No 28-33 - 2016
Leptospirosis: 2011-2016
SSI vaccine day in Vejle on 13 September 2016
Yellow fewer – outbreak status and updated vaccination requirements
Leptospirosis: 2011-2016
Leptospirosis is a zoonotic condition caused by bacteria of the Leptospira genus. Leptospirosis is commonly occurring in many developing countries, but its incidence is lower in Western Europe. Leptospira spp. are found in many different animal species, but the main reservoir is rodents; particularly mice and rats. Outbreaks are reported regularly; particularly in the tropics/sub-tropics and primarily in the rainy season, EPI-NEWS 02/05 and 34b/11.
The bacteria are secreted with the urine and can cause infection from the urine or contaminated freshwater in case of contact to mucous membranes, minor scratches on the skin or sodden, but seemingly intact skin. Following a 1-2 week incubation period (that may range from 2 to 30 days), the condition typically begins with influenza-like symptoms (fever, headache, myalgia) and often conjunctival erythema. In serious cases (Weil’s disease), vital organ failure is seen after few days and particularly the function of the liver, the kidneys and the coagulation system is affected. The condition may be treated with penicillin or other antibiotics. A human vaccine against leptospirosis does not exist. Clinical leptospirosis is notifiable on Form 1515.
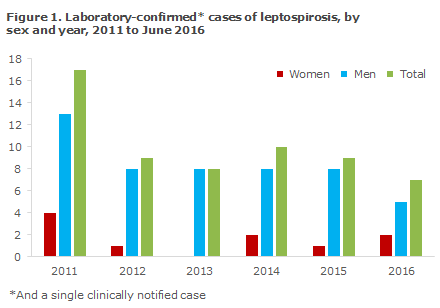
The period from January 2011 to June 2016 saw a total of 60 recorded cases of leptospirosis overall, i.e. notified and/or laboratory-confirmed cases; 10 (17%) women and 50 (83%) men aged 13-70 years with a median age of 44 years, Figure 1. Among the recorded cases, 38 patients aged 13-69 were notified clinically. Among these, 33 (87%) were men aged 16-69 years (median age 44 years). A total of 59 cases were laboratory-confirmed; these included 37 of the 38 clinically notified patients.
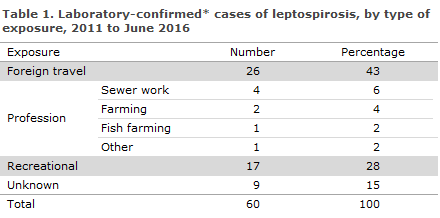
For a total of 25 persons (42%), information was provided about infection in Denmark. Eight of these had occupational exposure, including four following contact to sewage where rats were present and in a total of three cases after direct contact to rats or rat urine, one at a fish farm and two at farms, Table 1. The eights person worked putting up animal fencing outdoors and came into contact with stagnant water.
The persons who were infected in Denmark and had no occupational exposure had most frequently become infected when cleaning their own cellars (six persons), EPI-NEWS 34b/11 and 5/12, and through contact to stream water (five persons) in connection with both intentional and unintentional stays in water. Another four persons had come into more direct contact with rats, either by being bitten or in connection with rat prevention. Additionally, one patient was a hunter and another reported having stood barefoot in sewage.
A total of 26 persons were infected abroad, 16 (61%) of whom had travelled to Asia. Among the persons who were infected outside of Denmark, ten had been exposed to lake water and rivers; and among these, three persons had been infected doing river rafting. Only one person was believed to have become infected from sewage.
For nine persons cerebral symptoms were reported. Two of the 60 patients (one man and one woman) died due to their Leptospira infection.
