No 23 - 2016
MRSA 2015
MRSA 2015
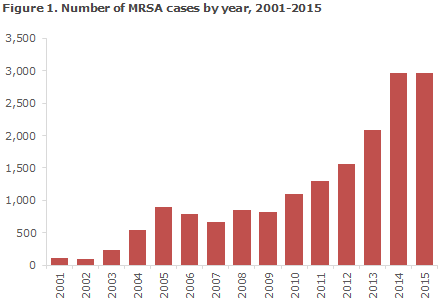
The number of persons who had methicillin-resistant Staphylococcus Aureus (MRSA) detected for the first time in 2015 was nearly identical to the number observed in 2014. A total of 2,971 cases were recorded compared with 2,973 in 2014, Figure 1. This is the first time since 2009 when the SSI recorded 818 new MRSA cases that the number has not increased.
Epidemiological classification
MRSA is categorised based on presumed mode of infection into the following: acquired abroad, hospital-acquired, community-acquired and livestock-associated. In Denmark, livestock-associated MRSA is nearly always caused by the CC398 MRSA type, which is closely associated with live pigs.
Community-acquired MRSA is further divided according to whether the person has had contact to hospitals or the nursing sector (nursing homes, etc.) within the past 6 months, and whether the person has come into contact with a known MRSA-positive person
Table 1 shows the distribution of notified MRSA cases by presumed mode of transmission
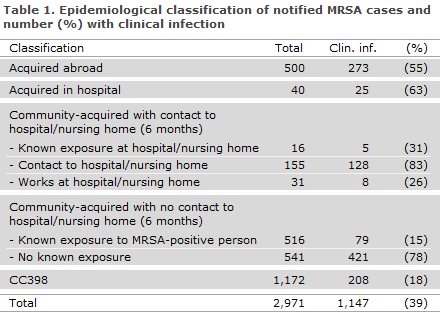
The majority of the MRSA cases were acquired in Denmark (83%), whereas infection acquired abroad was stated in 500 cases (17%) compared with 411 in 2014 (14%). The number of hospital-acquired cases observed in 2015 decreased to 40 from 95 cases in 2014, but still comprises only a very limited share of the total number of cases (1.3%). The number of MRSA cases of the CC398 type decreased from 1,276 cases in 2014 to 1,172 cases in 2015 and comprised 39% of the total number of cases. Community-acquired MRSA cases with no contact to hospitals or to the nursing sector comprised 1,057 cases in 2015 (36% of all new cases) compared with 946 cases in 2014.
In 541 of these cases (51%), there was known exposure to a person with MRSA, most frequently a member of the household (88%).
In hospital-acquired cases, the median age was 49 years (range 0-96 years); and in community-acquired cases with no contact to hospitals or the nursing sector, it was 30 years (0-94 years). The median age for CC398 was 31 years (0-96 years).
Infections
In 1,147 cases (39%), clinical infection was the reason why sampling was performed. In 29 cases, MRSA was isolated from blood, corresponding to 1.5% of all S. aureus bacteraemias, which is a substantial decrease with respect to the previous year (56, 2.9%) and in line with the years before that.
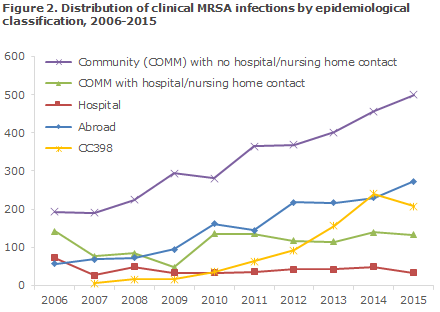
As previously, few hospital-acquired infections were seen (33 in all; 25 patients and 8 hospital staff members), whereas the number of community-acquired infections continued to increase (456 in 2014, 500 in 2015), Figure 2. In 79 cases of community-acquired clinical infection, there was known exposure to an MRSA-positive case, Table 1. The number of community-acquired clinical infections in which there was known contact to a hospital or to the nursing sector within the previous 6 months was in line with the number observed in 2014 (133 in 2015 compared with 140 in 2014), Figure 2.
A total of 14 outbreaks counting 46 MRSA cases were identified. The two largest outbreaks occurred in the Region of Southern Denmark comprising a total of 13 cases (spa type t032 and t2006). Three outbreaks started in neonatal departments (spa type t015, t127 and t304), whereas two outbreaks started at nursing homes (spa type t008 and t034) and three at asylum centres (spa type t044, t2251 and t5100).
The most frequently observed predisposing factors of MRSA were: sores (346), chronic skin disorders (106) and foreign objects, e.g. drains, urinary or IV catheters (53).
