No 19 - 2014
Increase in the number of reported MERS-CoV infections, April 2014
Boold donor screening 2013
Increase in the number of reported MERS-CoV infections, April 2014
Since September 2012, when a new coronavirus (Middle East Respiratory Syndrome Coronavirus, MERS-CoV) was initially identified, the WHO has reported a slowly increasing number of cases, primarily from the Arabian Peninsula. In the period from March 2013 to March 2014, an average of 15 monthly cases were detected. In April 2014, a substantial increase in the number (261 new cases) was reported.
The increase was primarily observed in Saudi Arabia and the United Arab Emirates, among others in relation to hospitals, and a growing share of secondary cases was seen among contacts to infected patients, healthcare staff as well as relatives who had been caring for sick patients.
This may indicate an increase in person-to-person transmission, but it may also be due to other conditions including insufficient precautions to avoid transmission at the hospitals in question or increased awareness. Only few non-hospital outbreaks have been observed, and the overall assessment remains that the new coronavirus is not particularly infectious.
As per 7 May 2014, a total of 495 confirmed cases of MERS-CoV have been reported to the WHO, of which 141 were fatalities, corresponding to a 28% mortality.
The majority of the cases of new coronavirus infection were diagnosed in Saudi Arabia (411 cases, including 248 since 1 April 2014) and the United Arab Emirates (49 cases, including 32 since 1 April 2014), but cases have also been seen in Qatar, Jordan, Oman and Kuwait. Furthermore, individual cases were diagnosed in the United Kingdom, France, Italy, Tunisia, Germany, Greece, Egypt, Malaysia, the Philippines and the USA, mainly among persons with previous stays on the Arabian Peninsula.
In Denmark, 14 persons have been tested for MERS-CoV to date, none of whom have tested positive; instead, other airway viruses were shown to be the cause of their symptoms.
In the initial phases of the outbreak, the reported cases showed an excess of elderly men, nearly all had underlying disease and the mortality was 60%. Only a limited share of the primary cases had any known contact to animals.
As the outbreak has progressed, more and more cases have been detected owing to contact tracing, which has changed the epidemiological picture. Now, more asymptomatic or mildly symptomatic cases are being reported among otherwise healthy younger persons, including female healthcare professionals.
About coronavirus and MERS-CoV
Coronaviruses are a family of RNA viruses found in birds and mammals. Members of the coronavirus family are a common cause of cold, but may also — in rare cases — cause lower respiratory airway infections. There are several groups of coronavirus, and the virus causing the 2003 SARS epidemic was a special variant. The new MERS coronavirus belongs to the same group as SARS, but the two are genetically different.
Coronavirus is transmitted by direct contact or through droplet spreading in connection with sneezes and or/coughing. Coronavirus is also excreted to faeces, which is therefore also a source of infection. The sources and routes of infection for MERS-CoV have not presently been fully established, but the incubation period is presumably 7-10 days, possibly up to 14 days.
Preliminary analyses show that MERS-CoV is genetically similar to coronaviruses that occur in bats, and MERS-CoV has been isolated from a single bat. Considerable genetic variation has been observed in MERS-CoV isolated from patients, indicating that several virus introductions have occurred, probably via infected animals.
A large proportion of Middle Eastern dromedaries carry antibodies to MERS-CoV, but this is not the case for other animals such as goats and sheep. MERS-CoV also seems to be capable of binding effectively to cells in the airways of humans, horses and dromedaries – and less effectively to cells in the airways of goats and bats.
MERS-CoV has recently been confirmed by PCR in the airways of dromedaries in screening studies and also in connection with outbreak investigations of human cases. There is, then, growing evidence to support that dromedaries are a source of MERS-CoV infection.
Risk of infection and prophylaxis
The risk of infection for travellers to the Arabian Peninsula and the neighbouring countries is still considered very limited. Travellers should observe standard hygiene advice, including:
- maintaining good hand and other personal hygiene
- ensuring good food hygiene (avoiding insufficient frying/roasting of meat and avoiding unpasteurised milk - particularly from dromedaries)
- avoiding close contact to animals, particularly to dromedaries. This applies in particular to animal excretions such as saliva and faeces
- avoiding close contact to persons presenting with acute symptoms from the airways (coughing and sputum production) and to persons with diarrhoea.
