No 23 - 2017
MRSA 2016
Measles in Europe
MRSA 2016
The number of persons who had methicillin-resistant Staphylococcus aureus (MRSA) detected for the first time in 2016 increased considerably compared with the number observed in 2015.
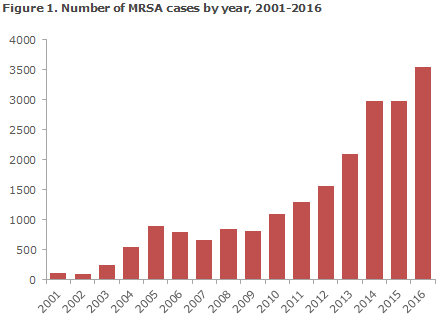
A total of 3,550 cases were recorded in 2016 compared with 2,973 in 2015, Figure 1. This constituted an increase of nearly 20% and is the highest number of newly registered MRSA cases since mandatory notification was introduced on 1 November 2006, EPI-NEWS 44/06. The increase was due mainly to a rising number of imported and community-acquired cases.
Epidemiological classification
Based on presumed mode of infection, MRSA is categorised into the following: acquired abroad, hospital-acquired, community-acquired and livestock-associated. In Denmark, livestock MRSA is nearly always caused by the CC398 MRSA type, which is closely associated with live pigs.
Community-acquired MRSA is further divided according to whether the person has had contact to hospitals or the nursing sector (nursing homes, etc.) within the past 6 months, and if the person has come into contact with a known MRSA-positive person.
Table 1 shows the distribution of notified MRSA cases by presumed mode of transmission.
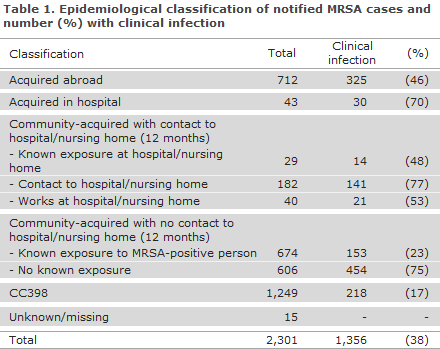
The majority of the MRSA cases were acquired in Denmark (80%), whereas infection abroad was stated in 712 cases (20%) compared with 500 in 2015 (17%). The number of hospital-acquired cases was 43 compared with 40 in 2015, and still comprises only a very limited share of the total number of cases (1.2%). The number of MRSA cases of the CC398 type increased from 1,172 cases in 2015 (39% of all cases) to 1,249 cases in 2016 when it comprised 35% of the total number of cases.
Community-acquired MRSA cases with no contact to hospitals or to the nursing sector comprised 1,280 cases in 2016 (36% of all new cases), which is the same share of the new cases as in 2015 (1,057 cases, 36%). In 674 of these cases (53%), there was known exposure to a person with MRSA, most frequently a member of the household (90%). In hospital-acquired cases, the median age was 61 years (range 0-87 years); and in community-acquired cases with no contact to hospitals or the nursing sector, it was 29 years (0-98 years). The median age for CC398 was 31 years (0-95 years).
Infections
In 1,356 cases (38%), clinical infection was the reason why sampling was performed. In 41 cases, MRSA was isolated from blood, corresponding to 2.1% of all S. aureus bacteraemia cases, which is an increase with respect to last year (29, 1.5%), but a decrease compared with 2014 (2.9%).
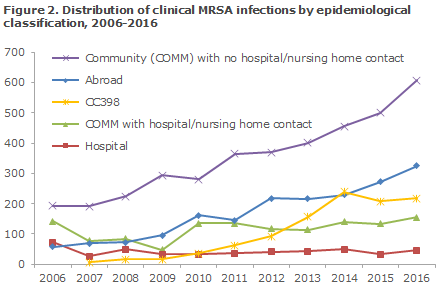
As previously, few hospital-acquired infections were seen (47 in all; 30 patients and 17 hospital staff members), whereas the number of community-acquired infections continued to increase (456 in 2014, 500 in 2015, 607 in 2016), Figure 2. In 153 cases of community-acquired clinical infection, there was known exposure to MRSA, Table 1. The number of community-acquired clinical infections in which there was known contact to a hospital or to the nursing sector within the previous 6 months has remained nearly identical since 2014 (155 in 2016, 133 in 2015, 140 in 2014), Figure 2.