Typing and resistance
MRSA of the CC398 type was detected using specific PCR analysis, which also determined if the strain was of the human-adapted type (scn positive). Isolates with a characteristic livestock MRSA profile were typically not spa-typed or tested for resistance. For isolates with a classic livestock MRSA profile, every tenth isolate was whole-genome sequenced. Resistance determination of 68 isolates confirmed previous findings that CC398 is resistant to tetracycline and frequently (> 90%) to clindamycin.
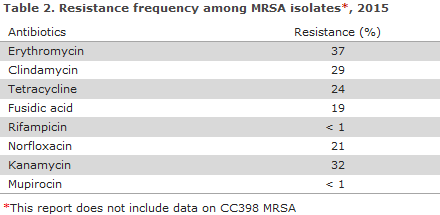
The remaining 1,799 isolates (61%) represented 293 spa types from 26 different clonal complexes (CC groups). The two primary groups, CC5 (n = 302) and CC8 (n = 300) both comprised 17% of the isolates and represented 39 and 26 different spa types, respectively. The 10 most frequently observed spa types comprised 50% of the isolates. Among the types, t002 (n = 173; CC5) and t127 (n = 148; CC1) were the most frequently observed. Resistance for non-CC398 is presented in Table 2.
MRSA CC398
MRSA CC398 decreased in 2015 to 1,172 from 1,276 in 2014. A total of 208 (18%) had a clinical infection at the time of diagnosis (240, 19% in 2014), Table 1; and 88% of the cases were detected in persons with direct contact to pigs or in persons whose household members had direct contact to pigs. A total of 140 (12%) persons had no known contact to animals, which is in line with the level observed in 2014 (137 persons, corresponding to 11%). 2015 saw a total of six cases of MRSA CC398 bacteraemia, including one with a
fatal outcome within 30 days. Contact with pigs could not be confirmed for this patient.
In 2015, a total of 70 cases were recorded in connection with research-related risk-group screening. Adjustment for these cases did not significantly change the percentage occurrence of transmission to persons with no known contact with livestock or the percentage occurrence of infection at the time of diagnosis.
mecC MRSA
MRSA usually carry the mecA resistance gene. In 2015, a total of 61 (2.1%) cases of the mecC MRSA gene, a variant of mecA, were detected compared with 53 cases (1.8%) in 2014. The type was initially described in 2010, EPI-NEWS 47/12, and has been associated with a wide range of different animal species, particularly cattle and sheep, but also wild animals. The source and mode of infection were unknown in the majority of the cases.
Asylum seekers
In 2015, a total of 150 cases of MRSA were detected among asylum seekers. As asylum seekers are often moved between various centres, they are only offered treatment if the logistic conditions allow for this (and if the physical premises at the centre in question facilitate the treatments). It is therefore recommended that asylum seekers who live or have lived in asylum centres within the past 6 months are tested for MRSA carrier state when they come into contact with a hospital.
Commentary
The number of new MRSA cases now seems to level off after several years with substantial increases. It is encouraging that 2015 recorded a slow-down, even though this trend conceals a continued increase in the number of imported and community-acquired cases. A minor decrease in CC398 was observed, which, however, cannot be considered a reflection of a decrease in the number of persons infected. It is more likely that the decrease is due to a greater share of persons who come into contact with pigs being tested.
This causes a decrease in the number of persons who are at risk of first-time infection. It should be noted that despite the levelling off, it is very likely that the number of healthy carriers will accumulate over time, particularly among carriers of CC398 MRSA with contact to livestock. This is so, because healthy carriers with contact to livestock are not comprised by MRSA treatment programmes. It is, nevertheless, remarkable and positive that the number of persons with CC398 with no contact to pigs has not increased. This population is “infinite”, and continued spreading to the community in general would have been recorded if the CC398 infection pressure was increasing. This conclusion is not changed by adjustment for the extraordinary screening test performed in 2015.
In 2014, 2.9% of all S. aureus bacteria were caused by MRSA, whereas in 2015 the corresponding share was 1.5%, which is in line with the years before 2014. The high number of MRSA in blood observed in 2014 therefore seems not to reflect a real increasing trend.
As previous years, 2015 recorded a very low occurrence of hospital-acquired MRSA, indicating that the national Danish MRSA guidelines are working well.
(A. Petersen, A.R. Larsen, R.L. Skov, Microbiology and Infection Control, A. Koch; C.H. Møller, L.K. Knudsen, Department of Infectious Disease Epidemiology)
Link to previous issues of EPI-NEWS
8 June 2016