Diagnostics and notification
Patients should be tested for coronavirus if they suffer from acute respiratory infection or have another serious infection in conjunction with an underlying chronic disease (immunosuppression), and have stayed on the Arabian Peninsula or in any neighbouring countries in the last 14 days leading up to symptom onset.
Before samples are submitted, the indication should be discussed with the virologist (daytime) on call or with the infectious disease epidemiologist (outside normal working hours). If there is indication to test for MERS-CoV, nasal and throat samples, tracheal secretion, expectorate and other microbiological samples are submitted to the SSI; see instructions for urgent submission of samples at www.ssi.dk. To exclude MERS-CoV, sampling material from the lower airways is also needed. Suspected MERS-CoV cases are notifiable to the Medical Officer of Health.
Commentary
Initially, the MERS-CoV outbreak attracted considerable attention with international health authorities as its mortality was high, and it was feared that the new virus would cause a SARS-like epidemic. Over a period of few months in 2003, the SARS-virus, which was also a coronavirus, rapidly spread to several continents causing 8,000 cases of which 800 were fatalities, including several among healthcare staff.
It was quickly established, though, that MERS-CoV was less infectious than SARS and that elderly persons with an underlying disease had a greater risk of suffering a severe disease course.
The cause explaining the substantial increase in the number of reported MERS-CoV cases in April remains unclear, but the situation is followed closely. Recently, growing evidence has appeared to support that dromedaries are a source of MERS-CoV infection.
The WHO has dispatched a team of experts to Saudi Arabia to assist the national health authorities in establishing if there are signs of an increase in person-to-person transmission and to perform serological studies to establish the scope of such transmission. The WHO has also designed and proposed an international epidemiological case-control study to establish the primary cases’ exposure and risk behaviour.
It is still assessed that MERS-CoV is not particularly infectious and no travel or trade restrictions have been imposed on the affected countries on the Arabian Peninsula, but travellers to the area should observe standard hygiene advice as mentioned above.
(T.G. Krause, P.H. Andersen, Department of Infectious Disease Epidemiology, A. Fomsgaard, Virus Research and Development)
Blood donor screening 2013
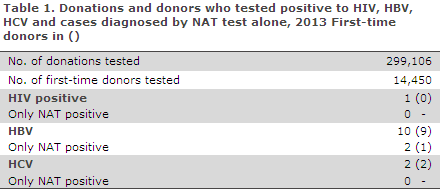
In 2013, a total of 299,106 blood units were screened and 14,450 first-time donors were tested. The number of positive donors is presented in Table 1.
NAT screening (nucleic acid amplification technique) of donor blood for HIV, hepatitis B and C virus (HBV and HCV) was introduced by law on 1 January 2009, EPI-NEWS 2/10.
HIV
One multiple donor tested positive to HIV. The donor is believed to have been infected through heterosexual contact abroad. At the latest donation session a year ago the blood drawn was not donated and therefore look back has not been performed
Hepatitis B virus
In 2013, a total of nine male first-time donors tested positive to HBV. Their median age was 38 years (range 20-53 years). One was detected by NAT screening only.
Seven persons were born in an endemic area or by a mother from an endemic area, one had had a tattoo and piercing performed, and for one person the mode of infection was unknown.
Additionally, one multiple donor tested positive to HBV by NAT screening alone. The donor had a chronic hepatitis B infection with no detectable HBsAg, a so-called occult hepatitis B infection.
Hepatitis C virus
In 2013, two women first-time donors aged 39 and 42 years, respectively, tested positive to HCV. One was presumably infected when being tattooed abroad, the other probably through IV drug use.
Commentary
In 2013, the number of donors who tested positive to the three virus markers remained low.
One multiple donor tested positive to HIV, but as the donor's last unit of blood had not been used for donation, there was no risk of infection.
One donor was NAT positive only to HBV and he would therefore not have been detected by the donor-screening scheme if NAT screening had not been introduced. Expectedly, some donors will test positive to antibodies to hepatitis B core antigen as they undergo testing, EPI-NEWS 18/13.
Such donors will be excluded from making donations in future, but there are no plans to perform look back on the large number of blood donations made over the years.
(A.H. Christiansen, S. Cowan, Department of Infectious Disease Epidemiology, L. Harritshøj, H. Ullum, Department of Clinical Immunology, Copenhagen University Hospital (Rigshospitalet)
Link to previous issues of EPI-NEWS
7 May 2014