A total of 8 outbreaks counting 56 MRSA cases were identified. The largest outbreak was observed in the Region of Southern Denmark and comprised a total of 36 cases associated with a maternity ward, with a human variant of CC398 (spa type t034, scn and pvl positive). The second-largest outbreak, counting eight cases, started at a residential sports school for young people (spa type t148).
In a total of 673 cases, information on predisposing factors was reported with the primary factors being: ulcers (420), chronic skin conditions (103) and foreign objects such as drains and urinary or IV catheters (77).
Typing and resistance
MRSA of the CC398 type was detected using specific PCR analysis, which also determined if the strain was of the livestock MRSA type or a human variant. Isolates with a characteristic livestock MRSA CC398 profile (96%) were typically not spa typed or tested for resistance.
For isolates with a classic livestock MRSA profile, every tenth isolate was whole-genome sequenced. Resistance determination of 79 isolates confirmed previous findings that CC398 is resistant to tetracycline (95%) and frequently (86%) also to clindamycin. The remaining 2,253 isolates (63%) represented 322 spa types from 26 different clonal complexes (CC groups).
The two major groups, CC22 (n = 357) and CC5 (n = 331), comprised 16% and 15% of the 2,253 isolates, respectively, and represented 31 and 30 different spa types, respectively.
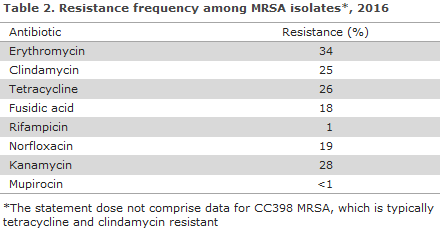
The 10 most frequently observed spa types comprised 52% of the isolates. Hereof, t304 (n = 223; CC8) and t223 (n = 212; CC22) were the most frequently observed. Resistance to non-CC398 MRSA is presented in Table 2.
Livestock MRSA CC398
The number of livestock-MRSA CC398 infections increased in 2016 to 1,249 from 1,173 in 2015. Until 2014, when the largest number of cases was identified (1,276), the number rose considerably, but has since remained stable. In 2016, a total of 218 (17%) had a clinical infection at the time of diagnosis (208, 18% in 2015), Table 1; and 83% of the cases were detected in persons with direct contact to pigs or in persons whose household members had direct contact to pigs.
A total of 209 (17%) persons had no known contact to animals, which is above the level observed in 2015 (140 persons, corresponding to 11%). Among these, 98 had a clinical infection, corresponding to 47% of all detected infections, which is an increase from 2015 (77, 37%). 2016 saw a total of seven cases of livestock MRSA CC398 bacteraemia, including one with a fatal outcome within 30 days. Contact with pigs could not be confirmed for this patient.
Livestock MRSA CC398 has also been recorded in persons with contact to mink, which correlates with MRSA findings in the mink and their fodder. In 2016, contact to mink comprised 26 cases of livestock MRSA CC398, which was an increase compared with 2014 and 2015, where 15 cases were detected annually.
mecC-MRSA
MRSA usually carries the mecA resistance gene, but some carry a variant of the mecA gene called mecC. In 2016, 45 cases (1.3%) were shown to have the mecC-MRSA gene, which is slightly lower than the previous two years: in 2014 (53) and 2015 (61). The type was initially described in 2010, EPI-NEWS 47/12, and has been associated with a wide range of different animal species, particularly cattle and sheep but also wild animals. The source and mode of infection were unknown in the majority of the cases.
Imported MRSA cases
The number of imported MRSA cases rose sharply in 2016, which was due partly to an increase in the number of new MRSA cases among asylum seekers. Asylum seekers were reported separately in 2015 and 2016 as these cases are often from areas with a high MRSA incidence, and in Denmark this group is offered treatment only if the logistic conditions permit.
In 2016, a total of 417 cases of MRSA were detected among asylum seekers. This constitutes an increase compared with 2015 (150). Part of the increase may be attributed to a changed and more thorough recording practice, and the screening activity has probably also increased.
Many of the cases among asylum seekers carried MRSA of the types t304 and t223, which are now the most frequently observed spa types. It is therefore recommended that asylum seekers who live or have lived in asylum centres within the past 6 months are tested for MRSA carrier state when they come into contact with a hospital.
