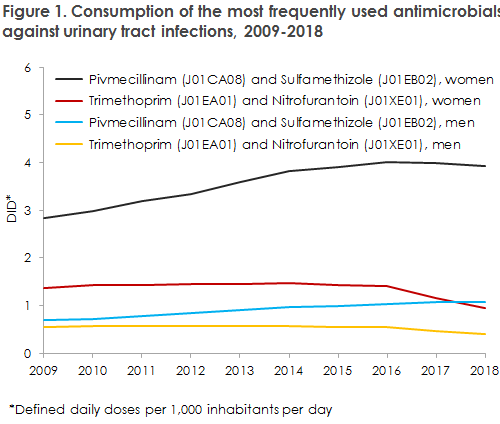
The target group of the campaign is women aged 60+ years who are at an increased risk of being affected by cystitis. From the Danish monitoring of the consumption of antibiotics and from Danish studies, it is known that consumption of antibiotics used for urinary tract infections (UTI) - pivmecillinam, sulfamethizole, trimethoprim and nitrofurantoin - increased until 2016, but is now following a declining trend. The objective of the campaign is to support and strengthen this positive trend.
The target group of the campaign is women, as approximately three of four prescriptions on all antibiotics are issued to women. For antibiotics against UTI, the difference between the sexes is even larger, and widening; in 2018, as many as 4 out of every 5 prescriptions were issued to women. In 2018, a total of 412,065 persons were treated with antibiotics primarily or exclusively used for UTI. Of these, 339,395 were women, accounting for 82% of the prescriptions. See figure 1.
In 2018, an average of 111 prescriptions for urinary tract antibiotics were redeemed per 1,000 Danish citizens, based on reportings from the community pharmacies. Among women aged > 60 years, the corresponding number was 200 per 1,000 inhabitants, whereas the number among men in the same age group was 119. For more information, please see DANMAP 2018.
The campaign messages are consist of three sound and simple advices for the prevention of simple cystitis:
- Drink lots of water and flush away the bacteria
- Take your time when peeing
- Keep clean and dry down below.
Leaflet, poster, website, etc.
Posters and leaflets have been prepared and will be sent out along with the goods ordered by GPs at the SSI in weeks 46-49. If you have not ordered goods for the period, you can still chose to receive an antibiotics campaign package when ordering goods at a later date. In the unlikely event that you do not receive the materials, feel free to write to sha@sum.dk stating ”Antibiotikamateriale” (Antibiotic Material) in the subject field.
As previously, the website www.antibiotikaellerej.dk is an important channel for profiling of the campaign and it is the place to go to read more and see all campaign materials.
The campaign will also come to life on Facebook, where short videos and the three pieces of advice, among others, will be posted.
The poster and leaflet of the 2019 national antibiotic awareness campaign

This year, the European campaign focuses on health workers and their (further) training in the field of antibiotics resistance, rational consumption of antibiotics and prevention of infection. Ahead of the campaign, a questionnaire was sent out that focused on the handling of antibiotics resistance at European hospitals and health centres. A total of 773 Danes participated in the questionnaire.
Results from the study are available at the European campaign’s website. The Danish results demonstrate that the majority of Danish nurses and doctors hold a sound basic knowledge about the use of antibiotics, but only few of them are actively disseminating their knowledge to their patients. Results from the Danish study will be published on the SSI website on antibiotics resistance.
Links to more information
For more information about this year’s national antibiotic awareness campaign, please follow this link:
The antibiotics campaign’s website where you may also offer materials, etc.:
www.antibiotikaellerej.dk
The Danish Antibiotics Council
European Antibiotic Awareness Day
World Antibiotic Awareness Week 2019
For more information about the use of antibiotics and the occurrence of resistance to antibiotics in humans and animals, please see the SSI website and the 2018 DANMAP Report.
(U. Sønksen, the Reference Section for Antimicrobials Resistance, B. Jørgensen, Secretariat of the Management, SSI)
Acute and chronic hepatitis B 2018
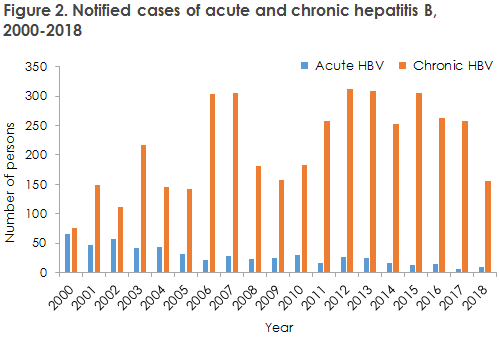
In 2018, the Department of Infectious Epidemiology and Prevention received nine notifications of persons with acute hepatitis B and 155 notifications of persons with chronic hepatitis B.
