No 10 - 2014
Diarrhoeagenic E. Coli 2000-2012
Prevention of hepatitis A - advice and guidance collected in a new guideline
Diarrhoeagenic E. coli 2000-2012
Diarrhoeagenic E. coli (DEC) are divided into main groups on the basis of the clinical picture they cause, and they are characterised by different virulence factors.
The best known is probably verocytotoxin-producing E. coli (VTEC) which has caused multiple outbreaks, Table 3. VTEC produces one or two verocytotoxins (VT1 and/or VT2) and causes gastroenteritis, often with bloody diarrhoea. The most serious complication of VTEC is haemolytic uraemic syndrome (HUS). Due to the risk of severe complications, VTEC — as the only DEC — along with HUS cases are individually notifiable on Form 1515. In addition to VTEC, another five DEC groups have been defined. Each group is described below.
- Intimin-producing E. coli (attaching and effacing E. coli, A/EEC) are positive to the eae gene that codes for intimin, which is associated with destruction of the intestinal epithelial cells in what is known as the "attaching and effacing lesion". The intimin-producing E. coli form a very heterogeneous group which cannot be unequivocally established as a cause of diarrhoea. In cases in which no other aetiology is established, the finding of intimin-producing E. coli is considered a possible cause of diarrhoea.
- Enteropathogenic E. coli (EPEC) is a subgroup of the intimin-producing E. coli. This subgroup is defined on the basis of its specific O:H serotypes which fall within the following 11 O groups: O26, O55, O86, O114, O119, O111, O125, O127, O128, O142 and O158. Contrary to the broader concept of intimin-producing E. coli, EPEC are indeed diarrhoeagenic and a classic cause of diarrhoea in smaller children. Three O groups known from VTEC, i.e. 0103, O145 and O157, are also observed as EPEC.
- Enterotoxigenic E. coli (ETEC) form the enterotoxins LT and/or ST. LT is heat-labile and nearly identical to cholera toxin, whereas ST is heat-labile and occurs in two variants. In order to cause an infection in humans, ETEC needs to express attachment factors specific to intestinal epithelial cells in humans. ETEC isolated from animals therefore does not cause illness in humans. ETEC is a very common cause of diarrhoea among children in developing countries, and in Denmark these infections are most frequently seen in connection with foreign travel. More rarely, they may cause food-borne infections, often in connection with vegetables imported from exotic countries.
- Eteroinvasive E. coli (EIEC) invade the epithelial cells of the large intestine in the same manner as Shigella does and are clinically indistinguishable from Shigella species.
- Enteroaggregative E.coli (EAggEC) are characterised by a specific attachment pattern in a cell assay . Enteroaggregative E. coli may be a cause of bloody or prolonged diarrhoea
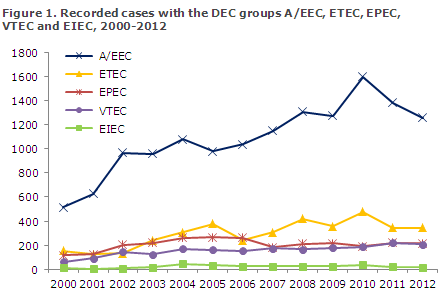
General development
The number of recorded DEC cases has increased steadily as the use of routine diagnostics has gained a stronger foothold, starting in 1997. Including the intimin-producing E. coli, DEC has thus been the second-most frequently occurring pathogenic intestinal bacterium group, following Campylobacter, since 2003. In the 2003-2012 period, an average of 1,201 annual cases of intimin-producing E. coli were recorded, 341 ETEC cases, 225 EPEC cases, 175 VTEC cases and 28 EIEC cases, Figure 1. EAggEC was not included as they were not included in the routine diagnostics of intestinal bacteria in this period.
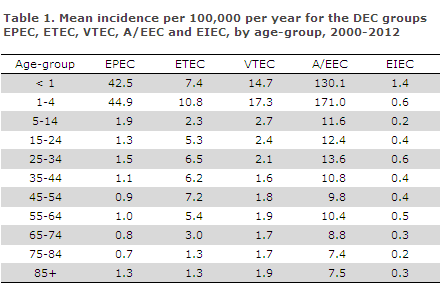
The mean incidence varied between the various DEC groups according to age, Table 1.