Commentary
The number of new MRSA cases once again increased in 2016 following a stable period in 2015. The increase was due to continued increase in the number of imported and community-acquired cases. Among the imported cases, asylum seekers comprised an increasing share of the cases in 2016. As previously, 2016 recorded a very low incidence of hospital-acquired MRSA, indicating that the national Danish MRSA guidelines are working well.
A slight increase was seen in the number of livestock MRSA CC398 cases, but the share of the total number of MRSA cases nevertheless followed a slightly decreasing trend from 2015 and is at par with the number observed in 2014. This is probably because testing has been performed on a larger share than previously of persons who come into direct contact with pigs. This causes the number of persons at risk of a new infection to decrease. It should be noted that despite the levelling off, it is very likely that the number of healthy carriers will accumulate over time, particularly among carriers of livestock MRSA CC398 with contact to livestock.
This is so because these carriers are not comprised by MRSA treatment programmes. The number of people with livestock MRSA CC398 without known contact with pigs has increased, and more infections are also seen in this group. This trend is expected to increase due to the increasing infection pressure from livestock MRSA CC398. In consequence of the development in livestock MRSA CC398, the 2016 revision of the MRSA guideline introduced that all hospital patients who have come into contact with pigs shall remain isolated until they test negative, and that contact to mink is now also a special risk group.
(A. Petersen, A.R. Larsen, Microbiology and Infection Control, A. Koch; C.H. Møller, L.K. Knudsen, Tinna Urth, Department of Infectious Epidemiology and Prevention)
Measles in Europe
Statens Serum Institut (SSI) currently receives an increasing number of calls from parents who state that their GP has referred them to the SSI for advice about measles prior to travels in Europe and elsewhere.
The SSI still does not provide either written or phone-based advice for private citizens. The GPs are encouraged to stay updated on the current vaccination recommendations, including for travels, at the SSI’s website under News, and in EPI-NEWS.
In 2017, an increased number of cases were detected in various European countries, and non-immune travellers may be at risk when travelling to common tourist destinations. The only effective preventive measure against measles is vaccination with the MMR vaccine, which also protects against mumps and rubella.
In relation to the childhood vaccination programme, it is important to point out that there is no general recommendation to give the first MMR vaccine earlier than at the recommended 15 months of age. If the parents are worried about infection and want to bring forward the time of the first vaccination, the MMR vaccine may be given right away as from 12 months of age. If practical, it may be given at the same time as the other vaccines usually given at this age (DTaP-IPV/HIB and PCV13), and otherwise with any interval relative to these.
If you need to stay in an area that is known to harbour measles outbreaks, the MMR vaccine may be given as from 9 months of age. In special cases, it may be considered to give the vaccine off-label from 6 months of age, see below. In both of these cases, the vaccination must then be repeated at the times recommended in the childhood vaccination programme (at 15 months and 4 years).
The cost of any extra MMR vaccination is defrayed by the parents.
If a neonate has become exposed to infection, the MMR vaccine may be given (off-label) as from 6 months of age, EPI-NEWS 50/15.
This will also lead to a recommendation that the child receives an extra MMR vaccination. As the first MMR vaccine in this situation is given as part of post-exposure prophylaxis (PEP), this vaccination will be covered by the National Danish Health Service (Sygesikringen).
In 2017, Europe has seen a particularly large amount of measles cases in Germany (634 cases, particularly in Nordrein-Westfalen), Italy (2,719 cases in 18 of the 21 regions, but mainly in the regions of Abruzzo, Lazio, Lombardy, Piemonte, Sicily, Toscana and Veneto), Belgium (293 cases in all provinces of Wallonia) and Romania (6,434 cases since the beginning of 2016, particularly in Western Romania). Measles are also still in circulation in many other countries beyond Europe, including Africa and Asia. The American continent was declared free of Measles in September of 2016.
It is the objective to eradicate measles (and rubella) in the WHO Europe Region no later than by 2020. Denmark is expected to achieve status as having eliminated measles during the course of 2017.
(P.H. Andersen, L.K. Knudsen, Department of Infectious Epidemiology and Prevention)
Link to previous issues of EPI-NEWS
7 June 2017