For a detailed epidemiological description of the 2018 incidence, please see the 2018 annual report on acute and chronic hepatitis B.
Acute hepatitis B
The number of notified cases of acute hepatitis B remains low; see Figure 2. The majority of the cases in this group were sexual transmissions. Even though the hepatitis B incidence is low in Denmark, it remains important to consider vaccination prior to travels to high-endemic countries if it is likely that the traveller will engage in unprotected sex with someone from the area, and if the traveller has a partner from a high-endemic country or is a man who has sex with other men, cf. the Danish Health Authority’s guideline on HIV, hepatitis B and C.
Chronic hepatitis B
The number of persons notified with chronic hepatitis B was somewhat lower than in the preceding years. The number of people notified with chronic hepatitis B reflects a number of factors, including frequency of testing, frequency of notification, immigration and incidence in the countries of origin and the coverage of the childhood vaccination programmes in the countries in question. Denmark is one of the few countries in the world where hepatitis B vaccination does not form part of the childhood vaccination programme offered to all children. On the other hand, Denmark has in place a vaccination programme targeting risk groups. In Denmark, the primary initiative in the prevention of hepatitis B is the general pregnancy screening and risk group vaccination, including IV drug users and men who have sex with men, the latter group only in the Capital Region.
The majority of cases of chronic hepatitis B were immigrants who were infected prior to their arrival to Denmark. More than half were notified as mother-to-child transmissions, and the majority of the remaining cases were notified with unknown mode of transmission.
As many as 45% of those notified with chronic hepatitis B were detected via the general screening of pregnant women. This indicates that many persons residing in Denmark are carriers of chronic hepatitis B, but have yet to be diagnosed and are therefore beyond the reach of any control and treatment, Furthermore, a considerable share of those who have, indeed, been diagnosed with hepatitis B are not notified to the national notification system for infectious diseases (NSID) at the SSI.
Pregnant women and neonates
In 2018, a total of 69 pregnant women were notified with chronic hepatitis B. No children were notified as having been infected at birth in Denmark. Thanks to the screening of pregnant women for hepatitis B, every year sees the detection of a considerable number of asymptomatic carriers who must be referred to a specialist department (infectious medicine or gastro-medicine) for further work-up, control and, if relevant, treatment. This is important, not least because today it is possible to treat pregnant women with a high viral load effectively; these women would otherwise have a considerable risk of inter-uterine infection of their child.
Children born by hepatitis B-positive mothers shall be given immunoglobulin and vaccine at birth (so-called post exposure vaccination) and when they are 1 month (e.g. at the 5-week examination), 2 months and 12 months old to reduce the risk of mother-to-child transmission during labour. When their child is born, parents receive a letter informing them of further steps needed to vaccinate their child. The letter has now been translated into English, Arabic, Farsi and Somali to ensure that all relevant target groups are reached.
In a limited number of cases, post-exposure will not prevent mother-to-child transmission. It is therefore recommended that children born by mothers who have hepatitis B be tested for hepatitis B to determine their status and the vaccination effect 1-2 months after they have concluded their hepatitis B vaccination. A blood sample is taken to test for quantitative anti-HBs (antibodies) and HBsAg (antigen). This is done at the child's GP.
Vaccination recommendations
The Danish Health Authority’s guideline on HIV and hepatitis B and C recommends testing persons from high-endemic countries, regardless of their sex, at their first contact with Danish healthcare. This recommendation includes adoptees. The guideline also recommends vaccination of the following groups:
- Children of HBsAg-positive mothers
- Exposed staff groups
- People sharing a household with hepatitis B carriers
- Children in day-care institutions attended by a pre-school child diagnosed with chronic hepatitis B.
- All residents in institutions for mentally handicapped persons who share household-like conditions with persons who have chronic hepatitis B.
- Persons with Down’s syndrome, including those who live in their own homes.
- Patients with haemophilia
- Patients who are receiving or will be receiving chronic dialysis therapy or who will undergo an organ transplant.
- Patients with HIV or HCV infection.
- Sexual partners to persons with acute or chronic HBV infection.
- Men who have sex with men.
- IV drug users.
Furthermore, we recommend that whenever a person tests positive for hepatitis B, the person’s sexual partner(s) and children should also be tested.
(M. Wessman, S. Cowan, Department of Infectious Epidemiology and Prevention)
20 November 2019