No 27a+b - 2019
Enhanced duty of notification
Vaccines not covered by public Danish healthcare
Annual report on imported malaria 2018
Vaccination recommendations for foreign travel 2019
Enhanced duty of notification
When the HPV vaccine Gardasil®9 is introduced into the childhood vaccination programme for boys, expectedly as per 1 September 2019, the vaccine will once more be placed on the list of medicines with an enhanced duty of notification. Therefore, all presumed adverse effects of the vaccine must be reported by physicians to the Danish Medicines Agency. The current list of medicines with an enhanced duty of notification is available here.
(Danish Medicines Agency)
Vaccines not covered by public Danish healthcare
Statens Serum Institut has prepared a list of the vaccines that are available in Denmark and that do not form part of the publicly financed vaccination programme, but may be given upon personal request. The list consists of an illustration with a timeline and text providing additional information. The wish for a full list was an element in the previous government’s vaccine proposal from October 2018 .
(P.H. Andersen, Department of Infectious Disease Epidemiology and Prevention)
Annual report on imported malaria 2018
In 2018, a total of 64 cases of imported malaria were detected in Denmark.
Figure 1 presents the development in the number of malaria cases imported to Denmark since 1998, by place of infection.
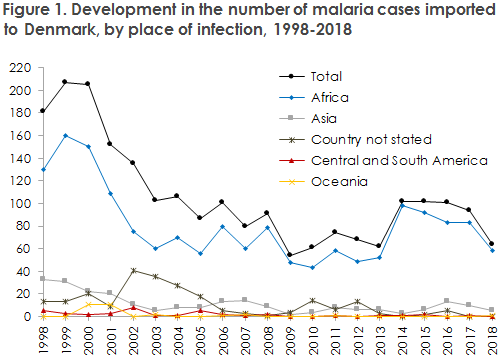
The number of malaria cases imported to Denmark in 2018 was somewhat lower than in the 3-4 preceding years, when approx. 90-100 annual cases were recorded. Many of the cases recorded in the 2014-2016 period were refugees who had arrived from Eritrea/Ethiopia, but in 2017-2018 a drop was recorded in the number of cases from this group, which explains the overall observed decline in cases in 2018.
As previously, the main problem with imported malaria in Denmark is falciparum malaria in persons who have travelled in Africa, both in terms of the number of cases and their severity. As in previous years, malaria constitutes a disproportionately large problem in immigrants, including in their children. There appears to be a need for enhanced efforts to inform this group about the risk of malaria and the importance of using effective prophylaxis during travel, e.g. during long visits to friends and relatives in countries of origin.
Even though the problem of vivax cases in refugees and migrants from Eritrea has declined, in line with the lower number of refugees and migrants arriving to Denmark from Eritrea, treating physicians and other healthcare providers, e.g., Red Cross Centres, still need to be attentive to this group. Children from Eritrea may be infected with vivax malaria but only present with discrete uncharacteristic symptoms or signs of illness.
In 2018, one case of the serious falciparum malaria in a Danish man who returned from Africa ended fatally. The circumstances have yet to be clarified, but the case underlines once more that treating physicians must always be attentive to malaria when the patient has a relevant travel history, even if the patient does not present with “classical” malaria symptoms, such as fever. If a diagnosis has not been made, these patients must be referred to a medical ward for further assessment, observation and treatment.
(L.S. Vestergaard, H.V. Nielsen, Malaria Reference Laboratory, Department of Bacteria, Parasites and Fungi, Department of Infectious Disease Epidemiology and Prevention).
Vaccination recommendations for foreign travel 2019
Statens Serum Institut’s (SSI) reference group for travel vaccination and malaria prophylaxis regularly revises and updates the SSI’s travel vaccination recommendations. This year brings no changes to the annual summary table, EPI-NEWS 27b/19. The WHO’s list of countries with recommendations/requirements for yellow fever vaccination, recommendations for malaria prophylaxis and any other vaccination requirements (e.g., polio) was last updated on 15 November 2018. Only few changes were made to the yellow fever risk areas and no changes were made to the recommendations for malaria prophylaxis. The limited number of changes that were made have been implemented, and the SSI’s travel site has thus been updated.
As described in the malaria report for 2018, the number of imported malaria cases has remained largely stable in recent years, but a decline in cases was seen in 2018. The main problem with malaria is still serious falciparum malaria among travellers to Africa, whereas only very few cases are seen in travellers returning from Asia or South and Central America.
Additionally, a number of other mosquito-transmitted virus infections exist (arbovirus) that are present in many areas across the world and for which no effective prevention is available, apart from careful use of mosquito bite prophylaxis. We describe below some of these infections. For more information about these diseases, please see the SSI website.
