No 47 - 2014
Uptake in the temporary HPV vaccination programme for females born in 1985-1992
European HIV Testing Week 21-28 November 2014 – Talk HIV. Test HIV.
Uptake in the temporary HPV vaccination programme for females born in 1985-1992
Introduction
From 27 August 2012 to the end of 2013, a temporary free-of-charge human papillomavirus (HPV) vaccination programme for females from the 1985-1992 birth cohorts was in place.
Several studies conducted abroad have found a significant association between ethnic background and HPV vaccine uptake, with a lower uptake among ethnic minority groups. Since Denmark is a country with a relatively large non-Danish population, it is relevant to analyze whether there are ethnic disparities in vaccine uptake in addition to describing the overall uptake of HPV vaccination in the population.
The vaccine given was the 4-valent vaccine Gardasil, marketed in Denmark since October 2006. The vaccine followed a three-dose schedule, EPI-NEWS 28-33/12.
Vaccinations given prior to as well as during the programme were included in this study. Vaccinations given prior to the programme were medically prescribed and subject to payment. In order to determine the uptake, data about HPV vaccinations administered by the end of 2013 were retrieved from the Danish Vaccination Registry (DDV).
This dataset was linked to the Danish Civil Registration System by 27 June 2013 to obtain information about country of birth and time since immigration. Vaccination uptake was determined by counting number of administered vaccinations divided by the number of females eligible for vaccination.
Uptake
Out of a population of 274,154 females born in 1985-1992 identified from the CPR-registry 44,122 (17 %) had received the first dose, 38,253 (14 %) had received the second dose and 31,266 (11 %) had completed the HPV vaccine schedule before the temporary programme came in to place, table 1.
During the programme, 161,819 females (70%) out of 230,032 with no previous HPV vaccination, received the first dose of the HPV vaccine. The second dose coverage was achieved in 151,195 (64 %) out of the 235,901 eligible females, and completion of the HPV vaccine schedule was achieved in 121,997 (50 %) out of the 242,888 eligible females.
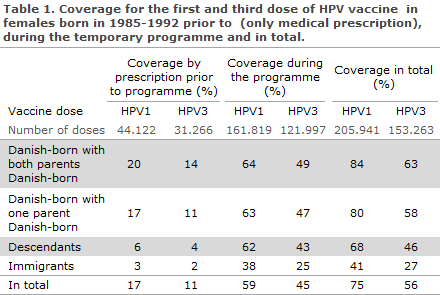
By the end of the programme 205,941 (75 %) had received at least one HPV vaccine dose either prior to or during the programme and 153,263 (56 %) of all females in the age group had received all three doses, table 1.
Uptake by country of birth
During the programme, Danish-born females with both parents Danish-born had the highest HPV1 uptake, 80%, followed by Danish-born with one Danish parent, 76%, and Danish-born with both parents of foreign descent (descendants), 66%. The lowest HPV1 uptake was seen among immigrants, 39%. These results are consistent with those seen prior to the temporary programme where first dose HPV vaccine coverage was 20%, 17%, 6% and 3% for the respective groups.
However, the increase in HPV catch-up programme initiation was most marked among descendants and immigrants; with the introduction of the free-of-charge programme, there was a 12-fold increase between the uptake prior to and during the programme among descendants, and an 11-fold increase in uptake among immigrants. In comparison, we observed a four-fold increase for Danish-born females with both parents Danish-born, while there was a five-fold increase among Danish-born with one Danish parent.
The coverage of HPV1 including vaccines given prior to the programme and during the programme was 84% for Danish-born females with both parents Danish-born, 80% for Danish-born females with one Danish parent, 68% for descendants and 41% for immigrants, while the coverage of HPV3 was 63%, 58%, 46% and 27% for the respective groups, table 1.
The effect of years lived in Denmark among immigrants
The number of years lived in Denmark among immigrants had a strong influence on HPV vaccination uptake. For example, immigrants who had spent 10-15 years in Denmark had a 5.5-fold (Odds Ratio adjusted= 5.5; 95% CI: 5.1-6.0) higher chance of vaccination than immigrants who had stayed less than 5 years.
Comments
The launch of the temporary free-of-charge HPV vaccination programme was well accepted, with an increase in the HPV1 coverage from 17% to 75%. The increase was most pronounced among descendants and immigrants. However, among immigrants, the HPV1 coverage had a low starting point, 3%, and remained relatively low by the end of the programme at 41% in comparison to 68% for descendants and 84% for Danish-born females with two Danish-born parents.
Vaccination programmes are better able to control vaccine preventable diseases if groups with low uptake are targeted. In light of the results, immigrants who have recently moved to Denmark may represent a population that is hard to reach. Immigrants – especially those new to Denmark – may be unfamiliar with the Danish healthcare system and may face a possible language barrier in the access to medical services. Furthermore, ethno-cultural aspects may play a role in forming decisions about HPV vaccination.
Since ethnic minorities in Denmark form a significant part of the population (one fifth of the cohort studied), extra efforts are necessary to reach this group in future vaccination campaigns. Addressing the described issues prior to future campaigns may contribute to increase equity in HPV vaccine uptake between Danish-born and immigrant populations.
(V. Fernández de Casadevante, J. Gil Cuesta, P. Valentiner-Branth Infectious Disease Epidemiology, Statens Serum Institut. L. Cantarero-Arévalo, Department of Pharmacy, Section for Social and Clinical Pharmacy, Faculty of Health and Medical Sciences, University of Copenhagen)
European HIV Testing Week 21-28 November 2014 – Talk HIV. Test HIV.
This week sees the launch of the second European HIV Testing Week, with the theme "Talk HIV. Test HIV".
The objective of European HIV Testing Week is to raise awareness of HIV and not least to draw attention to the advantages of being tested so that treatment may be initiated early.
It has been demonstrated that the sooner you start treatment for HIV, the better are your chances of maintaining good health, and the risk of passing the disease on to others decreases.
Today, at least one in three of the 2.3 million people who live with HIV in Europe are unaware that they are HIV positive. Also, 50% are diagnosed late, which delays their access to treatment.
To change this picture, this week more than 650 NGOs, hospitals and clinics from all of Europe unite to have more people tested for HIV. Participants in the HIV testing week offer HIV testing, communicate the benefits of HIV testing and early treatment and strive to increase awareness of HIV testing among European policy makers.
The European HIV Testing Week is coordinated by HIV in Europe, which is located with CHIP under the Copenhagen University Hospital (Rigshospitalet), Clinic for Infectious Medicine and Rheumatology. CHIP can be contacted at hie.rigshospitalet@regionh.dk or tina.bruun.01@regionh.dk (phone: +45 35 45 57 93).
To sign up for the initiative, go to the website, where you may also find more information and material.
(S. Cowan, Department of Infectious Disease Epidemiology)
Link to previous issues of EPI-NEWS
19 November 2014