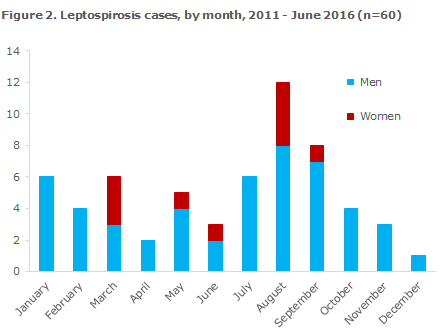
Infection by the Leptospira bacterium is renowned for seasonal variation, which depends on the temperature and on rat population density. As in other years, the majority of leptospirosis cases were seen in late summer and in the autumn, Figure 2, which is when water temperatures peak. The bacterium survives poorly in water below 18 degrees Celsius and does not tolerate drying out.
Leptospira contain both pathogenic and intermediate pathogenic species: L. interrogans is the more frequently occurring species in humans, and more rarely the following are seen: L. borgpetersenii, L. fainei and L. kirschneri. The Leptospira family is also categorised into more than 200 serovars. Only a limited number of serovars are found in more than one Leptospira species.
The bacterium is visible directly upon inspection with dark field microscopy and may be cultured, but these methods have a low specificity and sensitivity. By definition, serology (antibody-testing) is used to determine the Leptospira serovar, and therefore the diagnosis is best made through serology and PCR, which have a considerably higher sensitivity and specificity.
Diagnostics
In Denmark, Statens Serum Institut performs the laboratory diagnostics for leptospirosis. Diagnostics consist of serology (R-343) through micro-agglutination test, MAT testing for 15 Leptospira serovars, PCR for the Leptospira species (R-065), and PCR and culture for Leptospira (R-1350). The recommended materials for PCR are blood, urine or spinal fluid, if possible obtained before the initiation of antibiotic treatment.
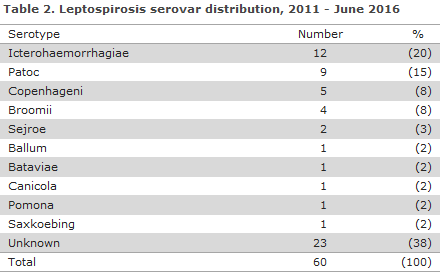
In 38% of cases, the serovar could not be determined. In 15 of these patients, the diagnosis was based on PCR exclusively. An additional seven patient sera yielded too many cross reactions for the serovar to be determined. The most frequently established serovar was L. interrogans serovar Icterohaemorrhagiae (20%), Table 2, which is frequently found naturally in rat urine.
*Including PCR positives and one clinically notified case.
Two patients had Leptospira DNA detected in their spinal fluids, and serology identified Leptospira interrogans of the serovar Sejroe, Table 2. One of these patients recovered, whereas Leptospira DNA was detected in the spinal fluid post mortem in the other case (for a detailed description, see “Case stories”). A total of 46 persons contacted hospitals directly, whereas only six persons were seen by their GP. In eight cases the samples were ordered by private medical companies or by other Scandinavian healthcare facilities.
Case histories: Four recent cases of leptospirosis in persons who were infected in Denmark
1.
A 45-year-old, previously healthy woman was admitted to hospital with influenza-like symptoms (fever, headache, nausea, poor general condition and back-pain radiating into the left hip).
Two weeks prior to the admission, the patient had been bitten by a rat (in her own home on a farm) and two days prior to the admission she had contacted the emergency call physicians due to severe back pain.
At admission her temperature was 39.7 degrees Celsius, her blood pressure was 104/77 mmHg and the heart rate was 132. Paraclinically, the patient had leukocytes 11.4 x 109 /L, CRP 288 mg/L, blood sedimentation rate 51 mm and creatinine 127 μmol/L. A thorax X-ray revealed bilateral pulmonary infiltrates. The clinical physical examination was otherwise normal. The patient was treated with intravenous piperacillin-tazobactam and ciprofloxacin and given intravenous fluids to re-establish the electrolyte balance and blood pressure.
Eight hours after the admission, the patient desaturated to 80% despite maximal oxygenation. Severe pulmonary haemorrhage was observed and shortly thereafter the patient suffered cardiac arrest and died. The diagnosis of leptospirosis was made post mortem using PCR on urine, blood from blood culture tubes and on spinal fluids.