The mean incidence varied between the various country areas. For EPEC, ETEC and VTEC, the incidence was highest on Funen and in North Zealand, Table 2.
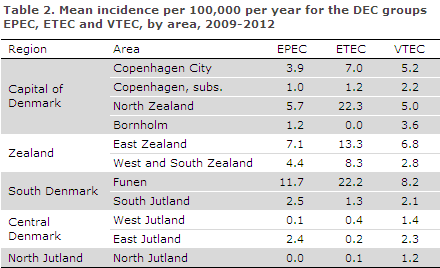
The different referral criteria applied throughout Denmark may be one explanation for the differences observed between the various parts of Denmark. Thus, in 2012 the Department of Clinical Microbiology at Odense University Hospital introduced a practice according to which all stool samples were tested for DEC. In 2012, the incidence for the three commonly occurring DEC groups in the area of Funen was 12.2 per 100,000 for EPEC; the mean incidence for the remaining parts of Denmark was 2.7. For ETEC in the area of Funen, the incidence was 24.3 per 100,000; the mean incidence for the remaining parts of Denmark was 3.3. For VTEC in the area of Funen, the incidence was 10.5 per 100,000; the mean incidence for the remaining parts of Denmark was 3. Extrapolation of these numbers to the remaining parts of the country yields a calculated number of possible extra cases in 2012 of slightly above 450 for EPEC, approx. 1050 for ETEC and nearly 400 for VTEC.
The most common EPEC and VTEC O groups are O26, O103, O111, O128, O145 and O157. The groups O55, O119 and O125 are nearly only found in EPEC bacteria; and O91, O104, O117 and O146 are most frequently observed in VTEC bacteria. Nearly all cases of O117 and O104 are acquired via foreign travel, Figures 2 and 3.
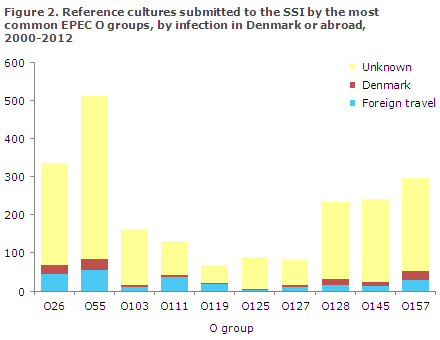
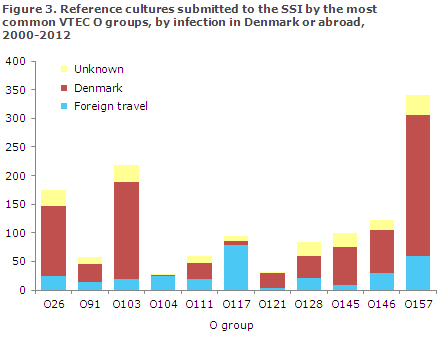
As presented in Figures 2 and 3, the majority of VTEC infections - barring VTEC O117 - are acquired in Denmark, whereas information on foreign travel is lacking for most EPEC infections.
Outbreaks
Since 2003, the SSI has recorded a total of 11 DEC outbreaks. Eight of these were food-related. Furthermore, DEC was detected in two outbreaks caused by contaminated drinking water, Table 3.
In February of 2012, four persons were infected with sorbitol-fermenting O157:H- (SF O157:H-) which is an aggressive subtype of O157. HUS was seen in two of these persons. In the autumn of 2012, Denmark recorded its first general food-related outbreak with HUS cases caused by VTEC O157:H7. The source of the outbreak was probably contaminated minced meat, EPI-NEWS 45/12.
