No 19 - 2013
Invasive pneumococcal disease and PCV coverage 2012
Invasive pneumococcal disease and PCV coverage 2012
More than five years have passed since the first conjugated pneumococcal vaccine (PCV) was introduced into the Danish Childhood Vaccination Programme at three, five and 12 months of age.
The 7-valent vaccine (PCV-7) was used from 1 October 2007 to the end of 2010. The 13-valent conjugate pneumococcal vaccine (PCV-13) was gradually introduced as from Week 16 of 2010. The PCV-7 was thus phased-out in the course of 2010, and 2011 was the first year in which only PCV-13 was administered.
Laboratory monitoring data preceding the introduction of PCV-7 demonstrated that 64% of all cases of invasive pneumococcal disease (IPD) in children up to five years of age were caused by pneumococcal serotypes included in the PCV-7 (4, 6B, 9V, 14, 18C, 19F og 23F), and that 91% of IPD cases in the same age group were caused by serotypes included in the PCV-13 (the PCV-7 serotypes plus serotypes 1, 3, 5, 6A, 7F and 19A), EPI-NEWS 37 a+b /07.
Following the introduction of PCV-7, the incidence of IPD in small children was halved within a year. The decline in incidence was closely associated with a decrease in IPD caused by the serotypes included in the vaccine.
Vaccination coverage
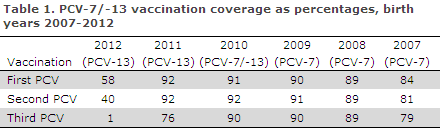
Vaccination coverage was recorded using the administrative service codes indicated by GPs when settling the first, second and third PCV vaccinations, respectively.
Coverage was calculated on the basis of data from the Childhood Vaccination Database as per 10 January 2013. There is a 2-3 month lag from a vaccination is performed until it is recorded in the Childhood Vaccination Database.
Vaccinations administered after mid November 2012 are therefore not included in the above report.
The coverage of the Childhood Vaccination Programme for birth cohorts 2007-2011 was in the range 84-92% for the first PCV, 81-92% for the second PCV and 76-90% for the third PCV, Table 1. For the 2012 birth cohort, vaccination had not been concluded at the calculation date.
Changes in IPD incidence
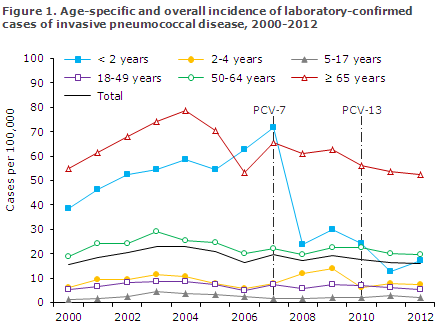
Figure 1 shows the age-specific incidence of laboratory-confirmed IPD cases per 100,000 inhabitants before and after the introduction of PCV-7 and PCV-13 into the Childhood Vaccination Programme.
The report is based on national Danish data from the Neisseria and Streptococcal Reference Laboratory, Statens Serum Institut (SSI). An IPD case is defined as a disease episode for which pneumococci, Streptococcus pneumoniae, have been cultured in cerebrospinal fluid, blood or another normal, sterile sampling material.
As from 1 October 2007, submission of pneumococcal isolates from IPD patients to the SSI has been required by law for monitoring purposes, including serotyping.
In a limited number of cases every year, diagnosis is not made by culture, but only by PCR, why serotyping is not possible.
The overall incidence in the population of IPD prior to the introduction of PCV, defined as the mean annual incidence during the eight-year period from 2000 to 2007, was approx. 20 cases/100,000 (a mean 1,056 annual cases).
The incidence has been reduced significantly by approx. 20%, which is equivalent to 16 cases/100,000 (864 cases) in 2012.
The strongest decline in the IPD incidence was observed in children < 2 years of age: from a mean incidence in the eight-year period from 2000 to 2007 of 54 cases/100,000 annually to approx. 17 cases/100,000 in 2012.
The 2012 incidence represents a minor increase relative to 2011, when the incidence was slightly below 13/100,000. The average annual number of cases of pneumococcal meningitis in children below five years of age decreased from 19 annual cases in the period from 2000 to 2007 before the introduction of PCV to six in 2012.
For IPD caused by the serotypes included in the PCV-7, the incidence in the < 2 years age group decreased from approx. 36/100,000 cases before PCV to less than one case per 100,000 in 2011, and the incidence has subsequently decreased further, as no cases were observed in 2012.
For the six extra serotypes included in the PCV-13, the incidence has decreased from approx. 13 cases/100,000 annually before the introduction of PCV to around 2/100,000 annually in 2012.
The incidence of the so-called non-vaccine serotypes (not included in the PCV-7 or the PCV-13) has, however, increased from an annual 5-6 cases per 100,000 before PCV to approx. 15/100,000 in 2012.
Among persons above 65 years of age, the overwhelming majority of whom may be considered unvaccinated, a significant decrease in IPD incidence has been observed from approx. 66 cases/100,000 in the eight-year period from 2000 to 2007 before the introduction of PCV into the Childhood Vaccination Programme to approx. 53/100,000 in 2012.
This decrease is mainly owed to a reduction in the serotypes included in the PCV-7, whereas a similar effect has yet to be observed for the six extra serotypes included in the PCV-13.
The observed decrease in incidence among unvaccinated persons, the so-called herd effect, is presumably achieved because PCV reduces the ability of children vaccinated for the serotypes comprised by PCV to serve as carriers and thereby reduces the circulation of vaccine serotypes in the population.
Commentary
Five years after the PCV-7 was introduced, PCV-7 serotypes are hardly ever observed in IPD isolates from small children in Denmark. PCV-13 has had a similar effect on the six extra serotypes. However, the data showing this were analysed after a relatively short monitoring period.
This is important to keep in mind as the distribution of pneumococcal serotypes is characterized by natural variation which is unrelated to vaccination.
Data from 2012, however, do show an increased occurrence of non-vaccine serotypes in children < 2 years causing a moderate increase in IPD incidence for this age group.
The increase does not outweigh the overall positive effect of the vaccine.
The PCV coverage is approximately one to two percentage points lower than that of the DTaPIPV/Hib vaccine which is given concurrently.
The reason for this difference is unknown, but the overall coverage is in line with that observed in previous years, EPI-NEWS 21/12.
(P. Valentiner-Branth, C.H. Suppli, P.H. Andersen, Department of Infectious Disease Epidemiology, S. Hoffmann, T. Dalby, H.C. Slotved, H.B. Konradsen, Z.B. Harboe, Microbiology and Infection Control)
Link to previous issues of EPI-NEWS
8 May 2013