2.
A middle-aged man who resided on his own farm with pig farming and agriculture initially contacted the emergency call physician following four days with influenza-like symptoms. Three days hereafter the patient contacted his GP who observed a heavily increased CRP and admitted the patient for further work up. The patient had no skin conditions or major wounds in the period leading up to the symptoms, but may have had minor scratches caused by the farm work.
In the period leading up to symptom onset, he had been cleaning the stables and slurry store with a high-pressure flusher and he had replaced the farm’s rat traps. During this work he wore rain wear and rubber boots, but he did not use gloves. Laboratory tests detected Leptospira DNA in both his urine and spinal fluid and positive serology with finding of Leptospira interrogans serovar Sejroe. This serovar is primarily seen in mice and horses. The patient recovered fully.
3.
A middle-aged man who worked in pig pens and with previously diagnosed psoriasis on the shins, but no recollection of current wounds/scratches on his arms or hands, was admitted following four days with nausea, vomiting, fever, dizziness and with increasingly sparse urination. At admission his liver and kidney counts were affected and relevant antibiotic treatment was initiated.
This treatment also covered Leptospira. Laboratory tests of urine were PCR positive and returned a positive serology with finding of Leptospira interrogans serovar Sejroe. Before symptom onset, the patient had been feeding, cleaning and minding his livestock and he had been getting straw from a stock where rats had been seen shortly before and rodent control had been performed. While working, he used disposable gloves, rubber boots and coveralls, but he never wore a mask.
It could not be excluded that the patient had had an infection focus in the skin in relation to his psoriasis, nor could it be excluded that he had touched straw from the stock and then dried his face around the eyes, nose and mouth. The patient recovered, and the case was subsequently reported as an occupational accident.
4.
A young man was admitted with headache, a high fever and increasing CRP. Previously that month (eight days prior to symptom onset), he had participated in a swim-run event in Denmark. During his admission, the patient was - among others - treated with Meropenem. The patient was PCR positive for Leptospira in the urine. The patient had no skin conditions or large wounds at any time during the incubation period, but he possibly acquired minor scratches during the 6-hour-long swim-run event where he swam and ran through streams and stubble fields wearing running shoes and a short-sleeved (arms and legs) swimsuit after which he was only able to bathe and change into other clothes later in the evening. The patient recovered without sequelae.
Prevention
Protection with rubber boots and gloves is recommended for any contact with sewage and for other relevant exposures, e.g. at farms, EPI-NEWS 34b/11. Contact between the hands and the mouth (smoking, eating, etc.) should be avoided during exposure, and thorough hand hygiene is mandatory after concluding the tasks in question, EPI-NEWS 5/12. Furthermore, rat control must be implemented in the locations (farms) where there is suspicion that animals may have become infected with Leptospira (pigs that miscarry, humans who become infected).
At the Danish Veterinary and Food Administration's website, a guideline on rat control in food-producing companies and farms is available, and the Danish Working Environment Authority has published guidelines on work with water.
During travels abroad, direct contact to freshwater should be avoided by anyone whose skin barrier is not intact (due to scratches, small wounds).
Commentary
The number of patients who were infected with leptospirosis in the period from January 2011 to June 2016 - a total of 60 persons - was considerably higher than the number recorded in the corresponding period from 2005-2010, when a total of 42 cases were registered, EPI-NEWS 34b/11. Only about half of the cases recorded in the entire period were notified on Form 1515. The majority of the cases were reported in 2011, including five cases associated with the summer 2011 rainstorm, EPI-NEWS 5/12.
The infection course with Leptospira from the blood stream to secretion in the urine and subsequent development of antibodies means that both laboratory methods (serology and PCR) may be needed to increase diagnostic sensitivity and specificity. It is remarkable that the number of persons who were presumably infected through farms or due to contact to sewage or freshwater in the period from January 2011 to June 2016 exceeded the number of people presumably infected at fish farms. Leptospirosis in pigs in Denmark is described by the Knowledge Centre for Agriculture.