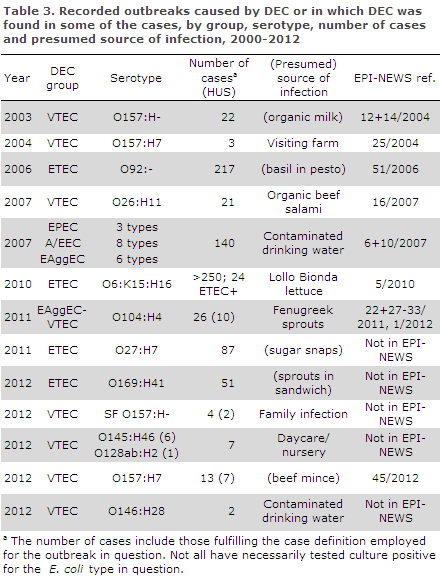
In addition to the cases presented in the table, three persons were infected with the same VTEC O145:H- in 2012 without this leading to an actual outbreak investigation.
Commentary
Presumably, the increase in DEC diagnosing in the period is primarily due to increased diagnostic activity. We assess that differences in incidence between areas are primarily caused by differences in diagnostic practices, i.e. referral criteria and choice of methods.
As described above, a practice in which all stool samples were tested for DEC would lead to a calculated extra number of DEC cases in the order of 1,900 in 2012 for the three DEC groups.
The Danish Society of Clinical Microbiology (DSCM) and Statens Serum Institut recommend that all patients below the age of seven years with diarrhoea, patients with diarrhoea associated with foreign travel and patients with bloody diarrhoea — regardless of their age — be tested for DEC using molecular biology diagnostics. It is important that the person submitting the samples state the clinical information on any bloody diarrhoea and recent foreign travel, and any suspicion of food-related infection so that infection tracing may be initiated early and secondary infection may be prevented.
The recorded ETEC outbreaks were exclusively found owing to extraordinary submission of Danish acquired ETEC isolates from individual departments of clinical microbiology or in connection with notification of suspicion of food-related outbreaks and subsequent typing of the submitted isolates. Note that in all of the outbreaks, barring the O157 outbreak in 2012, the possible sources are foods that are not normally heat-treated. In the remaining outbreaks, contact infection (person-to-person or contact with infected animals) is the most likely source.
(F. Scheutz, WHO Collaborating Centre for Reference and Research on Escherichia and Klebsiella, Department of Microbiology and Infection Control, L. Espenhain, S. Ethelberg, C. Kjelsø, K. Mølbak, Department of Infectious Disease Epidemiology, K.E.P. Olsen, A.M. Petersen, Department of Microbiology and Infection Control, B. Olesen, Herlev Hospital, J. Engberg, Slagelse Hospital, H. Holt, Odense University Hospital, A. Friis-Møller, Hvidovre Hospital, L. Lemming, Aarhus University Hospital, F. Schønning Rosenvinge, Vejle Hospital, J. Prag, Viborg Hospital, T. Ejlertsen Jensen, Aalborg University Hospital, M. Tvede, Copenhagen University Hospital (Rigshospitalet), P. Kjældgaard, Sønderborg Hospital)
Prevention of hepatitis A - advice and guidance collected in a new guideline
The Danish Health and Medicines Authority has updated the guideline on hepatitis A (her indsættes nedenstående link) so that all information on preventive measures against infection during travels, at home and in institutions is now available in a single publication.
The guideline includes measures to avoid infection in homes and other places where several people share housing, and it provides instructions for good hygiene in daycare and homecare facilities. The guideline also brings changes. Thus, the use of passive immunisation in the form of immunoglobulin is no longer as widely recommended as was previously the case.
Several effective hepatitis A vaccines are being marketed and the guideline presents their posology and degree of protection and the precautions relating to pregnant women. Specific recommendations are provided regarding which groups of persons should receive preventive treatment (prophylaxis) before or after exposure to infection risk at home, in institutions, at work and during travels. The guideline also stipulates what should be done in case of a single case of infection and in case of a hepatitis A outbreak in daycare institutions. That is if infection spreading has been established within the institution.
The target group of the guideline is hospitals, the practice sector, medical officers of health and the municipal health service and administrators as well as employees and employers in professions at risk of infection.
(Danish Health and Medicines Authority)
Link to previous issues of EPI-NEWS
5 March 2014