In Denmark, it is now possible to buy mosquito repellents containing either the active substance DHIP or DEET. Both types of repellent should contain a minimum of 20% of active substance and may be used by pregnant women. The other important elements in mosquito bite prophylaxis are sleeping under a mosquito net (impregnated, if possible), wearing clothes that minimises the amount of bare skin and spraying an insecticide indoors.
Zika fever
A large global outbreak of Zika virus was recorded in the 2015-2017 period, particularly in South and Central America, the Caribbean, Florida and Texas in the US, and to a more limited extent in Southeast Asia and the Pacific Region.
Zika virus has been known for many years in Africa and Asia. Here, the infection does not produce outbreaks, but sporadic cases occur occasionally. In 2018, eight citizens from EU countries thus became infected by Zika virus while travelling in Southeast Asia, and in 2019 two cases have been recorded among Danish travellers to Thailand. Furthermore, this year, Norway has reported two cases among travellers to Thailand.
The global situation has therefore moved from one of large outbreaks in countries where Zika virus was not previously observed and countries which have historically enjoyed a low and stable level of infection, to a new situation in which both of the previously mentioned types of areas may now expect a low but varying level of Zika virus (endemic occurrence). The SSI has updated its outbreak description for Zika fever and now shows the areas (maps and list of countries) where there may still be a risk of encountering Zika virus.
The European Centre for Disease Prevention and Control (ECDC) has recently updated its risk assessment. On this basis, the SSI has lowered its risk assessment for pregnant women:
The majority of people who become infected with Zika virus do not fall ill, and if you do fall ill, symptoms are typically mild and of brief duration. Even so, becoming infected with Zika virus during pregnancy may produce serious foetal damage, but the exact extent of this risk remains unknown. During the epidemic, the risk was reported as 5-7% during the entire pregnancy, but higher in the first trimester. In the new endemic situation, the risk is generally lower than during outbreaks, and therefore there is no basis for recommending that pregnant women avoid travelling to areas where Zika virus occurs. Even so, a small and varying risk remains, and pregnant women are therefore still recommended to consider postponing any non-necessary travels to countries and areas where Zika virus occurs. Future monitoring data on the real infection risk will determine if there is a basis for further lowering of this cautiousness-motivated risk assessment.
Regardless of your travel destination, pregnant women are encouraged to determine if a risk of infection with mosquito-borne infections exists, and - if this is the case - to protect themselves as well as at all possible against mosquito bites.
For women who have travelled to countries/areas where Zika virus occurs, the Danish Health Authority currently recommends the following precautions:
- Pregnant women who have travelled to areas where Zika virus occurs during their pregnancy, and who - during their journey or less than two weeks after returning - have experienced symptoms consistent with a Zika virus infection, must inform their GP and midwife.
- Women who have travelled in these areas and who are planning to become pregnant are encouraged to wait for 2 months after returning before becoming pregnant.
- Men who return from areas with Zika virus outbreaks and who have a pregnant partner are recommended using a condom for the remainder of her pregnancy.
- Men whose female partner is of child-bearing potential are recommended using a contraceptive (of any type) for three months after returning, regardless of whether the man is experiencing or has experienced Zika fever symptoms or not. (Previously six months)
- Couples who travel together to areas where Zika virus occurs are recommended using contraceptives (of any type) during their stay and for three months after returning home. (Previously six months)
Testing of a pregnant woman is generally only needed if she is presenting with symptoms and has been travelling in a Zika-endemic area. No general recommendations exist that men or women who are not pregnant or who wish to become pregnant should be screened for Zika virus after returning from areas where Zika virus occurs. Diagnostic Zika virus analyses cannot detect or confirm the absence of Zika virus infection in a person. Also, see the Danish Health Authority’s guidelines for healthcare workers on the handling of suspicion of Zika virus infection.
West Nile fever
West Nile fever is caused by infection with West Nile virus, which is transmitted by Culex mosquitoes. West Nile fever is common in Africa, the Middle East, North America and Western Asia. In 2010, West Nile fever was seen for the first time ever in Europe, and since then an increase in the number of cases has been recorded in South Europe. The situation is monitored weekly by the ECDC. In 2018, a record-high number of infected people was recorded, more than 2,000, exceeding the total number of cases registered in the 2011-2017 period. Among others, Greece, Italy, France, Romania and Bulgaria were affected, but human cases were detected as far north as Austria and the Czech Republic. So far, no cases have been detected in 2019, but new cases should be expected to occur in the course of the summer and early autumn, why doctors should be attentive to the diagnosis in patients who have travelled in known and potential new risk areas who present with relevant symptoms. You should be particularly attentive to signs of neuro-invasive disease (approx. 1% of the infected people), which is seen more frequently in the elderly and among immunocompromised people. Culex mosquitoes are also found in Northern Europa and have occasionally been found in Denmark.