(R. Datcu, Microbiological Diagnostics and Virology, C. Kjelsø, Department of Infectious Disease Epidemiology, M. M. Søndergaard, Department of Medicine, Svendborg Hospital, K. A. Krogfelt, Microbiology and Infection Control)
SSI vaccine day in Vejle on 13 September 2016
Now for the third time, the SSI invites GPs and practice staff with a healthcare background related to vaccines and vaccination to attend an instructive and educational day focusing on the childhood vaccination programme. The day will comprise sessions offered by the Department of Infectious Disease Epidemiology and the Danish Health Authority, among others, and there will be ample opportunity to ask questions and share experiences from clinical practice. This year, the venue of the Vaccine Day is Munkebjerg Hotel in Vejle.
See the programme and learn how to sign up (in Danish).
(Department of Infectious Disease Epidemiology)
Yellow fewer – outbreak status and updated vaccination requirements
Epidemiological status
Yellow fever outbreaks are still ongoing in some African countries, EPI-NEWS 21/16.
Angola has seen no new cases in July or August. Up to 4 August 2016, a total of 3,867 suspected cases had been recorded of which 879 were laboratory-confirmed. A total of 269 persons had died, including 119 of the confirmed cases. Massive vaccination campaigns have already been implemented in most of the country, and an additional vaccination effort targeting 3 million people in 18 districts was initiated on 15 August.
In the Democratic Republic of the Congo (DRC), a total of 2,269 suspected cases had been recorded by 8 August 2016, among which 74 cases had been confirmed out of 1,943 tested patient specimens. Among the 74 confirmed cases, 16 fatalities were recorded. The confirmed cases were recorded in seven of 26 provinces and 56 of the cases were imported from Angola. The outbreak is not yet under control, and vaccination campaigns were initiated on 17 August in 32 healthcare districts in the Kinshasa Province and in the 16 healthcare districts that border on Angola. Due to lack of vaccines, the vaccination efforts in the Kinshasa Province will consist in splitting the individual vaccines into lower-than-normal doses.
In Uganda, a yellow fewer outbreak started in March 2016, EPI-NEWS 21/16, but the outbreak does not form part of the main outbreak in Angola and the DRC. In the period from 26 March to 8 June, a total of 91 cases were recorded, including seven fatalities. Seven cases were laboratory-confirmed. There are no current updates from the WHO about the outbreak, and it therefore remains unknown if the outbreak has concluded or if new cases are still being recorded.
Kenya saw two new cases from Angola in March, but there is no information about any new cases of infection in the country.
Updated vaccination requirements
The general recommendations and requirements on yellow fewer vaccination presented in EPI-NEWS 21/16 remain in place. Additionally, on 25 July 2016 the WHO stated that some countries have temporarily introduced enhanced requirements for travellers relating to yellow fewer vaccination:
Uganda: All travellers to and from the country must be vaccinated against yellow fever, and the vaccination must have been documented using the international vaccination certificate.
Rwanda: All travellers to the country who come from yellow-fewer-endemic areas or who have visited a country with a current yellow fewer outbreak within the past 24 days may enter the country as normally only if they
- Can produce a valid yellow fewer vaccination certificate
- Do not run a fewer (temperature below 38.5 degrees Celsius)
- Have remained symptom-free for the past six days.
Travellers who run a fever of 38.5 degrees Celsius or above will be allowed to enter only if they agree to isolation and further tests to exclude that they have yellow fever.
Brazil: Until further notice, travellers from Angola and the Dominican Republic of Congo (including transit stays) must hold documentation for yellow fewer vaccination.
(P.H. Andersen, A.H. Christiansen, Department of infectious Disease Epidemiology)
Link to previous issues of EPI-NEWS
17 August 2016