Dengue fever
Globally, the incidence of dengue fever has increased over the latest decades, and the disease is now endemic in approximately 130 countries, primarily in tropical and subtropical areas. Many infections are asymptomatic, and the WHO refers to a study estimating that nearly 400 million people become infected annually, of whom approximately 100 million are symptomatic. It is estimated that approximately 1% of the cases are severe (haemorrhagic dengue fever), leading to a high proportion of deaths (1-3%). The risk of infection and severe disease is highest for the local population in endemic areas, particularly during and after the rainy season. Even so, dengue fever infections are occasionally imported to Europe, and apart frm malaria, dengue fever is the most frequent cause of travel-related vector borne disease in Europe. The combination of frequent imported cases and the presence of a competent vector (Aedes albopictus) creates a risk of local outbreaks in Southern Europe, as seen for example on Madeira in 2012-13.
In Cambodia and Laos, for instance, increased dengue activity has been observed in the first half of 2019. Currently, an increase in the number of dengue fever cases is also reported from Thailand - an increase which the local authorities describe as an epidemic. Until mid-June 2019, nearly 30,000 cases and 43 deaths had been reported, which is twice as many as the average recorded for the same period in the preceding five years.
A registered vaccine exists against the condition. The vaccine provides approx. 50% protection, but is not available in Denmark. New follow-up data have shown that unfortunately vaccinated people have a higher risk of complications, including admission to hospital, if they become infected with dengue fever. The WHO has therefore revised the recommendations for use of the vaccine in endemic areas. Importantly, the new dengue vaccine is only recommended to people who have already had dengue fever before. For Danish travelers in general, the most important available protection is careful use of mosquito bite prophylaxis and clothing which reduces the risk of mosquito bites.
Chicungunya fever
Chicungunya virus occurs endemically in Africa, Asia and on the Indian subcontinent. Furthermore, occasional outbreaks of chikungunya fever are seen. A map of areas with risk of chikungunya virus is available here. “Chikungunya” is Maconde (a local Tanzanian language) for "he who bends" and describes the huddled up body posture caused by the intense arthralgia which normally accompanies the acute infection.
In 2007, the transmission of chicungunya virus was reported for the first time ever in Europe in relation to a local outbreak in Northeast Italy, where the primary vector was Aedes albopictus.
In the beginning of 2019, a total of nine cases were imported from Thailand into Sweden, Switzerland, Great Britain, Rumania, Israel and France, respectively. The affected travellers had stayed in Bangkok or in tourist areas on the Malaysian peninsula. It remains uncertain to which extent these travel-related cases reflect an increased infection pressure, but they do show that travelling to popular Asian tourist destinations may be associated with a risk.
No vaccine exists against chicungunya virus infection. Prevention consists in limiting mosquito bites by using a mosquito repellent and other forms of mosquito prophylaxis during stays in endemic areas.
Yellow fever vaccination for Brazil
The past 3-4 years, the yellow fever risk areas in Brazil have expanded, motivating SSI to extend vaccination recommendation to include all travellers to Brazil as from November 2017. 2019 has seen a decreasing number of cases in Brazil overall, but new cases are still reported in previously unaffected areas, and therefore this recommendation remains in place.
Measles
Globally, an increase in the number of measles cases is observed, and the WHO has recently published a warning about the risk for travelers. Despite the increasing number of vaccinated children, in 2018 the WHO’s Europe Region reported more than 82,000 cases, which is approximately three times as many as in 2017 and 15 times as many as reported in 2016. All travelers should have received measles vaccination. Children can be vaccinated as from 9 months of age; in special cases as from 6 months of age (off-label use supported by both the CDC, ECDC and WHO). In Denmark, if the vaccine is given before 12 months of age, it is considered to have been administered outside of the childhood vaccination programme and must therefore be repeated twice later (normally at 15 months and 4 years of age). The costs associated with any extra MMR vaccination due to foreign travel are defrayed by the parents.
Adults who are not immune to measles are vaccinated free of charge regardless of their age, EPI-NEWS 13-14/18. Most persons born before 1974 have had measles and are therefore naturally immune.
(C.S. Larsen, Danish Society of Travel Medicine, S. Thybo, Danish Society for Infectious Disease, J. Kurtzhals, Danish Society for Clinical Microbiology, N.E. Møller, Danish College of General Practitioners, L.S. Vestergaard, Danish Society for Tropical Medicine and International Health, K. Gade, The Danish Paediatric Society, P.H. Andersen, A. Koch, Department of Infectious Disease Epidemiology and Prevention)